Substance abuse co-occurring with schizophrenia is a powerful risk factor for poor outcomes, including treatment nonadherence, relapse, rehospitalization, violence, victimization, criminal justice involvement, HIV, and hepatitis C (
1,
2,
3,
4,
5,
6,
7,
8 ). Estimates of the prevalence of substance use disorders range from 10 to 70 percent, depending on diagnostic assessment methods (
9,
10,
11,
12,
13,
14,
15,
16,
17,
18 ). Further, clinicians often assume that any level of substance abuse is likely to impair psychosocial functioning and lead to adverse sequelae (
16 ). However, several reports suggest that among persons with schizophrenia, substance users have higher levels of interpersonal functioning compared with those who do not use substances, possibly because they have more peer contacts and social skills that bring them into contact with peers who use substances, but these studies have used variable measures of substance use and abuse (
18,
19,
20,
21,
22 ).
Data from the National Institute of Mental Health's Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) (
23 ) provide the opportunity to further examine psychosocial functioning, contrasting nonusers and users with and without impairment by utilizing multiple measures of substance use, including a research diagnostic interview, substance use self-report, clinician ratings, family report, urine drug testing, and radioimmunoassay of hair specimens for illicit substances (RIAH). We sought to examine the relationship between domains of psychosocial functioning measured on the Quality of Life Scale (QLS) (
24 ) and substance use.
Methods
Study design and sample characteristics
The data for this study were collected as part of the CATIE project, a national study investigating the outcomes and cost-effectiveness of currently available first- and second-generation antipsychotic medications. The study was conducted between January 2001 and December 2004 at 57 U.S. clinical sites: 16 university clinics, ten state mental health agencies, seven Department of Veterans Affairs medical centers, six private nonprofit agencies, four private practice sites, and 14 mixed-system sites. Data from one site (33 patients) were excluded from all analyses because of concerns about their integrity. The study was approved by an institutional review board at each site, and each patient or his or her legal guardian provided written informed consent. Details of the study design and entry criteria have been presented elsewhere (
23 ).
We report findings from baseline assessments of 1,460 participants in this study. These data were collected at the time of enrollment—that is, before randomization and the initiation of experimental treatments. Interviewers were trained on reliable administration of all measures and certified specifically for reliable administration of measures of diagnosis, for severity of schizophrenia symptoms, and time to treatment discontinuation.
Measures
Dependent variables. Psychosocial functioning and quality of life were assessed by using the QLS (
24 ), a widely used clinician-rated scale of social functioning, interpersonal relationships, and psychological well-being. The QLS was developed to measure schizophrenia deficit syndrome. The scale contains 21 items with four subscales: interpersonal relations (household, friends, acquaintances, social activity, social network, social initiative, withdrawal, and sociosexual relations), instrumental roles (occupational or educational role, work functioning, work level, and satisfaction), intrapsychic foundations (sense of purpose, motivation, curiosity, anhedonia, aimless inactivity, empathy, and emotional interaction), and common objects and activities. This latter subscale assumes that the extent of participation in routine social and instrumental activities is reflected in the possession of common objects and engagement in certain community activities.
Each item is rated on a 7-point scale, ranging from 0 to 6. A total score is calculated by taking the mean of 21 items. Each subscale is calculated by taking the mean of the subscale items. Higher scores reflect higher functioning—that is, scores of 5 or 6 reflect unimpaired functioning. The QLS has acceptable reliability (
24 ). Intraclass correlations range from .53 to .94 for individual items and .88 to .97 for the four subscales and total score.
Independent variables. Independent variables were chosen on the basis of prior clinical and epidemiologic studies of risk factors related to substance abuse and other outcomes for individuals with schizophrenia.
Demographic characteristics. Items assessed a range of personal demographic and socioeconomic variables, including age, gender (reference group, female), racial status (white compared with all other racial groups; reference group, white), Hispanic ethnicity, marital status (married or cohabiting compared with never married; reference group, never married), education (in years), and employment activity (full-time, part-time, or unemployed).
Clinical history. This item assessed clinical history, including years in treatment assessed via self-report.
Clinical status. These items assessed a broad range of clinical characteristics in addition to overall functioning. Diagnosis of schizophrenia was confirmed by the Structured Clinical Interview for DSM-IV (SCID) (
25 ). Positive, negative, general psychopathology, and total symptoms were assessed with the Positive and Negative Syndrome Scale (PANSS) (
26 ). The assessment of positive symptoms included items such as delusions and hallucinatory behavior. Negative symptoms included items such as blunted affect and emotional withdrawal. General psychopathology symptoms included items such as anxiety, guilt feelings, and lack of judgment and insight. The possible range for the total PANSS score was 30 to 210 (7 to 49 on the positive and negative scales and 16 to 112 for the general psychopathology scale). Higher scores indicate greater symptom severity. The PANSS negative and general psychopathology subscales overlap with several domains measured in the QLS, especially in the areas of impoverished and bizarre social behavior. As a result, in analyses estimating the relationship between clinical characteristics and QLS subscales, only the PANSS positive subscales are used. Clinical status was based on the clinician-rated Clinical Global Impression Scale (CGI) to measure severity of illness. Possible scores range from 1 to 7, with higher scores indicating greater illness severity.
Recent illness exacerbation was assessed by determining if the patient had been hospitalized or treated in a crisis center in the previous three months. Recent victimization was assessed with two questions related to physical and sexual victimization.
Substance use, abuse, and dependence were assessed by using multiple sources of information and coded into three categories: abstinence from substances (no evidence of any substance use), substance use (current alcohol or illicit drug use without serious impairment or without diagnosis of a substance use disorder), and a substance use disorder (current abuse or dependence on alcohol or illicit drugs). The following measures were combined to make these determinations: diagnostic assessment by using the SCID (
25 ), positive hair assay (RIAH) or positive urine screen for illicit drug use, self-reported drug use, clinician rating of substance use on the initial screening inventory, clinician rating from the Alcohol or Drug Use Scale (
27 ), and family report of a problem with alcohol or illicit drugs. Substance use disorder (category 3) was assessed as positive by using the SCID one-month (current) assessment of abuse or dependence. Participants who screened positive for a SCID five-year substance use disorder were also categorized as a current positive diagnosis (category 3) if there was concurrent validation from one of the other indicators of use previously described. Substance use without impairment was assessed as positive by the presence of any indication of substance use in the absence of a SCID one-month or five-year diagnosis of a substance use disorder. No substance use (abstinence) was a residual category indicating no substance use recorded from any of these sources. For some analyses, substance use and substance use disorder were further classified into substance involvement restricted to alcohol compared with substance involvement that included cocaine, either singly or in combination with other substances.
Analytic approach
The sample consisted of 1,460 participants representing the initial (baseline) interview data from the CATIE project before randomization or study drug assignment. Because of small samples at some sites, data from 13 of the initial 57 study sites were collapsed to yield a final count of 50 sites. Substance use was based on the three-level classifications of substance use.
After description of the sample, the associations between psychosocial functioning measured on the QLS and substance use were estimated by using mixed-model multiple regressions that used SAS: PROC MIXED (
28 ). Results expressed as least-square means provide estimates of the predicted mean QLS scores for user subgroups, after the analyses controlled for relevant demographic and clinical characteristics. Participants in the abstinent group were excluded from the latter two sets of analyses. All multiple regression models included demographic covariates for age, gender, race, Hispanic ethnicity, and years of education; clinical status was controlled for by using the PANSS positive symptom scale. Marital status, employment status, and other PANSS subscales potentially measuring deficit syndrome symptoms were excluded because they are also assessed in the QLS. In addition, in a previous study, only the PANSS positive subscale and not the other PANSS ratings differentiated those who used any substances (substance use or substance use disorder) from those who did not (
29 ). The effect of study site was estimated as a random effect. In these models, p values were adjusted for multiple comparisons by using the Hochberg procedure (
30 ).
Results
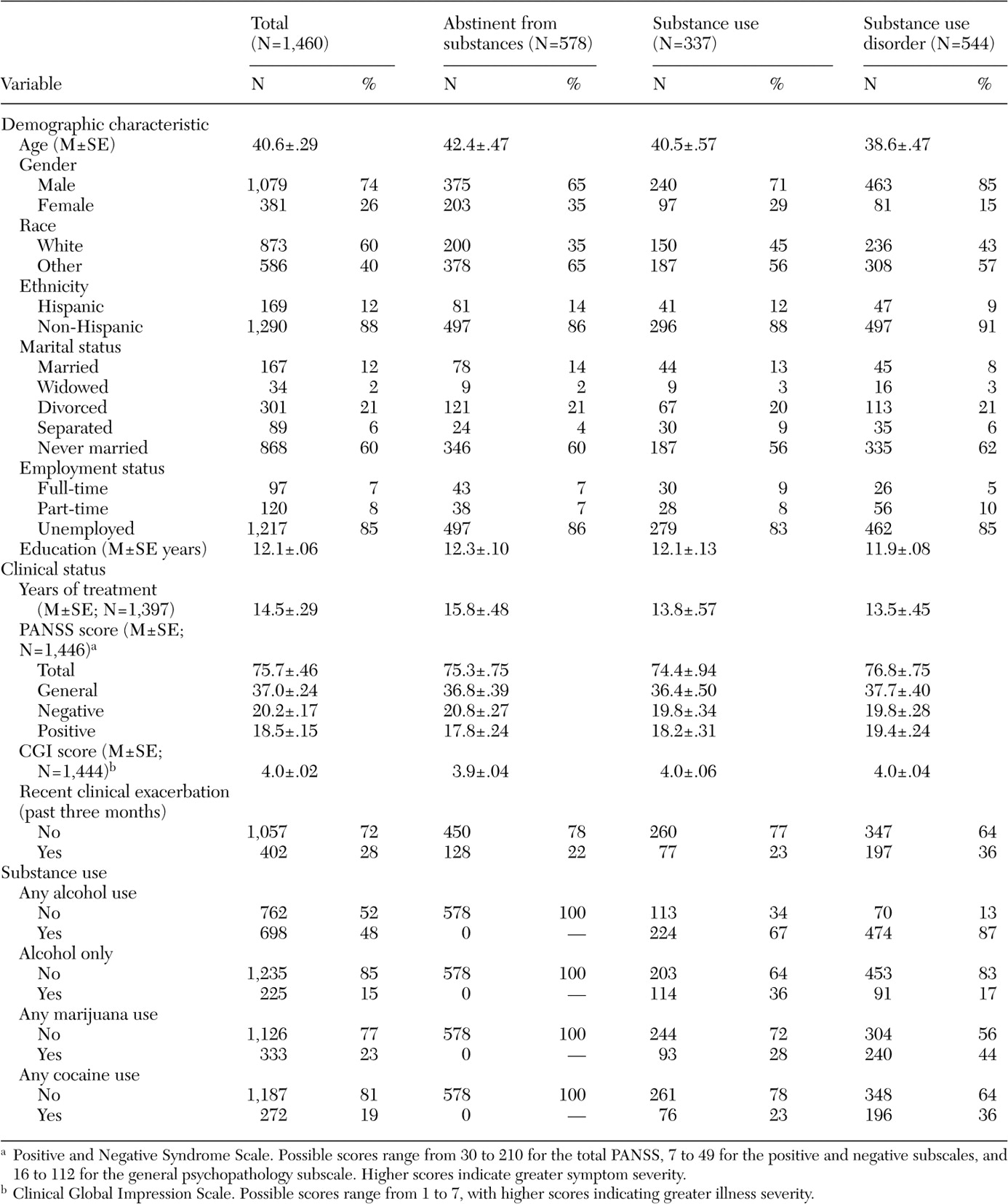
Table 1 lists the distribution of participants' characteristics across the entire sample and within each of the three categories: abstinence, substance use, and substance use disorder. Overall, 337 (23 percent) demonstrated substance use without impairment and 544 (37 percent) had a substance use disorder. A total of 578 (40 percent) were classified as abstinent. For the overall sample, 74 percent were male, 60 percent were white, 60 percent had never been married, 83 percent were unemployed, and 1,080 (74 percent) had received a high school diploma.
Clinically, total PANSS scores averaged 76, with a CGI severity rating of 4, both indicating moderate psychopathology. Twenty-eight percent of the sample had a recent exacerbation of illness requiring hospitalization or emergency care. We have shown elsewhere that persons with schizophrenia and a comorbid substance use disorder were significantly more likely to be male, report more childhood conduct problems, have lower educational attainment, have higher positive symptom scores on the PANSS, and have a recent illness exacerbation requiring hospitalization or emergency care (
30 ). Within the substance use categories, 36 percent with substance use without impairment used only alcohol; among those classified as having a substance use disorder, 17 percent used alcohol alone. Of those with a substance use disorder, 87 percent used alcohol, 44 percent used marijuana, and 36 percent used cocaine. Rates of polysubstance use were higher among those with a substance use disorder compared with those who used substances (317 participants, or 58 percent, compared with 91 participants, or 27 percent).
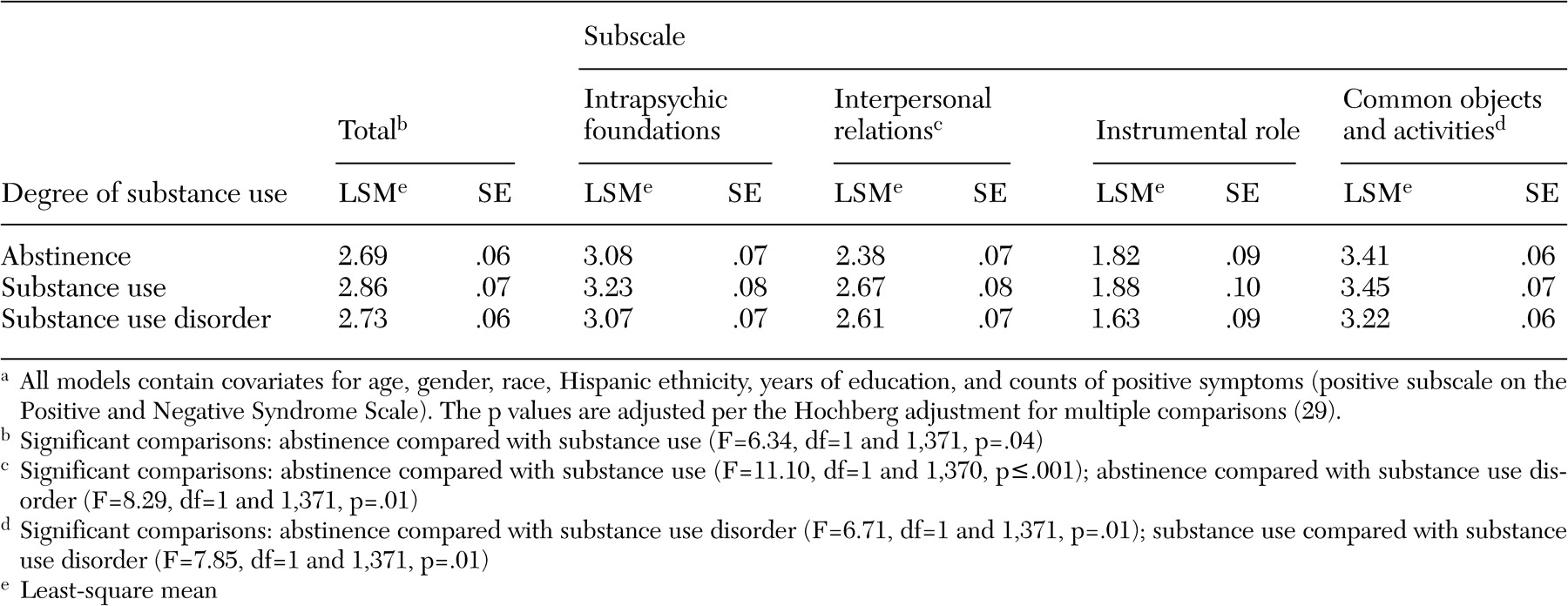
The predicted mean QLS scores for each patient subgroup after adjustment for the effects of other potential demographic and clinical factors are presented as the least-square means with standard errors. The QLS and its four subscales were compared for the abstinence, substance use, and substance use disorder groups. As shown in
Table 2, scores for the QLS total and subscales showed moderate to marked impairment across all groups, consistent with a sample with chronic schizophrenia.
Compared with participants who were abstinent, those who used substances had significantly higher scores on the total QLS and the interpersonal relations subscale, indicating higher overall functioning and more frequent social contacts. However, effect sizes for each—.10 and .22, respectively—indicated relatively small, but significant, increments in functioning. Compared with participants who were abstinent, those with a substance use disorder had equivalent overall functioning, higher scores on the interpersonal relations subscale (effect size=.10), and lower scores on the common objects and activities subscale (effect size=.30), indicating a small but significant increment in social contacts and moderate decreased engagement in social, vocational, and instrumental activities. Participants with a substance use disorder differed from those who used substances only in having lower scores on the common objects and activities subscale (effect size=.27), indicating a moderate decrease in involvement in routine social, vocational, and instrumental activities.
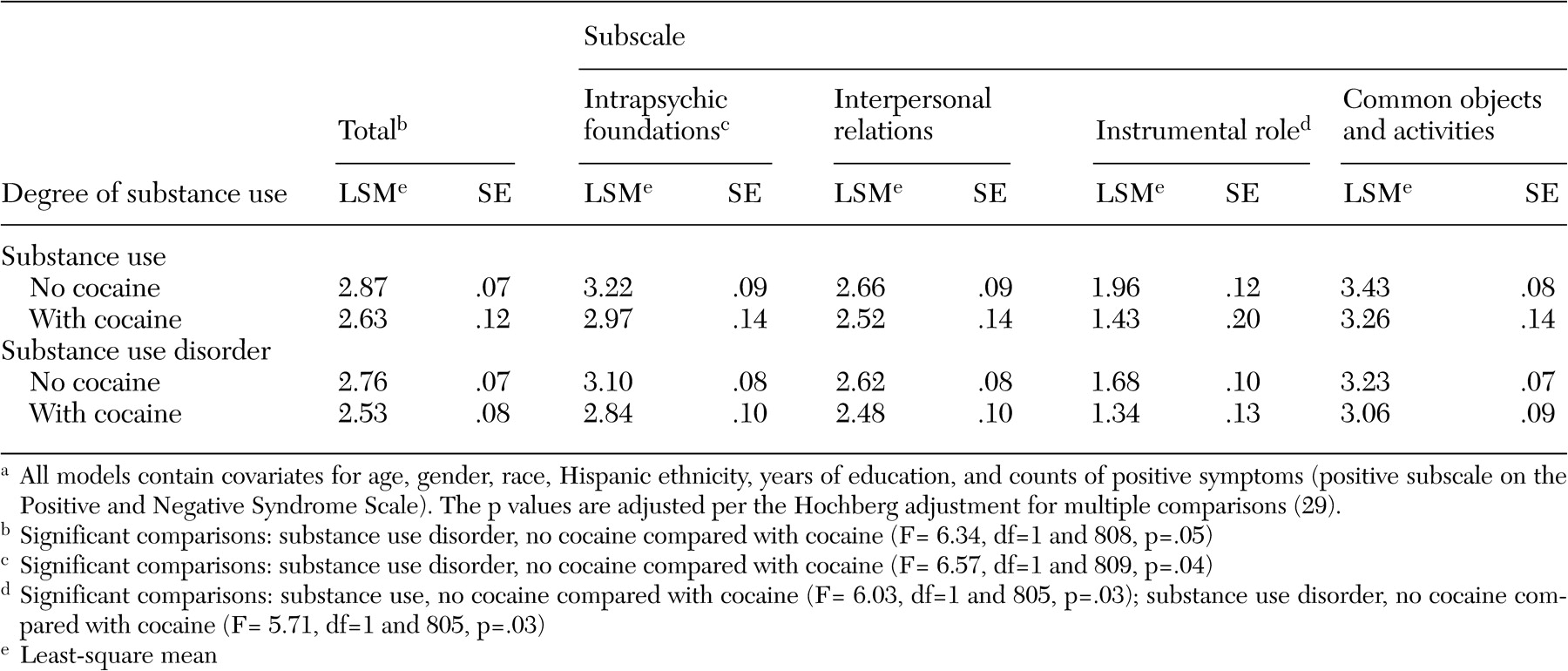
On the basis of visual inspection of QLS scores across participants with any substance use (data not shown), cocaine use appeared to be associated with different patterns of functioning than other types of drug use, including cannabis; the pattern for alcohol and cannabis appeared similar to patterns for other types of drug use. Two subsequent subanalyses examined the association between psychosocial functioning and specific patterns of substance use involving cocaine. In the first analysis (data not shown) participants who used only alcohol were compared with those who also used illicit substances; no significant differences in psychosocial functioning were found. As presented in
Table 3, in the second analysis, data were compared for participants whose pattern of substance use involved cocaine and those who used other substances but no cocaine. Among participants who used substances, cocaine use was associated with a small to moderate decrease in scores on the instrumental role functioning subscale (effect size=.26); however, the effect among those with a substance use disorder was more striking, with cocaine users having moderate reductions in total QLS scores (effect size=.36), scores on the intrapsychic foundations subscale (effect size= .32), and scores on the instrumental role subscale (effect size=.34).
In all models, female gender and years of education were associated with significantly higher levels of functioning, whereas higher positive PANSS scores were associated with lower levels of functioning. Older age was significantly associated with lower functioning on the aggregate QLS and the interpersonal relations and instrumental role subscales but not on the intrapsychic foundations or common objects and activities subscales. Race and Hispanic ethnicity were not significantly associated with functioning on any subscale. Models that included baseline antipsychotic medication before study enrollment did not affect these results.
Discussion
This study utilized multiple clinical and laboratory methods to provide sensitive detection of substance use in schizophrenia and contrasted psychosocial functioning associated with abstinence, substance use, and substance use disorder. Overall, 23 percent of the total sample appeared to have current substance use without impairment and 37 percent showed evidence of a current substance use disorder. These rates of substance use are generally consistent with previous comorbidity studies (
9,
10,
11,
12,
13,
14,
15,
16,
17,
18 ), although most previous studies have not estimated substance use and substance use disorder separately or used multiple methods of detection, including RIAH.
The QLS was originally developed to measure psychosocial functioning associated with schizophrenia deficit syndrome. We found that participants with schizophrenia who were substance users (and similarly those with a substance use disorder) had somewhat higher or equivalent overall functioning than those who were abstinent. One important exception is that persons with a substance use disorder exhibited significantly decreased engagement in social, vocational, and instrumental activities. On the whole, as measured by the QLS, participants in the two substance use groups showed no more evidence of schizophrenia deficit syndrome than abstainers. We previously reported that patients with substance use and those with a substance use disorder had higher scores on the PANSS positive subscale but no evidence of greater negative symptomatology than abstainers, which is consistent with the view that substance use is unrelated to a deficit syndrome in symptoms or functioning.
These findings of higher QLS scores among substance users are also consistent with findings by Salyers and Mueser (
18 ) that patients with schizophrenia who use substances have evidence of better social functioning. This may be because a certain level of initiative, organization, and social contact is a precondition for engaging drug-involved peers and procuring illicit substances. However, substance use disorder that involved cocaine use appears to be distinct and clearly associated with worse psychosocial functioning, especially in relation to work, school, or homemaking functions. These findings are also consistent with Drake and colleagues' (
31 ) observation that patterns of substance use and substance use disorder in this population are not driven by a need to self-medicate negative symptoms or other biologic proclivity but rather reflect this population's immersion in neighborhoods and peer social networks in which drugs are used. Hence patterns of use of specific illicit substances in schizophrenia are similar to patterns of use in the community. This ecological view of comorbidity also suggests that treatment of substance abuse in schizophrenia should focus on reconnecting users to nonusing peer groups without holding out undue hope for a specific pharmacologic treatment of substance use in schizophrenia.
Within the two groups that used substances, we found no differences in QLS scores between participants who used or abused alcohol compared with polysubstance users. By and large, impairment was associated with the level of involvement with substances (for example, abuse and dependence compared with use) rather than use of alcohol only compared with polysubstance use. In contrast, cocaine use in the group with a substance use disorder did appear to have a more deleterious effect on several domains of functioning. The cocaine users had moderately lower functioning, even compared with a general sample of persons with chronic schizophrenia, suggesting clinically significant functional decrements. Further, we interpret the disruption of psychosocial functioning among participants whose substance use disorder involved cocaine use as evidence of the detrimental effects of involvement with a criminogenic drug subculture combined with sensitivity to cocaine's deleterious pharmacologic effects.
As reported, the effect sizes for these differences in subgroups were generally small, with the exception of medium effect sizes associated with cocaine abuse. Bigger differences—particularly decrements in functioning associated with a substance use disorder—may have been harder to detect because the QLS rating for the entire sample was relatively low. Larger differences may have been evident if the level of consumption of substances was quantified. In addition, at baseline the clinician raters may have had less experience and fewer sources of ancillary data about the participants and their substance use patterns than they would gain over the course of the study.
This study is limited in several ways. First, these cross-sectional data cannot actually demonstrate causal connections between variables; rather, they show statistical associations, which may be consistent with several causal formulations.
Second, although the study used urine and hair samples to test for drugs, no laboratory assays were utilized to detect alcohol use. As a result, findings regarding alcohol involvement are more dependent on self-report than the estimates of illicit drug use, although self-disclosure of alcohol use should be less stigmatizing. Nonetheless, these findings may be underestimates of alcohol use relative to illicit substances and may be conservative estimates of the true prevalence of total substance use among persons with schizophrenia. In addition, we did not ask participants to estimate their consumption of alcohol or illicit drugs, and although we have carefully characterized the substance use patterns, we cannot make finer-grained distinctions about the level of consumption of each substance.
Third, participants in the CATIE study may not be representative of all persons with schizophrenia—particularly those at highest risk for substance use. On the one hand, by including 57 sites from across the United States, the CATIE study arguably includes data on schizophrenia that are extremely generalizable. Further, we can employ statistical techniques to control for variability across these different sites. In this way, the CATIE study permits analysis that is both externally and internally valid. On the other hand, the CATIE sample represents a group of treated patients with schizophrenia who were willing to enroll in a clinical trial of antipsychotic medication—a group that may not be representative of the population of interest.
Conclusions
Substance use and use disorders, unless cocaine use was involved, were generally associated with higher or equivalent overall psychosocial functioning compared with abstinence from substance use. Patterns of use of specific illicit substances in schizophrenia were similar to substance use patterns in the community, suggesting that treatment of substance use disorders in schizophrenia should focus on reconnecting substance users to nonusing peer groups.
Acknowledgments
This article is based on results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project, supported by grant NO1-MH-90001 from the National Institute of Mental Health (NIMH). The project was carried out by principal investigators from the University of North Carolina, Duke University, the University of Southern California, the University of Rochester, and Yale University in association with Quintiles, Inc., the program staff of the Division of Interventions and Services Research of NIMH, and investigators from 56 sites in the United States (CATIE Study Investigators Group). AstraZeneca Pharmaceuticals L.P., Bristol-Myers Squibb Company, Forest Pharmaceuticals, Inc., Janssen Pharmaceutica Products, L.P., Eli Lilly and Company, Otsuka Pharmaceutical Co., Ltd., Pfizer, Inc., and Zenith Goldline Pharmaceuticals, Inc., provided medications for the studies. The Foundation of Hope, Raleigh, North Carolina, also supported this work. Details about the CATIE Study Investigators Group are available at www.catie.unc.edu/schizophrenia/locations.html#clinicalsitelocation list.