Within one year after active interventions ended, adolescents who participated in the Treatment for Adolescents With Depression Study (TADS) largely retained the improvements they evidenced during the study and saw minimal symptom deterioration, a recent analysis conducted by the TADS researchers found.
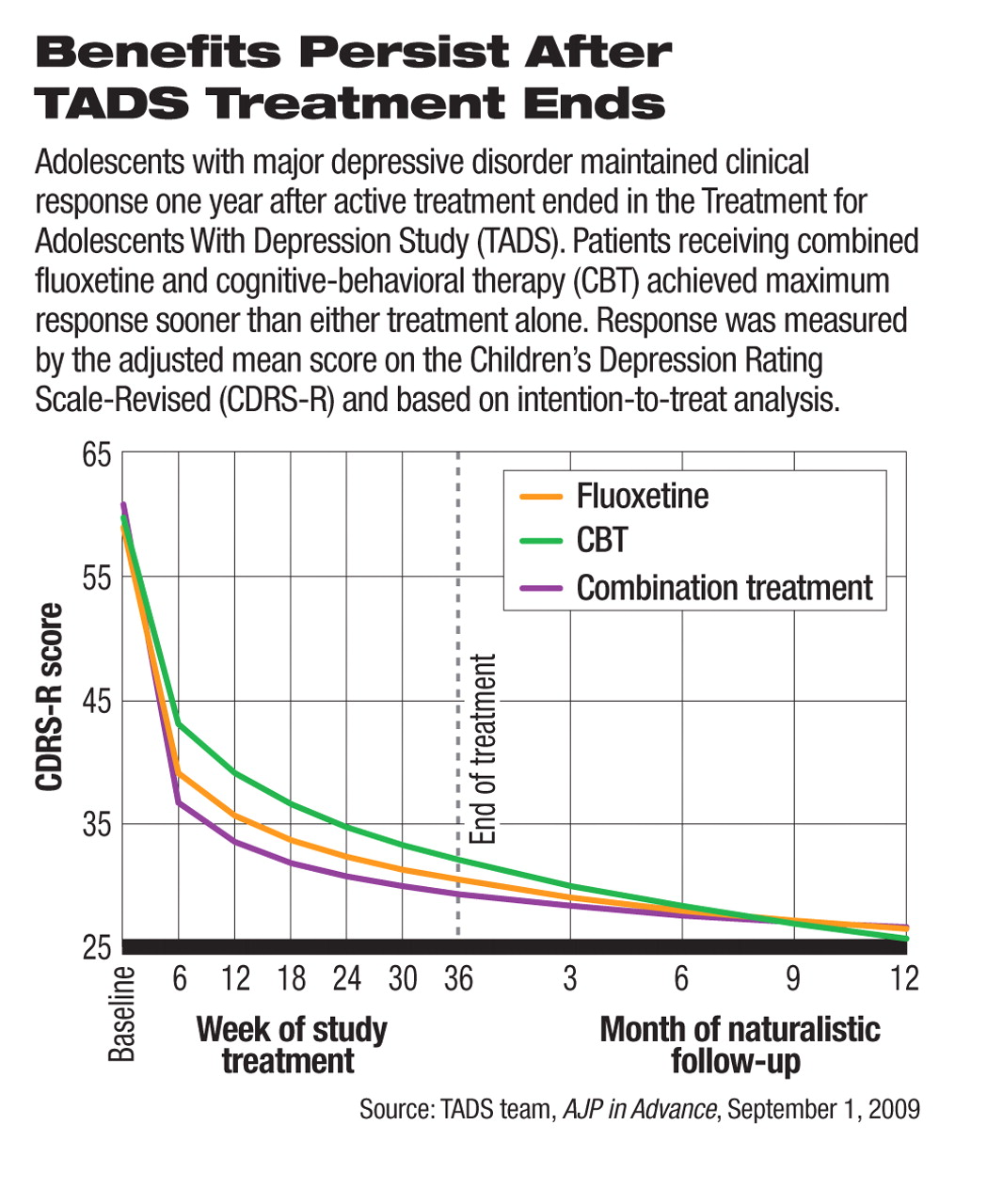
In findings published online September 1 in AJP in Advance, the TADS researchers reported the long-term outcomes of youth with major depressive disorder who had been treated with combined fluoxetine and cognitive-behavioral therapy (CBT), fluoxetine alone, or CBT alone for 36 weeks. After the study-related treatments ended, the clinical benefits the subjects achieved during active treatment were retained similarly across all treatment groups (see chart).
The multisite TADS trial, which began in 1999, was funded by the National Institute of Mental Health (NIMH). During the active-treatment phases of the trial, 327 adolescents aged 12 to 17 with a diagnosis of major depressive disorder were first randomized to acute treatments with fluoxetine, CBT, or both modalities combined for 12 weeks, followed by an additional 24 weeks of open-label, continued treatment. At the end of the 36 weeks of active treatments, 215 patients participated in follow-up assessments every three months, and those who showed signs of relapse were referred to a clinician in the community for additional treatment.
During the yearlong follow-up, 2.8 percent of the patients had a psychiatric-related hospitalization, and about one-third received outpatient mental health care on their own.
A small minority (13 percent) of the study patients were judged to have experienced clinical deterioration during this follow-up period by independent evaluators using the Clinical Global Impression (CGI) scale. Of the subgroup of patients who were in remission at the end of the 36-week active treatment, about 30 percent failed to meet the definition of remission at some point during the one-year follow-up. The three acute-phase treatment groups did not differ significantly on these long-term outcomes.
The finding that most adolescent patients with depression maintained their clinical response after 36 weeks of active treatment contrasts with a short-term study published in the April 2008 American Journal of Psychiatry. In that study, patients aged 7 to 18 who had achieved clinical response after 12 weeks of acute fluoxetine treatment for major depressive disorder were then randomly assigned to either fluoxetine or placebo. During the next six months, 69 percent of patients on placebo and 42 percent who continued on fluoxetine relapsed; the rates were statistically significantly different. The TADS authors also pointed to previous epidemiological and intervention studies showing a relapse rate of 25 percent to more than 50 percent after children and adolescents recovered from a depressive episode.
The relatively high rate of sustained response and low rate of relapse seen in TADS patients is encouraging, but the reason for this favorable outcome is yet to be fully understood.
“There are two explanations for the findings,” John March, M.D., M.P.H., the principal investigator of TADS, told Psychiatric News. He is the director of the Neurosciences Medicine Division at Duke Clinical Research Institute and a professor of psychology and neuroscience at Duke University. “One explanation is that long-term treatment produces sustained response and remission. The other is that [the sustained response] may reflect sample attrition, as only the sustained remitters stayed in the study,” said March.
March cowrote a review of the overall results from TADS so far with Benedetto Vitiello, M.D., chief of the Child and Adolescent Treatment and Preventive Intervention Research Branch at NIMH, which summarized key clinical messages gleaned from the study. The review was also published in AJP in Advance on September 1 and, along with the follow-up study, in the October print edition of the American Journal of Psychiatry.
Among the clinical messages derived from the study data, March and Vitiello noted, is that “it appears that six to nine months of treatment likely will be adequate for the average patient.” Although only 23 percent reached remission at week 12—the end of the acute treatment—the remission rate went up to more than 50 percent by week 36 in all three treatment groups (55 percent for fluoxetine alone, 64 percent for CBT alone, and 60 percent for combined CBT and fluoxetine).
In addition to showing the benefits that accrue from treating patients beyond 12 weeks, TADS also revealed several advantages of combined treatment over using CBT or fluoxetine monotherapy, according to March and Vitiello. For example, although combination treatment did not beat either monotherapy in response rate, patients on combination treatment reached maximum symptom improvement at week 18, on average three months earlier than those on either CBT or fluoxetine alone.
Another notable finding was that adolescents were twice as likely to have suicidal ideation or behaviors if they were treated with fluoxetine only than if they received CBT only or combination therapy. In fact, CBT appeared to have a protective effect on suicidality, since the rate of suicidal ideation or behaviors was significantly higher in the fluoxetine-only group, but similar between the CBT-only and combination therapy groups.
“The Treatment for Adolescents With Depression Study (TADS): Outcomes Over 1 Year of Naturalistic Follow-Up” is posted at<ajp.psychiatryonline.org/cgi/reprint/appi.ajp.2009.08111620v1>.“ Clinical Messages From the Treatment for Adolescents With Depression Study (TADS)” is posted at<ajp.psychiatryonline.org/cgi/reprint/appi.ajp.2009.08101606v1>.“ Fluoxetine Versus Placebo in Preventing Relapse of Major Depression in Children and Adolescents” is posted at<ajp.psychiatryonline.org/cgi/reprint/165/4/459>.▪