Borderline personality disorder (BPD) has come of age.
That's the message in a series of articles in the May American Journal of Psychiatry examining the history of diagnosis and treatment of BPD and the achievements and remaining challenges associated with a psychiatric condition that is among the most troubling—for patients and therapists alike.
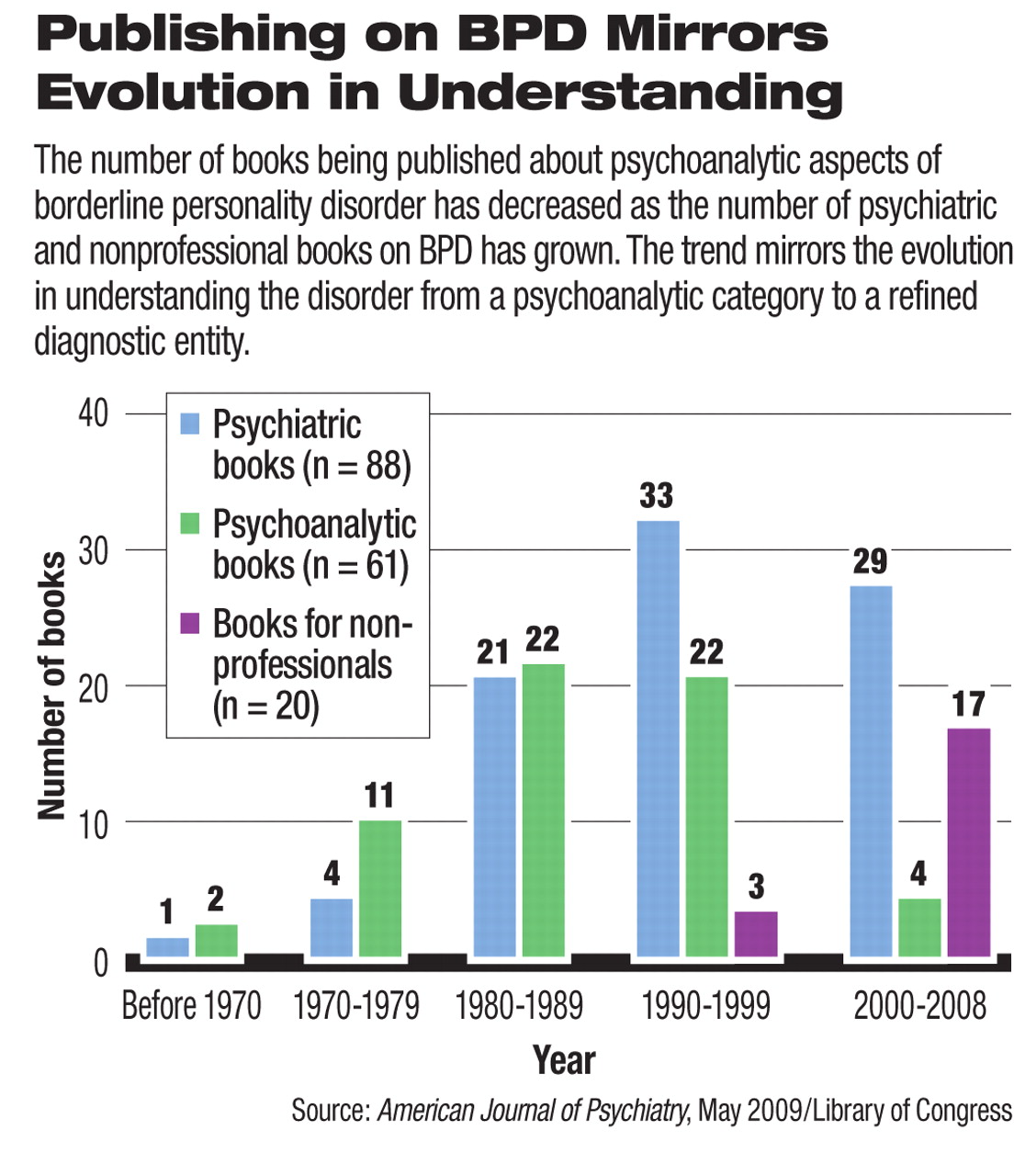
Leaders in research, diagnosis, and treatment of borderline personality disorder agree that what was once a catch-all term originating as a psychoanalytic category is now a highly refined diagnostic entity for which there is an abundant and growing body of research and several evidence-based psychosocial treatments.
At the same time, there remain numerous questions to be answered about the neurobiological basis of the disorder; a number of obstacles to treatment of BPD—especially as a growing body of evidence indicates that successful treatment requires expensive, long-term therapies; and a residue of stigma.
Leading lights in BPD research and treatment including Robert M ichels, M.D., Otto Kernberg, M.D., Glen Gabbard, M.D., John Oldham, M.D., and John Gunderson, M.D., among others, contributed to the series. The series is timed in honor of Congress's designating May “BPD Awareness Month.”
In the article “Borderline Personality Disorder Comes of Age,” Oldham described the largely pejorative description that attached to borderline patients 25 years ago.
“A prototypic image of a borderline patient emerged within clinical settings as an angry, volatile patient prone to reject help, blame others, and behave self-destructively,” Oldham wrote. “Too often, this behavior was seen as willfully oppositional, and borderline patients were spoken of as dreaded pariahs. Recommended treatment was generally psychodynamic psychotherapy or psychoanalysis, often referred to as 'heroic' and of uncertain or poor prognosis.”
In contrast, Oldham described the considerably more informed—and hopeful—state of understanding about the disorder today: key heritable risk factors—especially affect ive dysregulation and impulsive aggression—have been identified, and it is now known that“ [b]orderline pathology is at least partially 'hardwired' involving brain abnormalities that can be identified by brain imaging techniques.”
In addition, new findings suggest that inherent hyperactivity of the amygdala and overreaction to negative facial expressions may correlate with interpersonal hyperactivity, and that these heritable risk factors interfere with normal attachment during development.
“For patients with BPD, these combined etiological factors produce arrested, distorted, or incomplete integration of aspects of self and others, resulting in early onset and persistence of profound interpersonal difficulties,” Oldham wrote. “Normal early development becomes derailed, and the crucial developmental milestone of basic trust is not achieved.”
Gunderson, in the article “The Ontogeny of a Diagnosis,” offered a detailed outline of the origins of BPD as a “psychoanalytic colloquialism,” a category of patients “bordered” by sicker, psychotic patients on the one side and healthier neurotic patients on the other. From there, the conceptualization of the disorder evolved into a“ syndrome,” one largely defined by predictable negative phenomena that occurred within the context of psychotherapeutic treatment.
With the advent of biological psychiatry, research on the disorder began to grow in earnest along with a better understanding of the features that distinguished patients with BPD. And in the 1990s a number of creative psychotherapies—mentalization-based therapy and dialectical behavior therapy—began to be tested and found useful.
Today, Gunderson said, the stigma associated with the disorder among professionals continues, even as public awareness of the condition has grown—as evidenced by an increase in the number of books written about BPD for the general population (see chart).
Much remains to be learned. “Still unknown are the public health costs of this disorder, but given the borderline patients' heavy utilization of psychiatric services; medical complications; involvement in divorce, libel, and childrearing lawsuits; and their violence and sexual indiscretions, the costs can be expected to be tremendous,” Gunderson wrote. “Also unknown, despite significant advances, is borderline personality disorder's core psychopathology and its related neurobiology.”
For this reason, the defining clinical features of BPD continue to be interpersonal ones, he wrote.
So, even as the disorder has evolved from its early amorphous days as a“ psychoanalytic colloquialism,” some aspects of a refined psychoanalytic approach remain highly important in treatment. For instance, Gabbard presented a case history illustrating the usefulness of transference interpretation in treatment.
While some patients show a positive response to certain medications, the effects appear to be short-lived as the core underlying traits of BPD seem to overcome the usefulness of medication. And the successful psychotherapies—whether transference based, mentalization based, or dialectical behavior therapy—require long-term treatment, a major challenge to successful outcome.
“A major shortcoming of present-day research in the treatment of borderline personality is the limited time span of randomized, controlled, clinical trials, contrasting with the widespread clinical impression that long-term treatments are essential for these patients,” wrote Kernberg and Michels in a lead editorial for the series.
“Borderline patients, 20 or 30 years after completion of treatment, still show impoverishment of their personality: a lack of effectiveness and satisfaction in their lives, in their work and professions, and a lack of stability in intimate love and sexual relationships, in establishing families, and difficulty overcoming social isolation. The focus on the long-range course of borderline psychopathology and the effect of interventions on modifying it constitute a major challenge for future research.”
The special series of articles is posted at<ajp.psychiatryonline.org> under the May issue. ▪