Nineteenth-century architecture for the insane produced grand palaces of healing, ex pressing in brick and stone the enlightened therapeutic ideals of their age. They were paradoxical structures: massive, but allowing patients to view the natural world outside. Light, air, decent accommodations, useful work, and kindly staff were supposed to help patients recover or remain in compassionate care (Psychiatric News, September 2, 2005).
Of course, that idealized marriage of design and psychiatry did not last.
New policies led to overcrowding and mere custodial care of public patients by the late 1800s. Still later, shock at those conditions and the development of psychotropic drugs in the mid-20th century led to an emphasis on community care and deinstitutionalization. The number of patients in state and county mental hospitals declined from 337,691 in 1970 to 49,443 in 2002, and the number of hospitals decreased from 315 to 232, according to the most recent data from the National Association of State Mental Health Program Directors.
Yet the need for psychiatric hospitals has not disappeared. Public or private, they still offer long-term care for the most difficult cases and provide short- to medium-term settings for diagnosis and treatment. At least 11 states are now in the process of replacing older hospitals or building new ones. Some private facilities, such as the Sheppard and Enoch Pratt Hospital in Towson, Md., have also constructed new wings in recent years.
As they build, however, the people who design and run psychiatric facilities still put their ideas of how to care for patients into the very walls of their buildings. Over the last two decades, the design of new psychiatric hospitals and new psychiatric wings of general hospitals reflects the emphasis on recovery, shorter stays, and the patients' role in their treatment. Today's facilities still have their boundaries but, more than ever before, are less places of confinement and more places of treatment and preparation for return to the outside world.
“A psychiatric hospital should recapitulate a real community in which patients will live after treatment,” said Richard Lippincott, M.D., a professor of psychiatry at the University of Arkansas for Medical Sciences, articulating the views of many architects and mental health professionals.“ You make the inside represent the community outside.”
Lippincott was formerly director of New Hampshire's Department of Mental Health and Developmental Services and managed the creation of the New Hampshire Psychiatric Hospital in Concord, which opened in 1988. The new building was constructed, like others, around a central courtyard and includes a shop, gym, library, and dining hall for residents, staff, and visitors.
The dining room provided an especially vivid example of how design had altered social patterns in the hospital, said Lippincott. The space became a crossroads for more than patients and staff. Families met with their hospitalized relatives there. Previously discharged patients found the atmosphere so congenial that they returned for meals. Legislators from the nearby state house would even drop in for lunch. While this setting was open and friendly, access was also closely controlled, with only one way in or out of the room.
One state over, the Riverview Psychiatric Center in Augusta, Maine, which opened in 2004, is also constructed around an enclosed courtyard, so patients can go outside as they wish but still be in a secure setting, said Marya Faust, M.S.W., director of the Office of Adult Mental Health Services for the state. Riverview was designed by JSA Architects Interiors Planners of Portsmouth, N.H.
“The center offers a humane and welcoming environment without compromising security,” said Faust. “The challenge was how to make it look inviting. All rooms are private and have windows that give views to the outside.”
Those windows express the combination of security and patient autonomy guiding the new architecture. Blinds are enclosed between glass panes so that patients can control light entry but not damage the blinds or injure themselves. Building design can also influence staff practices. Two units at Riverview do not have seclusion rooms, so the staff improved their skills in de-escalating potentially violent situations, said Faust.
Light and color fill the interior spaces. Window walls let in the sun, and art, some by professional artists and some by patients, lines the corridors.
“Just being in the building gives one much more hope,” said Faust.
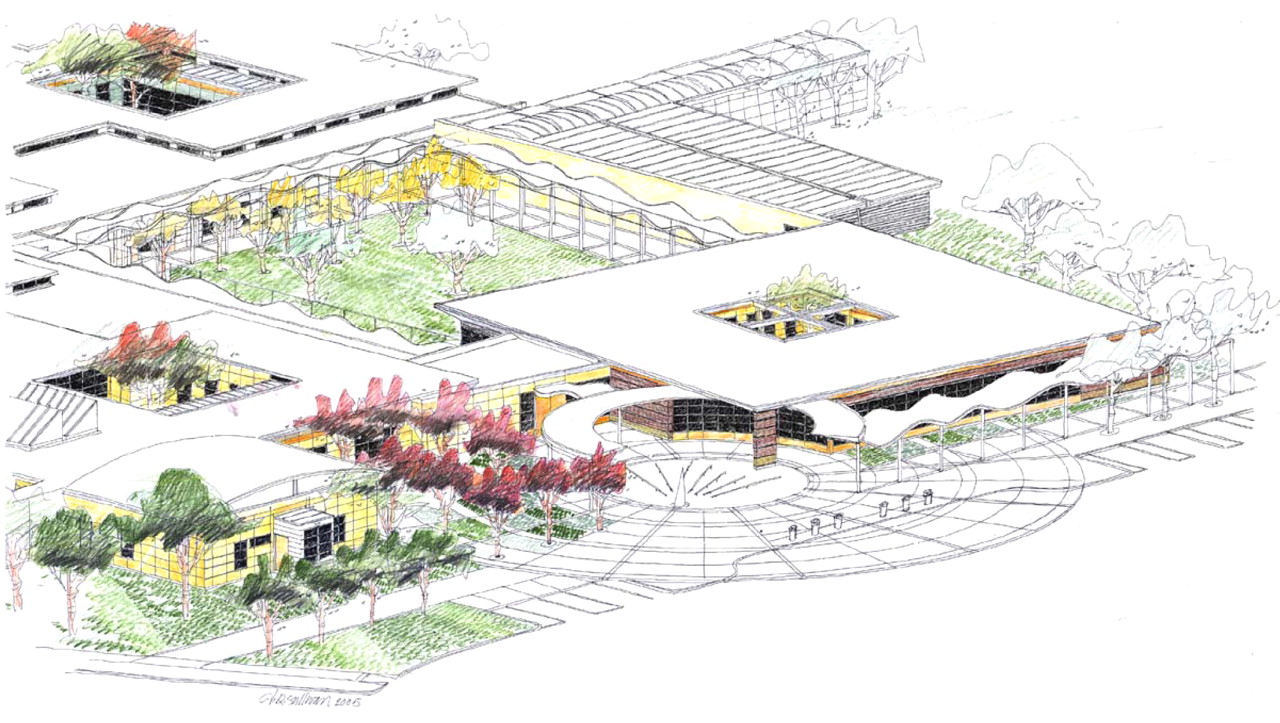
Similar ideas are evident in the plans for a new psychiatric unit that the Department of Veterans Affairs is building on its Palo Alto, Calif., campus. There, subunits cluster around courtyards, and small gardens are built into the ends of each cluster.
Enclosed courtyards are a common theme because they allow patients to move freely into the open air without fear that they will wander away.
Like all the new structures, the VA hospital will provide ample daylight in patient and common rooms. Views of the natural world outside can reduce psychological distress and recovery time and enhance staff functioning, wrote Bradley Karlin, Ph.D., and Robert Zeiss, Ph.D., of the VA in the October 2006 Psychiatric Services. Interior design makes the building feel less like an institution and more like a home—cinder blocks and echoing hallways are out. Furniture must be heavy enough not to be thrown but light enough to move around and create informal social spaces.
“The VA is moving to an interdisciplinary, evidence-based, recovery model of care,” said Karlin, the newly appointed director of psychotherapy programs for the VA's Office of Mental Health Services in Washington, D.C., in an interview. Karlin and Zeiss were part of the design team for the new inpatient psychiatric building. In that process, representatives of all divisions of the hospital were included in early discussions with the architects, Design Partnership of San Francisco.
“Creating these new hospitals is an intense collaborative exercise for both architects and staff members,” said Karlin.
When faced with planning a new building, psychiatrists should talk to each other, visit other facilities, and ask what worked and what didn't, said architect Frank Pitts of architecture+ in Troy, N.Y., in an interview.“ Simply because they are psychiatrists, they should be able to articulate what they see and how they feel about other facilities.”
The image of village—houses, a neighborhood, downtown—underlies the new movement, said Pitts, president of the American College of Health Care Architects and past president of the American Institute of Architects' Academy of Architecture for Health.
The “house,” in this case, is the patient's room, a place of comfort and familiarity, Pitts told Psychiatric News. When ready, the patient can move from the bedroom to a seat just outside the door (the“ neighborhood”), to places farther along the hall, and to more open shared spaces. The “downtown” may include the treatment areas, gift shop, or other common areas. The patient can emerge or retreat, as feelings dictate, while an observant staff can increase or decrease security as needed.
In the traditional rehabilitation model, said Pitts, movement depended on accumulating privileges. In the village model, patients can exercise more responsibility and control of their actions.
“You have to look at patients as individual human beings,” said Pitts. “They have had to leave home and face a lot of stress. You don't want that experience to further destabilize them.”
Early in his career, he said, when he began designing psychiatric facilities, he talked to everyone who would use the building, including patients.
“I would sit quietly on the unit just to see and hear what was going on, or I'd talk one on one with patients,” recalled Pitts. “The most singular thing I found was how frightened patients were about being harmed in the hospital.”
It became important to give them a range of options so that all patients housed on the unit (typically 24) were not in the same day-room at the same time, he said. Their fears could be lessened if the architect could provide tools for them to find their own safety. Pitts designed a clock tower near a nurses station in one building so patients could sit near staff but not right next to them. A place to sit near a dayroom allows patients to see and understand what is going on in the room before entering. Corners or bay windows in a dayroom added structural “texture” that allow patients the choice of being alone or with others.
“They can seek out society or solitude,” said Pitts. “The architect provides the tools to help them find their own safety.”
Today, even health insurance rules can affect building design, he said.“ Shorter stays for patients increase the importance of having clinical zones close at hand. You can't take the time and tie up a staff person to walk the patient across campus to another building for treatment.”
So far, the new psychiatric architecture appears to work. Patients and staff like it, and that may be reason enough to create more of these buildings. Nonetheless, people like Frank Pitts and Richard Lippincott want to go one step farther to see whether design innovations can have a measurable influence on clinical outcomes. “Evidence-based design” may be the next stage in psychiatric therapy, they said.
Lippincott has put together a team of six researchers and is preparing grant applications to investigate the effects of the physical environment on patients. At present, treatment outcomes are measured by length of stay and readmissions, but those criteria may have as much to do with changes in psychopharmacology or patient profiles over the last two decades rather than the design of the new buildings, said Lippincott. He wants to document the effect of architecture on the incidence of suicide and assaults, staff retention, readmission rates, medications, and length of stay.
Whatever the status of research on the intersection of architectural design and psychiatric care, the new approach seems to have had success in practice. Take, for example, the old Rochester (N.Y.) Psychiatric Center, a 16-story, 1,000-bed, concrete-block high rise built in 1955, just before the introduction of chlorpromazine.
“Everybody felt disrespected by the environment,” said to Laurence B. Guttmacher, M.D., now chief of psychiatry and acting clinical director at the center.
A new building, designed by architecture+, opened in 1995.
“The minute they moved over here, the patients started acting better; the staff started acting better,” said Guttmacher. “Working in this building is fundamentally wonderful. It really impressed me with the power of architecture.” ▪