There is an old German saying—Erstens kommt es anderes, und zweitens als man denkt. Or loosely translated: “Life offers many surprises.”
This proverb could certainly apply to the results of a study comparing the use of mental health services in six European countries—Belgium, France, Germany, Italy, the Netherlands, and spain. All have universal health insurance, but the number of psychiatrists and mental health professionals and the way mental health care is delivered differ sharply from country to country.
The investigation was headed by Viviane Kovess-Masfety, M.D., Ph.D., with the MGEN Foundation for Public Health at the University of Paris. The results were published in the February Psychiatric Services.
The European Study of the Epidemiology of Mental Disorders, conducted between 2001 and 2003, is the largest comparative study of mental health in the European Union in terms of sample size (about 9,000 individuals), range of mental disorders evaluated, and information collected. An identical instrument—the Composite International Diagnostic Interview—was used in all six countries to make the assessments. Kovess-Masfety and her colleagues used data from this investigation to conduct their own inquiry into the use of mental health care in the six countries.
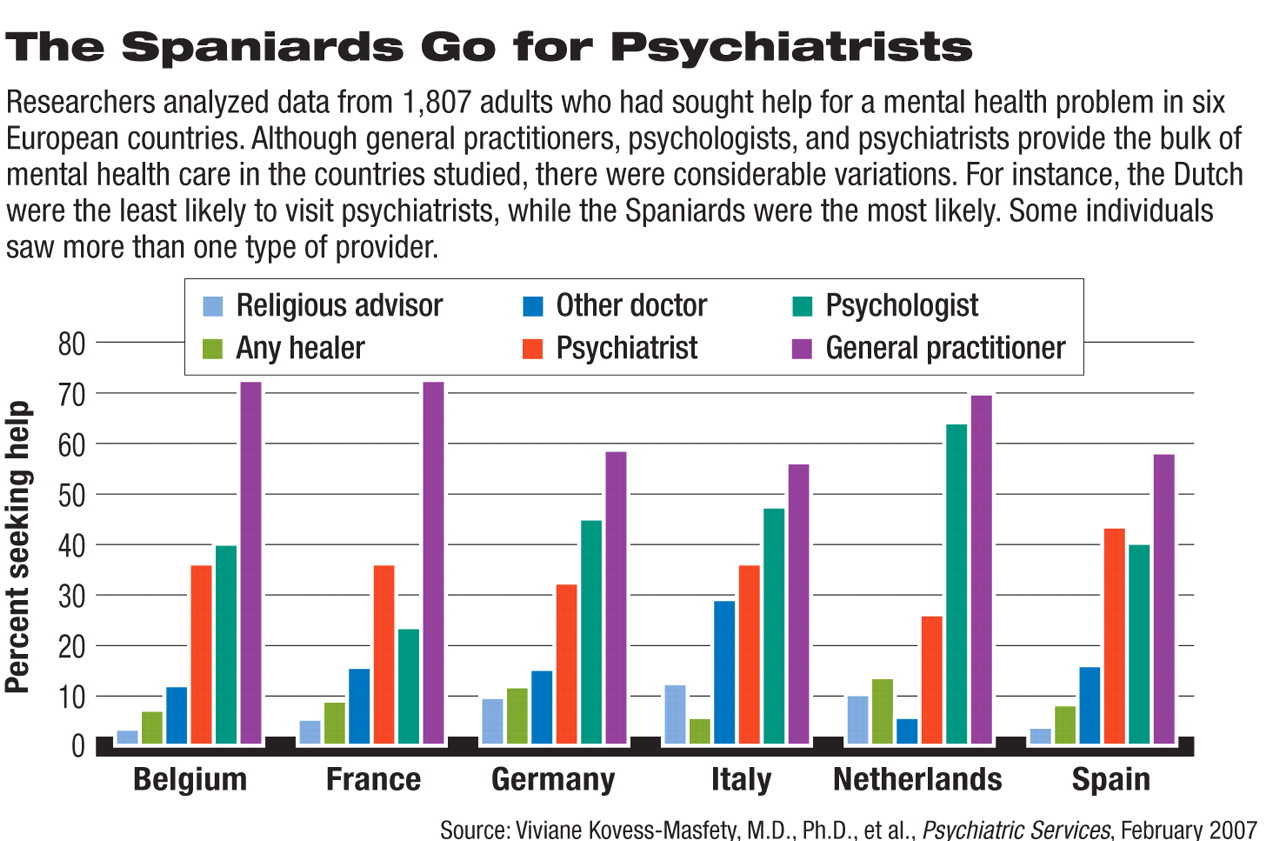
General practitioners were found to be the major mental health providers in all six countries, followed, in general, by psychologists and then psychiatrists. This finding was not surprising. But less expected were the variations found within this general trend. For example, consultations with psychiatrists ranged from 25.5 percent in the Netherlands to 44 percent in Spain.
Moreover, the amount of health care services used by individuals with particular mental illnesses was similar in the six countries. For instance, in each country, individuals with mood disorders used more mental health services than did individuals with anxiety disorders. But when each country's rates of mental health service use for particular disorders were compared with those of the other countries, significant differences emerged. For example, the Italians were the least likely to use services for virtually all mental disorders, and the Dutch were the most likely.
And, as expected, in each country the number of mental health care visits was found to correlate generally with the number of mental health professionals available. But this was not always the case. For instance, even though Belgium had nearly three times the number of general practitioners per capita as the Netherlands, the number of visits to general practitioners for mental health problems was practically identical in both countries. Even though Spain had the fewest psychiatrists per person of all six countries, Spaniards visited psychiatrists more than the Belgians and French, who had more psychiatrists per capita in their countries.
Thus, the use of mental health professionals in these countries is driven not only by their availability, but by some other factors, the researchers conjectured. One such factor might be sociocultural differences. For instance, when Italians experienced a mental health problem, they were less likely than their European neighbors to visit mental health professionals, but were more likely to seek help from religious advisors.
Another variable that might influence the use of mental health professionals in these countries is the extent of mental health insurance coverage provided. For example, in France the cost of psychotherapy is reimbursable only when the psychotherapy is provided by a psychiatrist or other physician. In contrast, the cost of psychotherapy in the Netherlands is reimbursable when the psychotherapy is provided by any licensed psychotherapist.
The investigation was funded by various sources, notably the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the U.S. Public Health Service, Eli Lilly and Co., GlaxoSmithKline, Ortho-McNeil Pharmaceuticals, and the Pan American Health Organization.