The psychiatric community has long recognized that there is a significant correlation between exposure to trauma and the development of psychopathology. This observation has been made in prospective studies of war veterans (
1 ), survivors of natural disasters (
2,
3 ), victims of terrorist attacks (
4,
5 ), and survivors of childhood and adult physical and sexual abuse (
6,
7 ).
Epidemiological studies document a high prevalence of trauma in the U.S. population, with associated productivity loss from posttraumatic stress disorder (PTSD) in excess of $3 billion annually (
8 ). Despite the high prevalence, many individuals do not receive adequate care for posttraumatic symptoms (
9 ). Reasons include the limited availability of services, reluctance of traumatized individuals to seek treatment, and inadequate screening (
8 ).
To explore the possibility that inadequate screening contributes to the undertreatment of posttraumatic symptoms, Eilenberg and colleagues (
10 ) conducted a chart review assessing the documentation of traumatic assessments of patients at a general psychiatric clinic. The principal findings were that although exposures to traumatic events were documented in 72 (40%) of the 180 charts reviewed, the presence or absence of common symptomatic sequelae of trauma was not recorded in a large majority of these evaluations. Specifically, symptoms of PTSD were assessed and recorded for only eight (11%) of 72 patients with a history of trauma, and the written treatment plans were deemed adequate in only seven (10%) of the charts reviewed (
10 ).
Our study is a ten-year replication of this work, designed to assess whether the increased awareness of trauma has led to improved documentation of trauma-related symptoms, diagnostic formulations, and treatment plans.
Methods
Our sample was drawn from patients who completed psychiatric evaluations from 2002 through 2005 at the same clinic that was evaluated in the initial study. The clinic is a general psychiatry clinic at an academic medical center in New York City, and it provides treatment for an ethnically diverse population with high levels of poverty, unemployment, and drug-related and domestic violence. The clinic places no restrictions on the diagnosis, financial status, or referral source of the patients. All patients who completed the clinic's initial psychiatric evaluation were eligible for the study, and 107 randomly selected charts were included. The procedures for the study were approved by the institutional review board of the New York State Psychiatric Institute.
The intake form that the clinic uses when evaluating new patients is the same as that used in the original study and contains standard questions germane to a psychiatric evaluation (history of current illness, psychiatric history, family history, and so forth). The form has a separate section mandating that evaluators ask about any history of physical or sexual abuse or other forms of trauma.
Senior psychiatric residents completed a majority of the intake forms (73 forms, or 68%); the remainder were completed by psychology interns (29 forms, or 27%) and medical students (five forms, or 5%). The sample included 15 psychiatry residents, four psychology interns, and three medical students. Each psychiatric evaluation was conducted over three separate sessions. All trainees were supervised by attending psychiatrists, who interviewed the patients with the trainees, discussed the clinical material after each interview, and reviewed the intake form. The intake forms were further reviewed and signed by the medical director of the clinic. All psychiatry residents and psychology interns working at the clinic received at least four hours of didactic training in trauma before working in the clinic. This was not a formal aspect of training when the initial study was conducted.
For the study presented here, we reviewed each intake form, using the same instrument that was developed for the original study. The first author rated each intake form, using the study instrument. Patient demographic characteristics and all
DSM-IV diagnoses were collected from the intake form. The written description of any trauma history was recorded from the section of the intake form mandating that clinicians ask about any lifetime history of physical or sexual abuse or trauma. Using the study instrument, the rater then assigned a trauma score to each intake form, from 1, no evidence of trauma, to 4, definite trauma. Patients whose intake forms had a trauma score greater than 3 were rated as having a positive history of trauma. Traumatic events were defined as physical or sexual abuse or catastrophic events with a "threat to one's physical integrity … or threat to the physical integrity of another person" (
11 ).
For each intake form documenting a positive history of trauma, the reviewer rated the thoroughness of the written description of the nature, frequency, and severity of the trauma. The reviewer then rated whether the chart contained a documented assessment of the presence or absence of trauma-associated symptoms. The symptom list was compiled on the basis of symptoms commonly associated with trauma in the psychiatric literature (
12,
13 ); they included PTSD, dissociation, somatization, self-injurious behavior, suicidality, and substance abuse. The documentation of symptoms was rated on the basis of a 3-point scale: 0, no mention of the symptom; 1, symptom noted but not fully related to the trauma history; 2, symptom noted and fully related to the trauma history.
Finally, the reviewer rated the thoroughness of the diagnostic formulation and treatment plan recorded in corresponding sections of the intake form.
DSM-IV (
11 ) and the American Psychiatric Association's consensus treatment guidelines served as a basis for comparison. For a diagnosis such as major depressive disorder with trauma as a precipitant, where there is no consensus on how to incorporate the trauma history into treatment, we rated the treatment plan as thorough if some consideration of how the trauma would be dealt with was documented; for example, "Will further discuss traumatic history with patient after treatment alliance is established."
To assess the reliability of the study instrument, 12 (22%) of the 54 charts that documented a positive history of trauma were randomly selected and assessed by a second rater who was blind to the first rater's assessments. The second rater, who developed the study instrument, was the first author of the initial study and is a psychiatrist highly experienced in trauma assessments. Ratings obtained from the second rater were compared with those from the first rater and demonstrated strong interrater reliability ( κ <.75, Cronbach's α <.75, intraclass correlation <.7, p<.001). A copy of the rating instrument is available from the first author upon request.
Results
We reviewed 111 randomly selected evaluation forms, which represented over 25% of the clinics' intakes from 2002 to 2005. Four charts were excluded because the intake form was incomplete; 107 intake forms constituted the study sample. The mean±SD age of the patient sample was 39.8±14.5 years (range 18–80). The sample included 55 (51%) Hispanic patients, 30 (28%) Caucasian patients, 19 (18%) African-American patients, and seven patients (7%) for whom no racial-ethnic information was recorded. Positive trauma histories were found in 54 (50%) of the 107 charts. The ages, racial-ethnic make-up, gender distribution, and rates of trauma were similar to those reported in the initial study. Rates of trauma in each racial-ethnic group and the forms of trauma were also similar to those reported in the original study.
The most common primary diagnoses included major depressive disorder (44 patients, or 41%), anxiety disorders (25 patients, or 23%), bipolar disorder (eight patients, or 7%), psychotic disorder (five patients, or 5%), personality disorder (nine patients, or 8%), and adjustment disorder (nine patients, or 8%). The remaining seven patients received a variety of other diagnoses. These diagnostic categories were similar to those in the initial study.
We found that compared with the charts in the initial study, the charts we reviewed were significantly more likely to contain a thorough description of the frequency ( χ 2 =27.5, df=1, p<.001) and severity ( χ 2 =21.1, df=1, p<.001) of the traumatic events. We found that 30 charts (56%) in our study contained a thorough description of the severity of the trauma, compared with 11 charts (15%) in the initial study. We also found that 32 charts (59%) in our study contained a thorough description of the frequency of the trauma, compared with 11 charts (15%) in the original study. We found no change in the proportion of charts with an adequate description of the nature of the trauma—33 charts (61%) in our study compared with 43 charts (60%) in the original study.
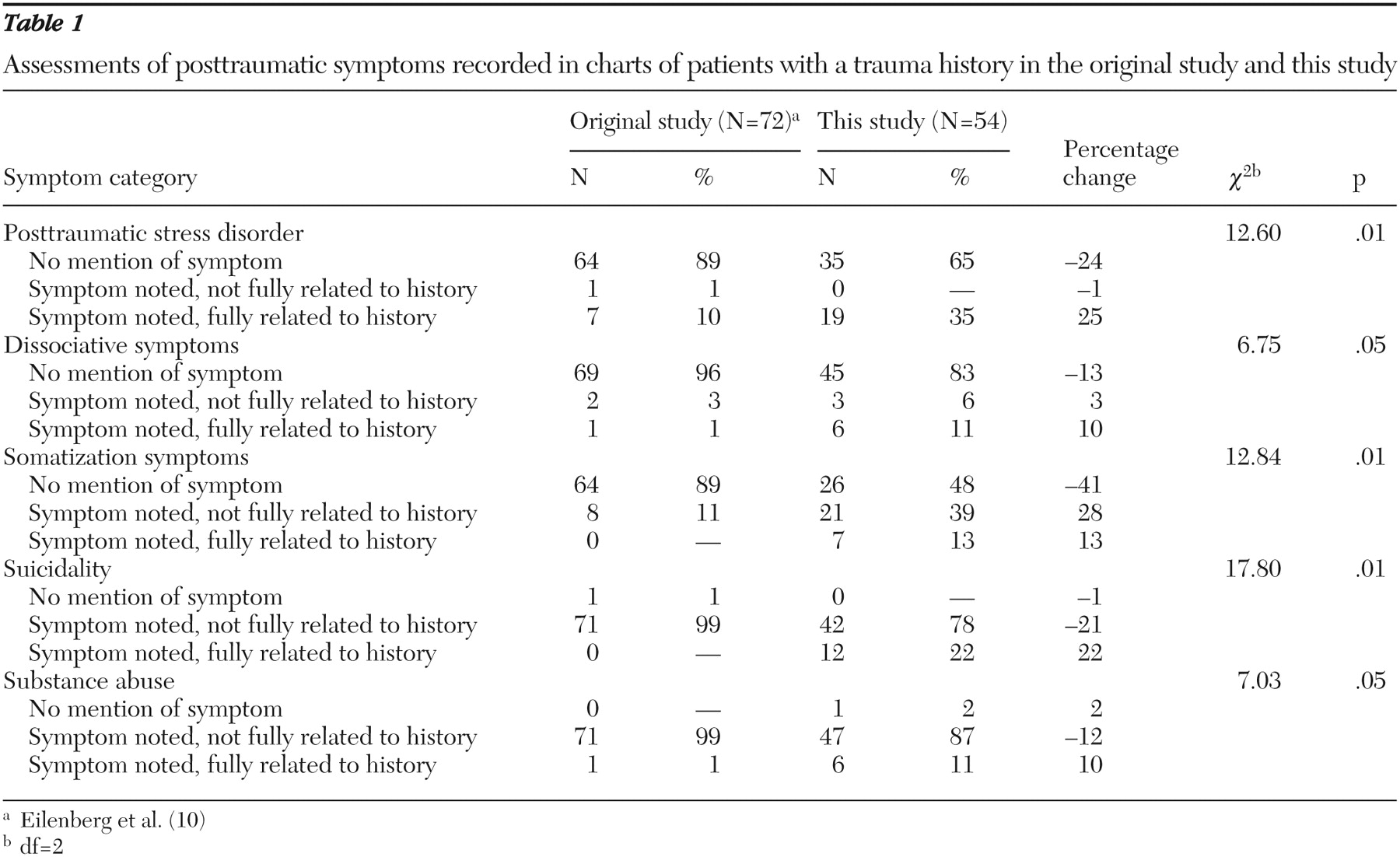
As shown in
Table 1, we also found that clinicians in our study were more likely to record the presence or absence of posttraumatic symptoms. For example, the initial study found that in 64 (89%) of the charts that documented a positive trauma history, the presence or absence of PTSD symptoms was not recorded. In our study, the presence or absence of PTSD symptoms was assessed and recorded in 19 (35%) of the charts of patients with a trauma history.
Finally, we found that eight (14%) of the charts that recorded a positive trauma history documented a thorough diagnostic formulation and five (9%) recorded a thorough treatment plan. Compared with the initial study, there was no change in the proportion of charts with an adequate diagnostic formulation or treatment plan.
Discussion
The study reported here is a replication of the work of Eilenberg and colleagues (
10 ) and was intended to assess whether documentation of trauma histories has improved over the past ten years as awareness of trauma has increased. The results of this study demonstrate significant improvements in the documentation of severity and frequency of traumatic events as well as in the recorded assessments of posttraumatic symptoms.
However, there is room for improvement. Most notably, we found that for a large majority of patients who had a trauma history, there was no recorded assessment of posttraumatic symptoms. The presence or absence of symptoms of PTSD was documented in only 19 (35%) of the charts that recorded a history of trauma. Moreover, we found no improvement in the recorded diagnostic formulations or treatment plans.
This study has significant limitations. Our assessments were restricted to the information recorded in patients' charts. Clinicians may have evaluated patients' trauma histories and symptoms during interviews without including this information in their written evaluations. Moreover, the study was retrospective, and we were therefore unable to compare the recorded rates of trauma or posttraumatic symptoms with the true prevalence. Likewise, the evaluations reviewed in this study were conducted by clinicians in training rather than experienced providers. We note, however, that all the evaluations were closely supervised by experienced psychiatrists. Furthermore, several investigators have found that trauma assessments remain deficient even when done by experienced clinicians (
14,
15 ). Finally, the generalizability of our findings is limited by the small sample as well as by site-specific factors. Clinicians at the clinic we studied received didactic training in trauma-associated psychopathology, and the clinic is located in New York City, where there is increased attention to trauma after the terrorist attacks of September 11, 2001.
Conclusions
Despite these limitations, our findings suggest that even when a trauma history is made explicit during a psychiatric evaluation, this does not lead consistently to a recorded assessment of posttraumatic symptoms. These findings are in keeping with a large body of literature suggesting that PTSD is often underdiagnosed and undertreated (
9 ). Our findings suggest that further research is needed to better understand the barriers that prevent comprehensive assessments of trauma history and how to best help clinicians overcome these barriers.
Acknowledgments and disclosures
The authors report no competing interests.