An estimated ten million to 17.5 million adults in the United States have a serious mental illness (
1,
2,
3 ). Section 1912(c) of the Public Health Service Act defines adults with serious mental illness as individuals aged 18 years and older who have a diagnosable mental, behavioral, or emotional disorder that meets criteria in the
DSM-IV (
4 ) and results in functional impairment that substantially interferes with or limits one or more major life activities. Estimates for the prevalence of adults with serious mental illness vary depending on the criteria and screening method used and the characteristics of the population examined, but according to a recent study that examined data from the National Comorbidity Survey Replication (NCS-R), the 12-month prevalence of serious mental disorders is estimated to be 5.3% among people 18 to 54 years of age (
5 ). The three most common types of mental disorder among people with serious mental illness are schizophrenia, bipolar disorder, and major depression.
In response to concern about the unmet need for treatment among individuals with serious and debilitating forms of mental illness, the federal government passed in 1992 public law (PL) 102-321—the Alcohol, Drug Abuse, and Mental Health Administration Reorganization Act—to establish the Substance Abuse and Mental Health Services Administration (SAMHSA). PL 102-321 mandated SAMHSA to provide states with block grants that fund mental health services for adults with serious mental illness and children and adolescents with serious emotional disturbances. According to a report by the Center for Mental Health Services (
6 ), in the past three decades the use of psychiatric care by people with mental illness increased considerably because of many factors, including increased awareness of the need for mental health services and increased availability of and access to care (
5 ).
Surprisingly, little published research is available on the trend in the use of psychiatric care among adults with serious mental illness. One of the few exceptions is a study by Kessler and colleagues (
5 ), who reported the results of analyses of data from nationally representative, face-to-face household surveys of individuals 15 to 54 years of age (NCS) or 18 years of age and older (NCS-R). According to the Kessler team's study, between 1990 and 1992 approximately 12% of people with a serious mental disorder reported receiving treatment; the rate for the prevalence of treatment among people with a serious mental disorder rose to about 20% between 2001 and 2003. The increase in the treatment rate was confirmed by another study by Mechanic and colleagues (
7 ), who examined data from the National Hospital Discharge Survey and the Inventory of Mental Health Organizations from 1988 to 1994. The study found that the rate of discharge from hospitalization for serious mental illness significantly increased in general hospitals, from approximately 196 to 314 discharges per 100,000 in the U.S. population. Private nonprofit hospitals saw the largest increase, almost 90%. During this period public hospitals experienced a significant decline of 28% in the rate of discharge involving serious mental illness.
The purpose of this study was to examine more recent data from the National Hospital Discharge Survey (1995 to 2002) to investigate whether the trend in general hospital discharges involving serious mental illness continued to increase. Further, to seek insights into potentially increasing trends in such discharges, we examined the trends in relation to hospital and patient characteristics and geographic regions.
Methods
Discharge survey data
We analyzed National Hospital Discharge Survey data for 1995 through 2002, the most recent year data were available (
9 ). Briefly, the National Center for Health Statistics (NCHS) conducts the survey annually to collect data on inpatient utilization from short-stay, noninstitutional, and nonfederal hospitals in the 50 states and the District of Columbia. The National Hospital Discharge Survey is the primary source for national data on the characteristics of patients discharged from nonfederal, short-stay hospitals. When interpreting the results, it is important to keep in mind that the survey produces estimates of inpatient activity; it does not collect data on ambulatory medical services or outpatient or emergency visits. The survey produces estimates for discharges, not persons, because persons with multiple discharges during the year can be sampled more than once (
10 ).
The National Hospital Discharge Survey collects data from general hospitals, children's general hospitals, and hospitals with an average length of stay of fewer than 30 days for all patients. Not eligible for inclusion in the survey are federal, military, and Department of Veterans Affairs hospitals; hospital units of institutions (such as prison hospitals); and hospitals with fewer than six beds. The survey uses a three-stage probability design, and the data are weighted to represent national inpatient hospitalization. Of 474 eligible hospitals, 445 responded to the survey in 2002, and data were collected for approximately 327,000 discharges (
9 ).
We selected for analysis all individuals aged 18 years and older who had a primary diagnosis of mental illness and serious mental illness. ICD-9-CM codes between 290 and 319 were considered to indicate mental illness. For serious mental illness, we selected the following codes: schizophrenia (295 and 297–299), bipolar disorder (296.0, 296.1, and 296.4–296.9), obsessive-compulsive disorder (300.3), and major depressive disorder (296.24 and 296.34).
Additional data
Hospital discharge rates per 10,000 in the U.S. population were calculated by using denominator estimates of the civilian, noninstitutionalized U.S. population from the U.S. Census Bureau (
11 ), which were adjusted for underenumeration. Numerators were the numbers of discharges, weighted to represent the U.S. population. Length of stay was measured as the number of hospitalization days from the admission date to the discharge date, with length of stay of less than one day recoded to equal one day.
Hospital ownership was categorized as proprietary, government, or nonprofit. Proprietary hospitals included hospitals operated by individuals, partnerships, or corporations for profit. Government hospitals included hospitals operated by state and local governments. Nonprofit hospitals included hospitals operated by a church or another nonprofit hospital. The expected primary source of payment was categorized as private insurance, government, or other. Private insurance included Blue Cross and Blue Shield, health maintenance organizations or preferred provider organizations, and other private insurance. Government insurance included Medicare and Medicaid, workers' compensation, and other government insurance. Other insurance included self-pay and no charge. Regions were coded according to the U.S. Census Bureau's classification as Northeast, Midwest, South, or West.
Statistical analysis
We conducted bivariate analyses to examine the trends for specific patient- and hospital-level characteristics. We did not conduct multivariate analyses because this analysis was exploratory. For race and ethnicity, we examined non-Hispanic white and black populations. Other racial groups were not examined because samples were too small. Also, in our analysis for race we did not include data on unknown race and ethnicity because there is no ideal way to adjust for underreporting of race in the National Hospital Discharge Survey (
12 ). According to a study conducted by NCHS, underreporting of race is more likely to affect the estimate for white discharges than for black discharges (
12 ). The NCHS concluded that research can be done on hospital use patterns within racial groups, and if the differences between racial groups are large, general inferences can be drawn from the National Hospital Discharge Survey data. Therefore, we examined the group-specific trends but did not conduct formal statistical analyses to compare different ethnic groups.
Considering the complex sample design of the National Hospital Discharge Survey, NCHS recommends the following guidelines for presenting survey estimates: the value of the estimate is not reported if the sample size is less than 30; the value of the estimate is reported but should not be assumed reliable if the sample size is 30 to 59 persons; the estimate is reported if the sample is 60 or more and the relative standard error is less than 30%; the estimate is considered to be unreliable if the relative standard error of any estimate is over 30% (
13 ). The relative standard errors for National Hospital Discharge Survey estimates were obtained with SUDAAN software (version 9.0) by using first-order Taylor series approximation of the deviation of estimates from their expected values.
In this analysis, we presented the estimates with unweighted samples of more than 60 patients and the relative standard error measures of less than 30% to meet National Hospital Discharge Survey criteria. In order to examine the changes in hospital discharge rates over the eight-year period, we used the generalized linear model procedure in SAS (version 9.1) to test for trends. The level of significance was set at p<.05. We did not make adjustments for multiple comparisons but included the exact p values in our results to show the level of significance. In this analysis we took into account the complex survey design of the National Hospital Discharge Survey, using relative standard errors computed from SUDAAN.
Ideally, we would have examined the trends from both general hospitals and psychiatric hospitals for discharges associated with serious mental illness, but data on psychiatric hospital discharges were not available for this analysis. However, our results based on general hospital (inpatient psychiatric services) discharges provide useful insights about trends in hospital discharges in the United States in regard to serious mental illness. Nevertheless, caution should be used in interpreting the results of this analysis because the trends for discharges involving serious mental illness were for general hospitals only.
Discussion
We examined the most recent data from the National Hospital Discharge Survey (1995 to 2002) to investigate whether the trend in general hospital discharges that involved serious mental illness had continued to increase. For further insight, we also examined trends in hospital discharges involving serious mental illness in relation to hospital and patient characteristics and geographic regions.
Although increases in the expenditure, availability, and volume of mental health care were observed (
6 ), there is little evidence that the prevalence or severity of mental illness increased in the United States. Data from the NCS and the NCS-R indicate that the prevalence of mental disorders did not change from 1990 to 2003 (24.9% between 1990 and 1992 compared with 30.5% between 2001 and 2003) (
5 ). However, the rate of treatment for mental disorders increased significantly, from 20.3% between 1990 and 1992 to 32.9% between 2001 and 2003 (
5 ). As mentioned previously, data from the National Hospital Discharge Survey and the Inventory of Mental Health Organizations also showed an increase in psychiatric inpatient care from 1988 to 1994 (
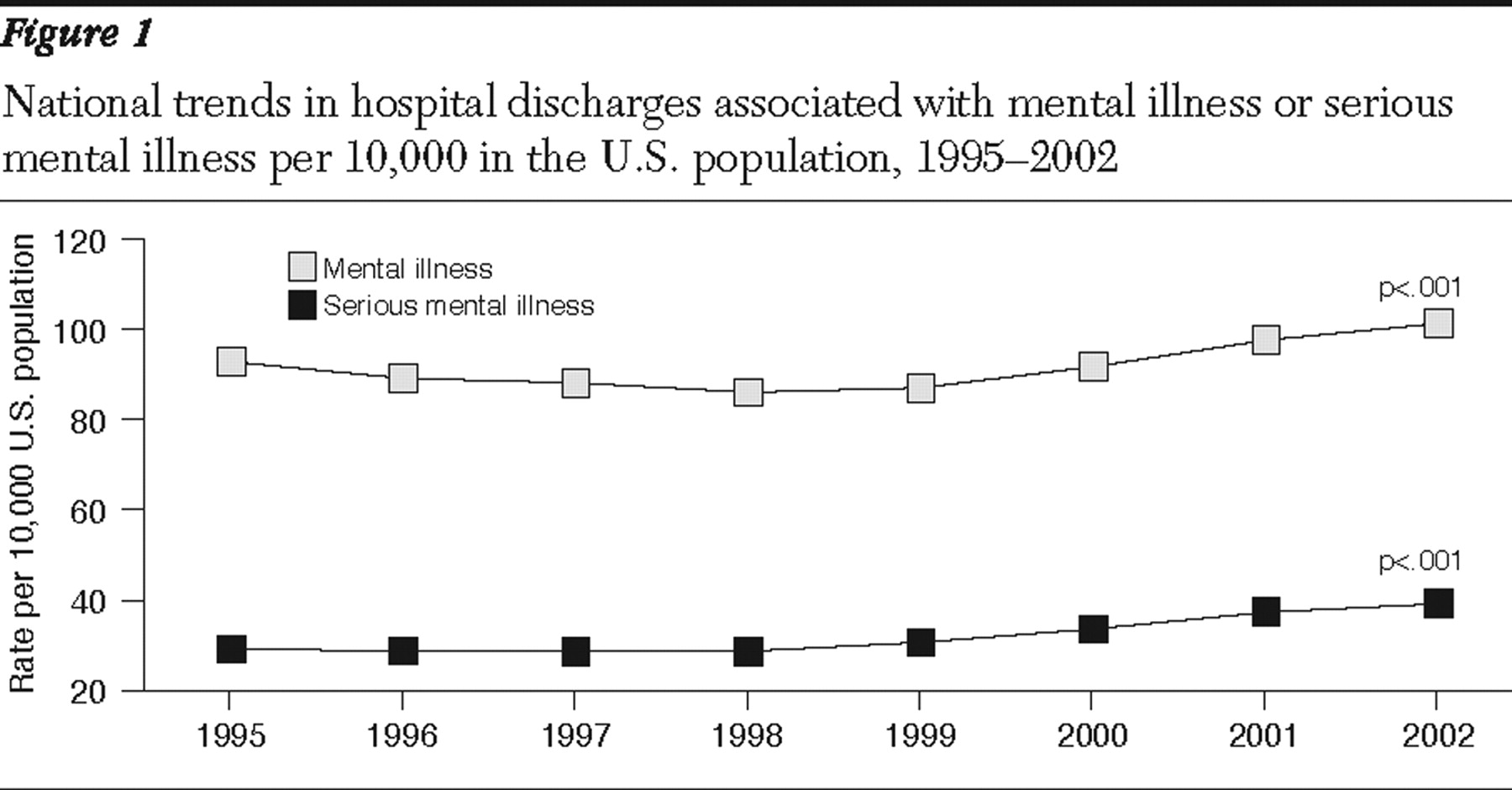
7 ). Our analysis of data from the National Hospital Discharge Survey from 1995 to 2002 confirmed that general hospital discharges for mental illness continued to increase significantly.
The Center for Mental Health Services reported that the number of nonfederal general hospitals with separate psychiatric services increased from 1,674 to 1,707 between 1990 and 1998. However, the number dropped to 1,373 in 2000 (
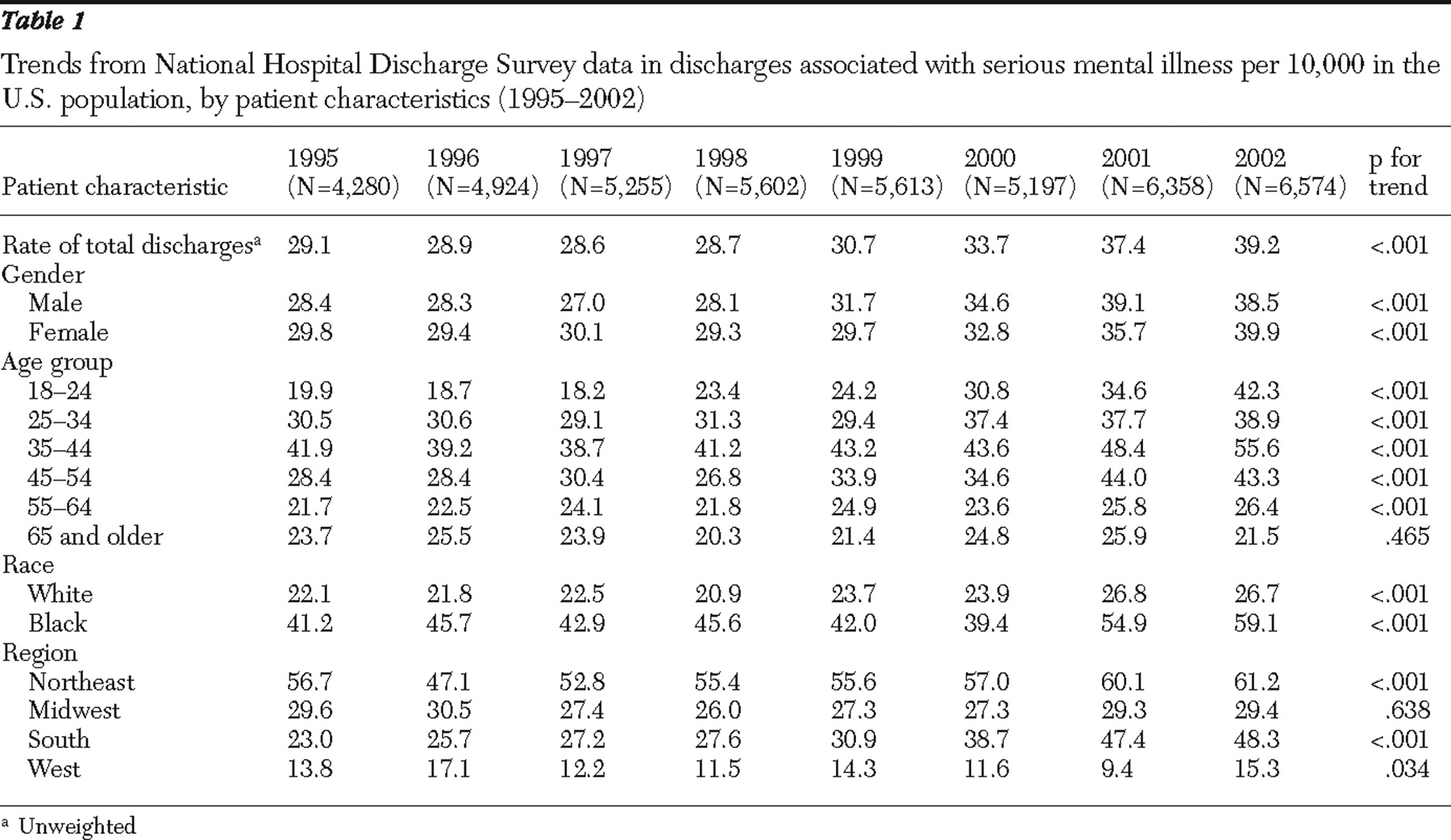
6 ). Our analysis of National Hospital Discharge Survey data for the period of 1995 through 2002 found that the increase in general hospital discharges associated with serious mental illness continued through 2002. The annual number of adult hospital discharges involving serious mental illness increased from 29.1 discharges per 10,000 in the U.S. population in 1995 to 39.2 discharges per 10,000 in the U.S. population in 2002. A closer look at the trend reveals that the discharge rate did not start rising until 1998; between 1995 and 1998 the discharge rate was relatively stable.
While the general hospital discharge rate for serious mental illness increased significantly between 1995 and 2002, the average length of stay declined from 12.8 days in 1995 to 9.7 days in 2002. The decreasing trend in psychiatric length of stay has been observed for more than a decade. For instance, studies by the American Hospital Association showed that the average length of stay in psychiatric hospitals declined between 1988 and 1992 (
14,
15 ). Mechanic and colleagues (
7 ) found that length of stay for mental illness in general hospitals also declined from 1988 to 1994.
For the purpose of programming and policy development that seeks to ensure the availability of and accessibility to psychiatric care for people with serious mental illness, it is important to identify characteristics of patients who are most likely to use services. In our study, a large increase in hospital discharges involving serious mental illness was found among young adults. Among people of ages 18 to 24 years the discharge rate increased more than twofold from 1995 to 2002. This finding corroborates findings from a study that examined data from the National Hospital Discharge Survey for children and adolescents and found that between 1988 and 1995, the general hospital psychiatric discharge rate increased significantly in the six- to 18-year-old group (
16 ). However, another study by Martin and Leslie (
17 ) found that the proportion of youths with an inpatient psychiatric admission decreased by 23.7% from 1997 to 2000 and that annual inpatient and outpatient costs decreased by 18.4% and 14.4%, respectively. The investigators also observed that the mean annual medication-related costs per outpatient increased by 12.1%. Therefore, it is not clear whether the increasing trend in service use among younger adults is specific to general hospitals or is a phenomenon seen across different types of mental health facilities.
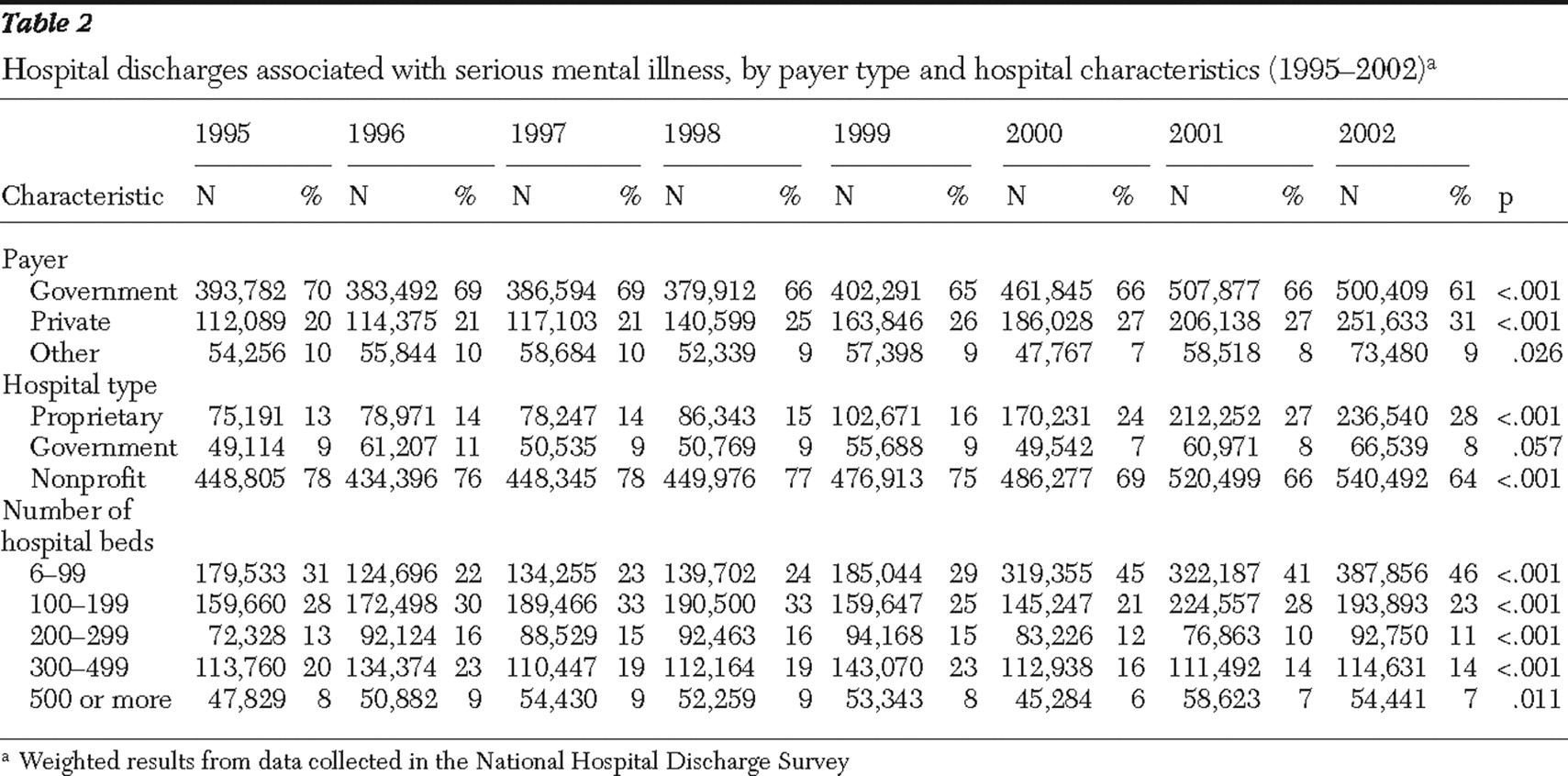
The examination of the trend for payer type and hospital characteristics revealed that government sources were associated with significantly fewer discharges (60.6%) in 2002 than in 1995 (70.3%) and that private sources were associated with more discharges (30.5%) in 2002 than in 1995 (20.0%). Regarding hospital type, the percentage of discharges from proprietary hospitals increased from 13.1% in 1995 to 28.0% in 2002. Mechanic and colleagues (
7 ) found that general hospital discharges increased most in private nonprofit hospitals and declined substantially in public hospitals. However, public programs have increasingly replaced private insurance as the major source of payment.
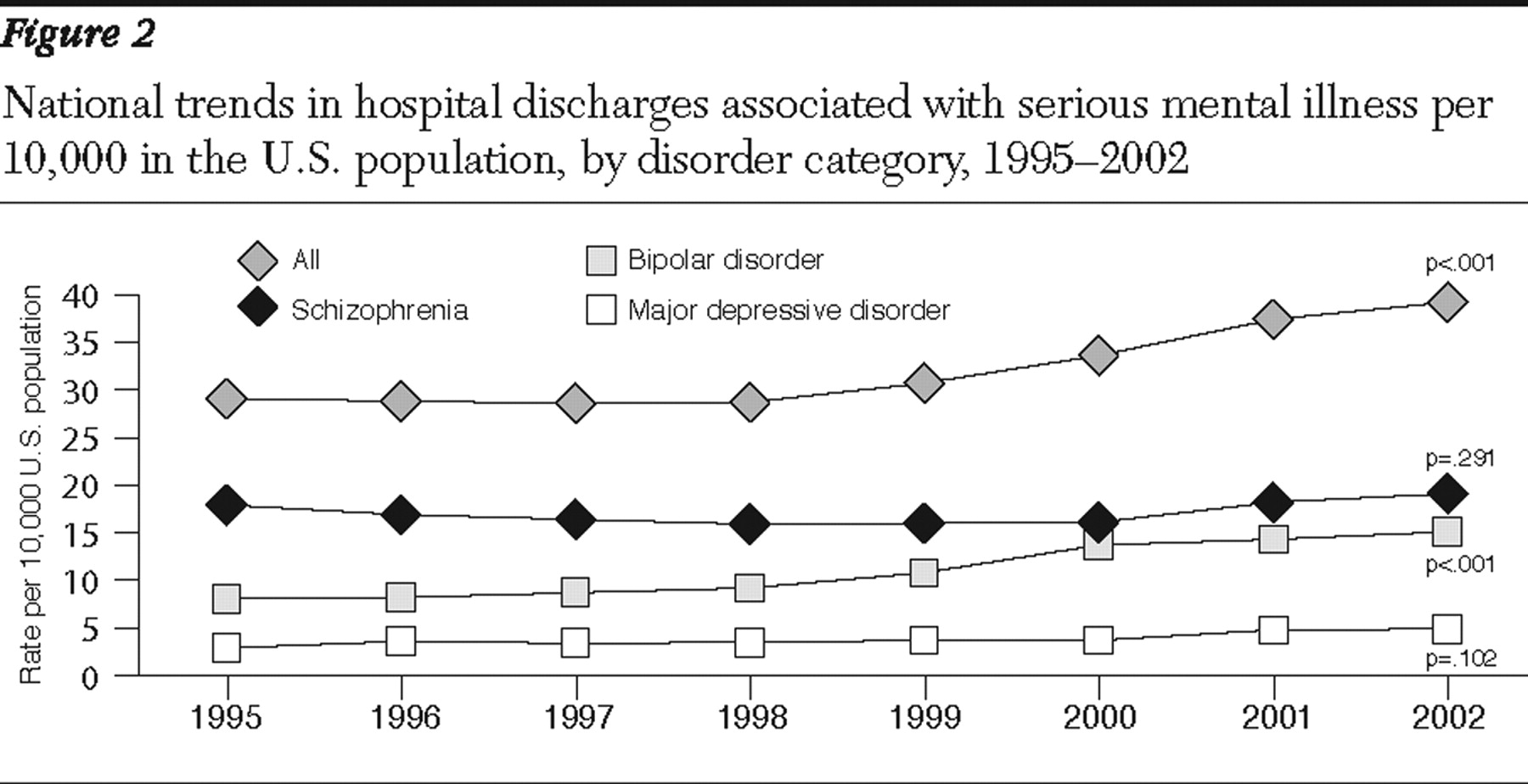
The trends for specific serious mental illness suggest that the increase in discharges for bipolar disorder may have contributed to the overall increase in the discharge rate for serious mental illness in the U.S. population. Schizophrenia and bipolar disorder are more likely to be misdiagnosed than other psychiatric illnesses because they have many variants and clinicians have to rely on phenomenological syndromes rather than on pathophysiologic origins for diagnosis (
18,
19 ). Further, compared with mental health specialists, other health specialists are more likely to misdiagnose. With the arrival of the newest generation of serotonin reuptake inhibitors, primary care providers began playing a more central role in diagnosis and treatment of anxiety and mood disorders (
19 ). It is plausible that the increase in general hospital discharges associated with bipolar disorder observed in our study is the result of an increase in diagnosis and treatment by general practitioners.
In regard to regional differences, we found that general hospital discharge rates associated with serious mental illness increased substantially in the South and Northeast regions. Findings from past studies confirm geographic variation in hospital use across the United States (
20,
21,
22,
23 ). Again, in the absence of evidence to suggest an increase in the prevalence of mental illness in the South and Northeast regions, we believe that the significant increase in the general hospital discharge rates we saw in these regions was due to factors that contribute to an increase in diagnosis or treatment for serious mental illness. As suggested by Ashton and colleagues (
23 ), factors such as geographic differences in practice patterns, supply of hospital beds, geographic unevenness in the market penetration of health care organizations, and access to care may explain geographic variability in the use of health care.
Three limitations of this study are relevant to the results reported herein. First, in our analyses, we looked at primary diagnostic codes to identify discharges from hospitalization for mental illness or serious mental illness. Although these codes tell us that a particular diagnosis for mental illness or serious mental illness was given to a patient, they do not necessarily mean that psychiatric care was given to the patient at the point of hospitalization. However, the data we used for our analyses provide insight into the pattern of health service utilization among people who have been diagnosed as having mental illness. Second, the data sources used are based on discharges, not individuals; therefore, the number and types of patients with more than one discharge in any one year cannot be determined. Third, we did not take into account changes in diagnostic practices over time and variations across different regions. Thus we could not determine how these changes or variations, if any, might have affected the findings reported here. Last, we did not make adjustments for multiple comparisons. Therefore, when interpreting the results, we need to consider the increased chance of incorrectly producing a difference (making a type I error) on an individual test.
Clarification of the implications of the results reported in this study requires more dynamic analysis of the data to identify reasons for the increase in hospital discharge rates among young adult and black populations. For example, analyses of Healthcare Cost and Utilization Project data and other population-based data on hospital discharge may be useful to confirm the findings from this study. We also recommend examining detailed clinical data to understand the differences in diagnostic and treatment patterns among various population subgroups and across geographic regions. Last, further research is needed to understand the important issue of how the patient- and system-level factors interact with each other to influence the likelihood of hospitalization among people with serious mental illness.