Although many patients with bipolar depression remain symptomatic despite the use of mood stabilizers, the effectiveness and risk of adding an antidepressant to their medication regimen remains controversial. A study in the September American Journal of Psychiatry adds weight to the opinion that, at least for a subpopulation of patients who have simultaneous manic symptoms and full-blown depression, adjunctive antidepressants provide few benefits and may even exacerbate mania.
The study was based on the naturalistic treatments and patient outcomes collected in the nonintervention phase of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) study, in which practitioners were given no particular guidelines regarding adjunctive antidepressants. Specifically, the researchers investigated whether antidepressants plus standard mood stabilizers succeeded in bringing patients out of a depressive episode faster than mood stabilizers alone.
STEP-BD, which was funded by the National Institute of Mental Health and conducted between 1998 and 2005, is the largest national research program on the treatment of patients with bipolar disorder. It sought to clarify treatment effectiveness and patients' disease course and outcomes in real-life clinical settings. The study design included both naturalistic treatment components and randomized, controlled, interventional treatments. (See related article
Psychosocial Benefits Accrue When Psychotherapy Part of Treatment.)
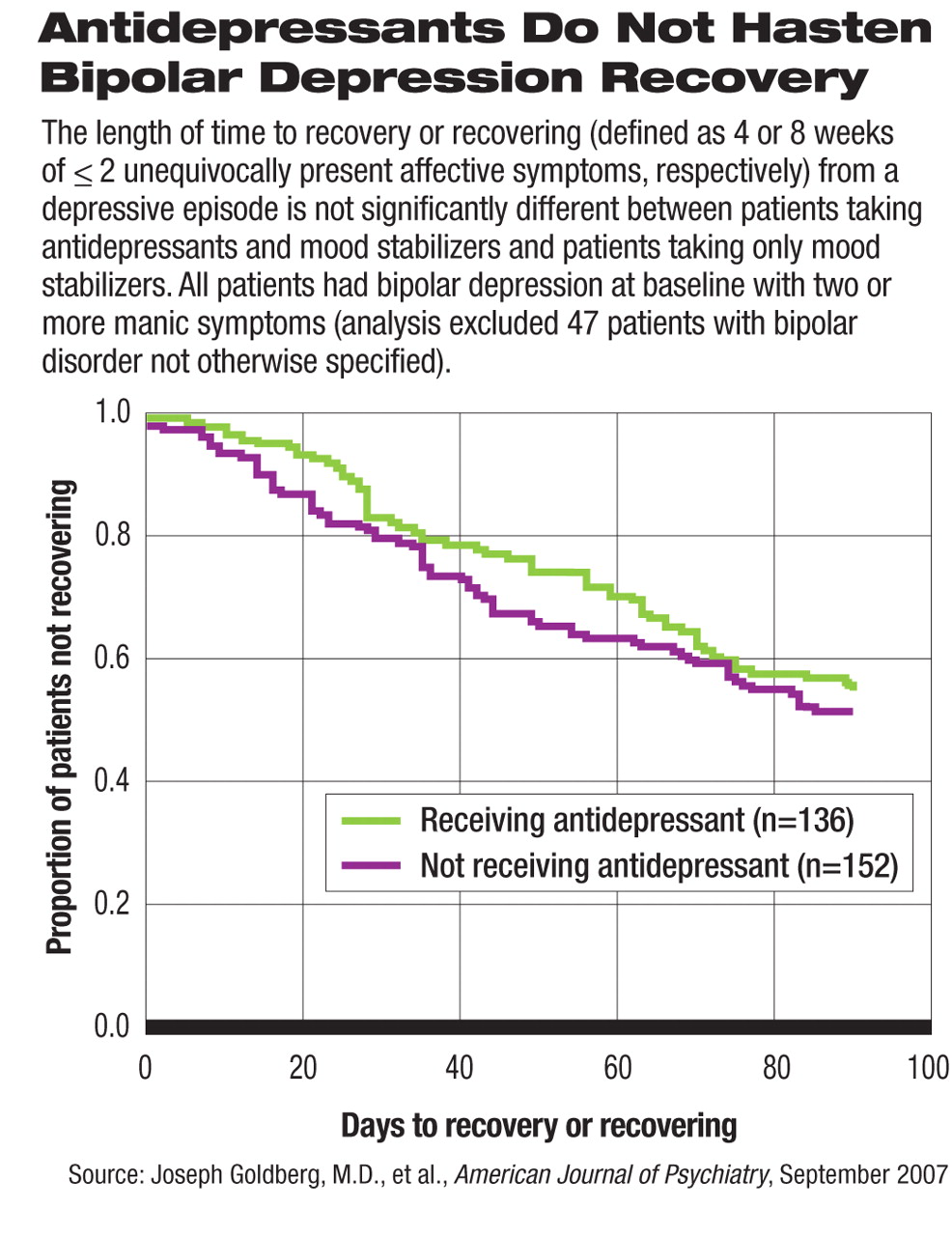
Among the first 2,000 patients enrolled in the naturalistic phase of STEP-BD, the authors chose a subgroup of 335 patients taking mood stabilizers who met the DSM-IV criteria for a full depressive episode while also having two or more manic symptoms. Patients with depression and subsyndromal mania were included because they were more likely to be prescribed an antidepressant than those who met the diagnosis of mixed episode, the authors said. About half of the patients in the subgroup (145) were treated with an adjunctive antidepressant before or at the time of enrollment; the remainder were not.
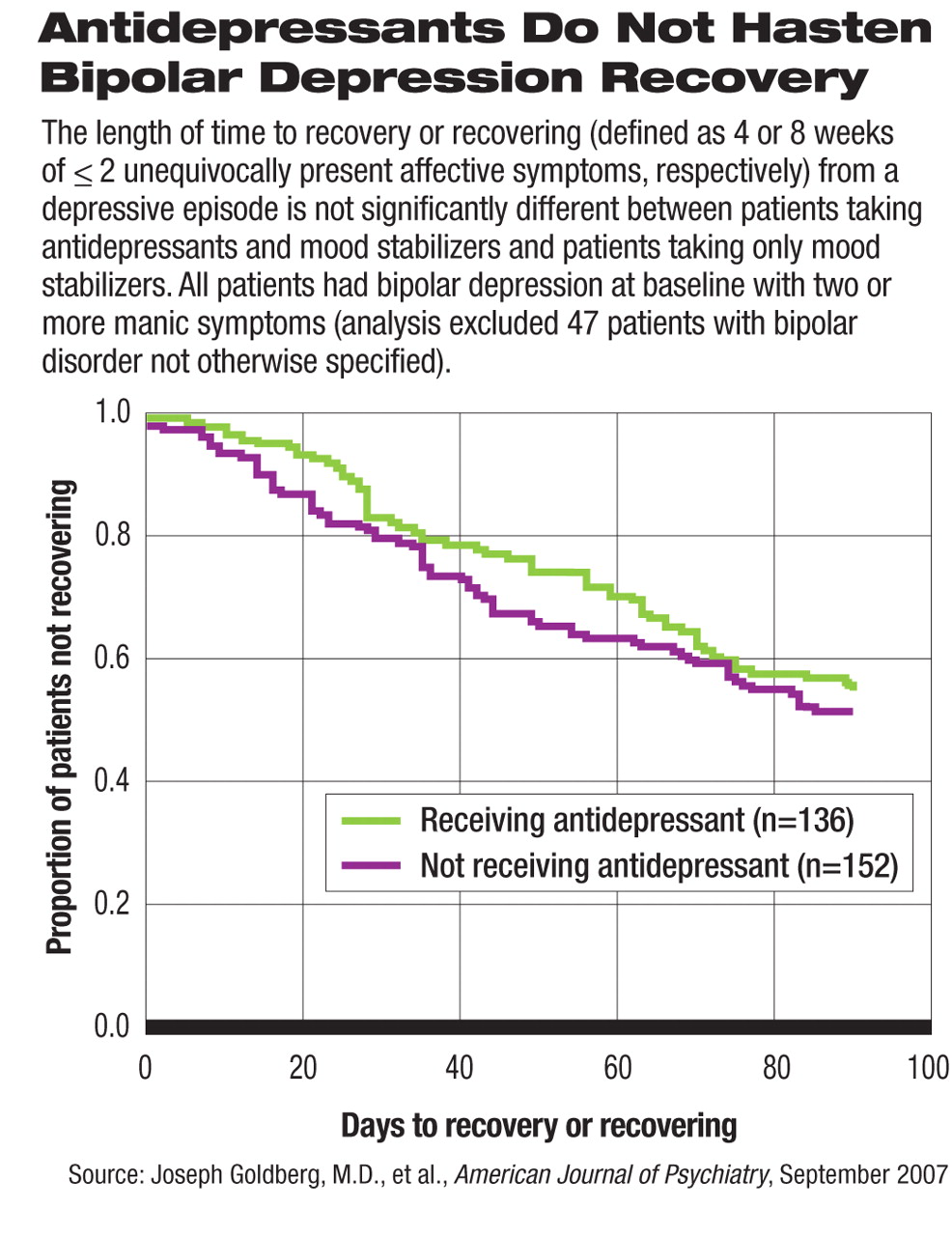
The time to recovering (defined as four weeks of two or fewer unequivocally present affective symptoms) or recovery (eight weeks of two or fewer affective symptoms) was not significantly different between patients taking an antidepressant with a mood stabilizer and those taking a mood stabilizer only. In other words, the addition of an antidepressant did not hasten patient recovery from a depressive episode.
The authors then expanded their analysis to a total of 445 patients with bipolar depression and any number of manic symptoms at baseline as well as those with no manic symptoms. For those who had one or more manic symptoms at baseline, adding an antidepressant was significantly associated with increased severity of mania (measured by the Young Mania Rating Scale) at the three-month follow-up visit.
STEP-BD researchers led by Gary Sachs, M.D., of the Department of Psychiatry at the Massachusetts General Hospital/Harvard University Medical School had found in another study that giving antidepressants to patients who had bipolar depression but no concomitant manic symptoms and were already on mood stabilizers increased neither the percentage of patients who achieved recovery nor their risk of switching to mania, compared with patients taking only mood stabilizers (New England Journal of Medicine, April 26).
That study “found that antidepressants neither help nor harm these bipolar patients in a more 'pure' depressive episode who had no manic symptoms. Our study looked at a different group of patients with depression plus manic symptoms,” said Joseph Goldberg, M.D., the lead author of the current American Journal of Psychiatry study and director of the Affective Disorders Program at Silver Hill Hospital in New Canaan, Conn., in an interview with Psychiatric News.
“In previously collected data, we had found that about half of patients with bipolar depression had subsyndromal mania that does not meet the DSM-IV definition of a mixed episode, while only a third had 'pure' depression without manic symptoms.” These data were presented at APA's 2007 annual meeting.
Despite the lack of evidence clearly supporting their advantages, antidepressants are widely prescribed to bipolar patients experiencing a depressive episode, as Ross Baldessarini, M.D., and colleagues reported in the January Psychiatric Services. This finding may reflect the difficulty in detecting manic symptoms when depression is the predominant feature.
In addition, long-term observational data published by Lewis Judd, M.D., of the Department of Psychiatry at the University of California, San Diego, and colleagues in the Archives of General Psychiatry (June 2002 and December 2005) have shown that depressive episodes and symptoms consume a much larger portion of patients' lives and cause more disability and mortality than do manic symptoms.
Goldberg and colleagues pointed out in their article that“ practitioners often fail to recognize manic symptoms during bipolar mixed states” or “underappreciate manic or hypomanic symptoms” during depressive episodes. They suggested that psychiatrists should be more vigilant in detecting signs of mania during a depressive episode that are below the threshold of DSM-IV-defined mixed episodes.
Even if a patient is clearly experiencing a depressive episode, the clinician “should be conscientious of any concomitant manic symptoms,” Goldberg recommended. “One should be very cautious with the use of antidepressants in these patients.”