Attention-deficit hyperactivity disorder (ADHD) is one of the most common childhood neuropsychobiological disorders. Two evidence-based treatments for ADHD, psychotropic medication and behavioral therapies implemented at home and school, have been identified (
1 ).
The use of stimulant medication for ADHD has increased during the past decade; higher rates of stimulant use in community samples have been associated with latency age, male gender, presence of impairment, Caucasian background, and having insurance (
2 ). These studies have not addressed parental or caregiver (collectively termed "caregiver") mental health status and its impact on use. Related research has found high rates of mental health problems among mothers of youths presenting for mental health services (
3,
4 ). Poorer outcomes (
5 ) and increased use of general pediatric services have been found among youths with depressed caregivers compared with youths whose caregivers are not depressed (
6 ). The impact of caregiver depression on medication use for youths with ADHD is critical to examine, particularly for youths served in the public sector who are at heightened risk for mental health disorders (
7 ).
For youths meeting DSM-IV criteria for ADHD in a sample of youths served in public-sector systems, our research question was, does caregiver depression affect youths' use of medication?
Methods
This research examined data from the Patterns of Youth Mental Health Care in Public Service Systems study, funded by the National Institute of Mental Health (NIMH). The study investigated mental health needs of youths served in public systems in San Diego. The prevalence of psychiatric diagnoses in the sample was high (54%). Study procedures called for data collection over a two-year period, including administrative data from public-sector systems and structured face-to-face interviews with caregivers and youths at wave 1 (October 1997 through January 1999) and wave 2 (November 1999 through March 2001). In addition, telephone interviews were conducted with caregivers at six, 12, and 18 months. Interview topics included demographic characteristics and youth's life history, youth's mental health and risk factors, and service utilization. Interviews averaged two to three hours, and compensation ranged from $10 and $40, depending on interview length.
After institutional review board approval, participants were selected from an unduplicated enumeration of youths ages six through 17 and served by five systems in San Diego (mental health, alcohol and drug services, child welfare, juvenile justice, and special education services for emotionally disturbed youths) during the second half of fiscal year 1996-1997. The sampling frame was stratified on the basis of patterns of single- or multiple-sector use, home versus aggregate care setting, and race and ethnicity. After we removed duplicate records, 3,417 youths were randomly selected to participate. Of these, 1,715 youths and their caregivers completed informed consent forms and completed at least one interview. Most of the caregivers were biological parents (71% at wave 1; 68% at wave 2). Participants did not differ significantly from nonparticipants except that fewer Asians participated relative to eligible participants. Analyses were weighted to account for this difference. Follow-up at two years was 93%.
To delineate the subsample of youths for the current analyses, an ADHD diagnosis was determined via caregiver or youth report at wave 1 on the Diagnostic Interview Schedule for Children (DISC-IV) (
8 ), an instrument designed to yield
DSM-IV diagnoses (
9,
10,
11 ). The instrument has demonstrated reliability in its English (
8 ) and Spanish versions (
11 ). Diagnoses were considered present if all criteria were met on scoring algorithms for either the caregiver or youth report and at least one moderate level of diagnosis-related impairment was endorsed. Of the 444 youths meeting
DSM-IV criteria for ADHD on the DISC-IV, 390 had complete data and were included in the current analyses. On all variables included in the models, weighted t tests and chi square tests comparing youths with and without missing data suggested no undue selection bias except in race and ethnicity, where youths in the "other" category were more likely to be missing data (F=3.88, df=3 and 1,268, p=.010; uncorrected
χ 2 =19.04).
The English and Spanish versions of the NIMH Services Assessment for Children and Adolescents (SACA) (
12 ) were used to ascertain caregiver report of adolescents' use of psychotropic medication. The dependent variable for these analyses, medication use in the past 12 months, was a composite of caregiver responses to the 18-month telephone interview and the wave 2 interview. A kappa of .96 has been established, and was used in this study, for medication use within the past six months (
12 ). Caregivers were asked about ADHD medication use in the previous six months. Answers were confirmed with prescription bottles when possible. Medication use for ADHD was operationalized on the basis of expert opinion guidelines published at the time of sample selection and included stimulants, bupropion, nortryptiline, and imipramine (
13 ).
The independent variable of interest, caregiver depression, was measured dichotomously at wave 1 with the published cutoff of 16 or higher on the Center for Epidemiological Studies-Depression Scale (
14 ).
Covariates in the model were drawn from the literature and included youth sociodemographic characteristics and caregiver education level at wave 1, caregiver report of youth receipt of a clinical diagnosis of ADHD at any time before the wave 2 interview, impairment at wave 1 measured by the Columbia Impairment Scale (
15 ), DISC ADHD diagnosis subtype (hyperactive-impulsive or combined subtype versus inattentive subtype), youth insurance status at wave 1, whether the youth was using mental health services at the time of enumeration, and caregiver physical health (5-point Likert scale collapsed to a dichotomous variable) at wave 1. Additional covariates measured by the SACA included use in the past 12 months (at wave 2) of outpatient general medical services; specialty outpatient mental health services provided by community mental health clinics and private professionals, such as psychologists, psychiatrists, and social workers; and school-based services in a special school for students with emotional or behavioral problems, in a special classroom or mainstream classroom in a regular school, or counseling or therapy. Test-retest reliability of the English and Spanish SACA is reported as ranging from fair to moderate for most service use variables (
12 ).
Analyses conducted included descriptive statistics (with weighted percentages), bivariate regressions, multivariate logistic regression modeling, and regression diagnostics. Analyses were conducted with the Stata statistical package, version 7.0, to allow for appropriate weighting of the data. All percentages reported were weighted to reflect sampling.
Results
The mean±SE age of the sample of 390 youths was 12.80±.18 years; 280 youths (71%) were male. The ethnic composition included 244 (61%) Caucasians, 53 (13%) Latinos, 64 (18%) African Americans, and 29 (7%) of other backgrounds. Caregivers reported that only 141 youths (38%) used psychotropic medication in the past 12 months. High rates of caregiver depression (N=153, or 41%) were found despite high rates of caregiver good health (N=293, or 73%). Other notable findings included high rates of youth public insurance (N=234, or 64%), ADHD hyperactive-impulsive subtype or ADHD combined subtype (N=233, or 62%), youth impairment (N=289, or 72%), and low caregiver educational attainment (N=233, or 60%). About two-thirds of youths (N=225, or 66%) had been active clients in the mental health services sector at the time of enumeration. Rates of general medical services (N=80, or 19%) were lower than rates of outpatient subspecialty mental health (N=233, or 60%) and school-based services (N=257, or 64%).
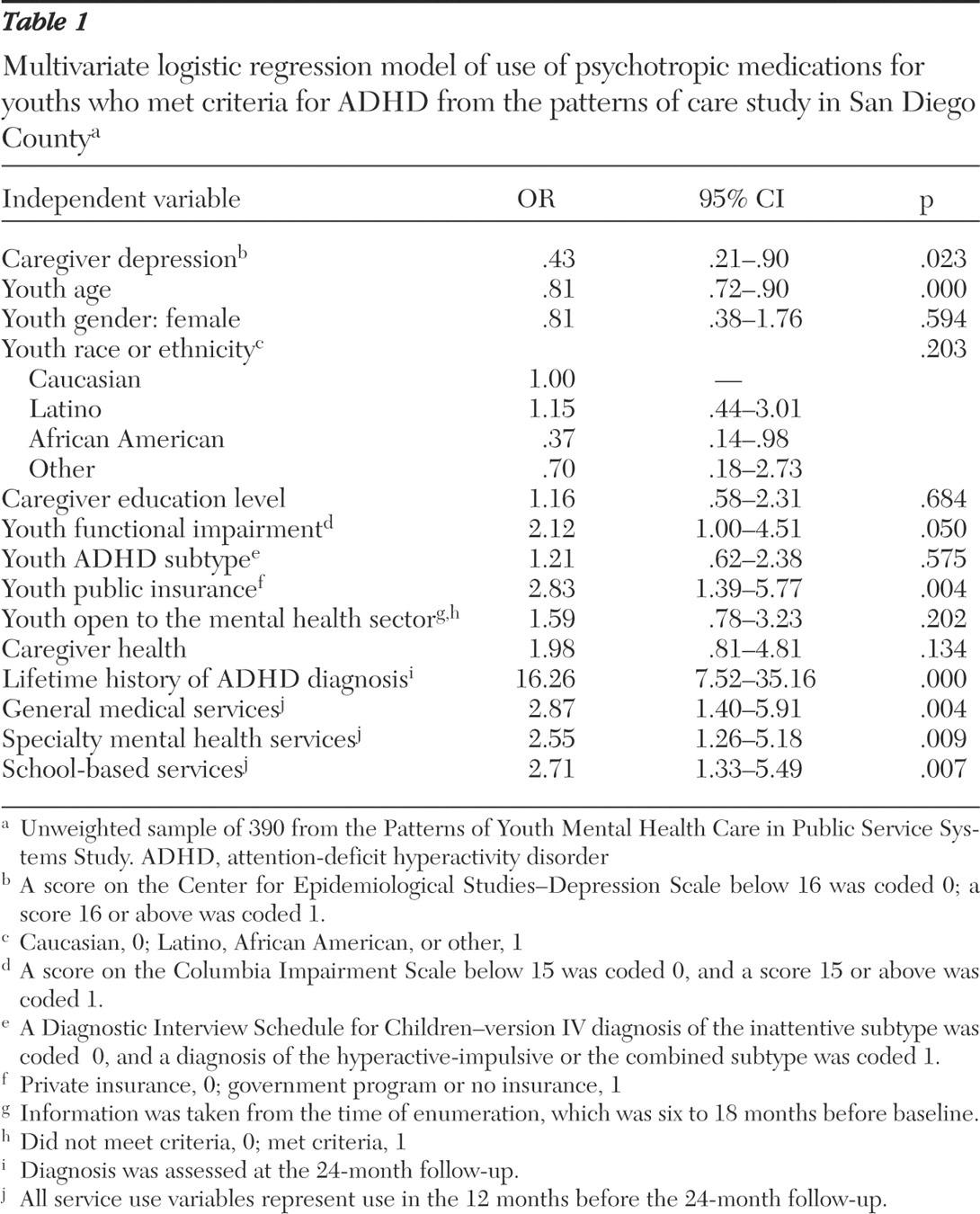
When data were examined in a multivariate logistic regression model that controlled for all covariates, caregivers who scored greater than 15 on the CES-D were half as likely as those who scored 15 or less to report medication use by youths in the past 12 months before the wave 2 interview. Youths who received medication were also more likely to be younger; be publicly or not insured; have a caregiver-reported history of a clinical ADHD diagnosis; and have received general medical, mental health, or school-based services in the past 12 months (
Table 1 ).
Discussion
This study examined medication use for a cohort of youths with positive DISC diagnoses of ADHD and who were active users of public-sector services in San Diego. Service use included lower general medical use and higher use of school-based and mental health services than has previously been described in community samples. These differences may reflect the Patterns of Care study sample because it consisted of youths who were already active in one or more public systems and at heightened risk for mental health problems.
Caregivers with depressive symptoms at baseline were half as likely to report that their children were using medications for ADHD at months 12 through 24 after the baseline interview, a worrisome finding given the high rate (41%) of caregiver depression in this sample. If causal, this finding may reflect caregivers' inability—as a result of their own impairment—to pursue medication for their child in California, which requires monthly triplicate prescriptions. The finding may also reflect that caregivers' personal experience with psychotropic medications negatively influenced decisions to seek medication for their child's problems. Mental health professionals caring for these children may also make decisions about treatment plans on the basis of their perceptions of the caregivers' abilities to adhere to a complicated treatment regimen. Alternatively, youths with poorly managed ADHD or complicated coexisting conditions may predispose caregivers to depression. Clearly this finding needs to be replicated and further explored with respect to direction and mechanisms of effect and dose-response relationships.
This study has several limitations. First, findings may represent idiosyncrasies of the San Diego public-sector systems. Second, medical records were not abstracted to determine accuracy of caregiver reports. Third, we did not examine caregiver depression as a function of the child's setting—that is, whether the child was placed in a nonrelative's foster home, with kin, or in a juvenile justice facility versus with a biological parent. Finally, no conclusions can be drawn regarding the quality of services provided or whether services across sectors were provided in a collaborative manner.
Conclusions
This study represents an important effort to disentangle factors affecting ADHD service use. Our findings of relatively low rates of medication use and an association between caregiver depression and medication use among youths cared for in the public sector highlight the need for increased attention to this vulnerable subpopulation of youths with ADHD.
Acknowledgments and disclosures
This study was supported by grants K08-MH-64816 and U01-MH-55282 from the National Institute of Mental health. The authors thank the agencies of the County of San Diego and the families and youths who participated in this study. The authors also thank Donald J. Slymen, Ph.D., Stephanie Brodine, M.D., and Sally Mathiesen, Ph.D., for their conceptual advice.
The authors report no competing interests.