A major goal of mental health policy in the United States is to reduce barriers to service utilization. This policy focus is motivated by research documenting that most mental disorders go untreated or are treated only after extensive delays (
1 ) and that effective treatments exist for most of these disorders (
2 ). Researchers have identified a number of barriers to receiving mental health care, including financial, knowledge-related, and attitudinal barriers (
3 ). Improving our understanding of the effects of reducing these barriers on utilization is important to inform mental health policy.
The authors of prominent reports identify stigma as a key barrier to mental health care. In 1999 the U.S. Surgeon General concluded, "For our nation to reduce the burden of mental illness, to improve access to care … stigma must no longer be tolerated" (
2 ). More recently, the President's New Freedom Commission made stigma reduction its first major policy recommendation (
4 ). Considerable recent research attention also attests to the intense interest in the relationship between stigma and mental health care (
5,
6 ).
The importance of stigma as a barrier to mental health care is also consistent with theoretical models of help seeking. These models typically conceptualize care seeking as a process that is influenced by social and cultural factors and one that involves symptom appraisal (for example, perceiving a need for mental health help) as well as acting on that appraisal (
7,
8 ). Empirical research supports these models, documenting that attitudes and beliefs about mental health and treatment have significant influences on help-seeking behavior, even after the severity of symptoms are controlled for (
9 ). Recently, these models were extended to focus on perceived public stigma as a key social factor that affects care seeking (
10 ). Public stigma is defined as the extent to which the general public negatively stereotypes and discriminates against a stigmatized group, and perceived public stigma is the extent to which an individual perceives the public to stereotype and discriminate against a stigmatized group (
10 ).
Despite recent policy attention and a strong conceptual foundation, there is limited and mixed empirical research documenting how individuals' perceptions of stigmatizing attitudes by the public toward mental health care impede care seeking. Although prior research has found that perceptions of stigma reduce service use among patient samples (
11,
12 ), community-based samples are needed to assess associations between perceptions of stigma and use of any services. One recent community-based study found that participants in a 2001–2003 survey (N=4,319) were less likely than those in a 1990–1992 survey (N=5,388) to report being embarrassed if friends were to learn that they used services (
13 ). The author concluded that these changing attitudes reflect a trend of perceiving less public stigma, which may partially explain the contemporaneous increase in mental health services use. Another recent study found that negative attitudes toward help seeking (including the expectation of embarrassment) reduce the likelihood of perceiving a need for help and subsequently using mental health care (
9 ). Other community-based studies found that between 24% and 29% of individuals with an apparent need for help reported being afraid of what others might think as a reason for not seeking care (
14,
15 ). In contrast, another study that used a prospective longitudinal design and a community-based sample of Australians found no association between a single-item measure of perceived public stigma and mental health service use (
16 ).
In the study presented here we build upon this important research literature in three respects. First, we measured perceived stigma by using a multiple-item scale, rather than a single item, because stigma is generally considered a multidimensional phenomenon (
17,
18 ). Second, we focused on respondents' perceived need for help, in addition to their service utilization, hypothesizing that stigma may have an impact on either stage. This focus highlights that care seeking is a multistage process and is justified by prior research that shows that perceiving a need for help is one of the most important predictors of service utilization (
14,
19 ). Third, we evaluated the association between perceived stigma and help seeking in a newly studied population, namely, university students. This population has special significance for mental health policy, given that 50% of mental disorders develop by age 18 (
20 ) and that prior research has documented the extensive delays in seeking mental health care after the initial onset of a disorder (
1 ). Furthermore, this study improves on the lack of high-quality data related to help-seeking behavior and mental health among university students, particularly amid recent reports of poor mental health in this population (
21,
22 ).
We had three main research questions. First, what is the level of perceived public stigma regarding mental health service use in a population of undergraduate and graduate students, and does it vary by sociodemographic groups, mental health status, social contacts with mental health service users, or beliefs about mental health services? Second, to what extent is perceived public stigma associated with perceiving a need for help? We hypothesized that higher perceived public stigma is associated with a lower probability of perceiving a need for help. This would be the case if perceiving a need not only implies recognition of symptoms but also has the subjective meaning of accepting tacit membership in a stigmatized group. Third, to what extent is perceived public stigma associated with the probability of receiving mental health care? We hypothesized that higher perceived public stigma is associated with a lower probability of receiving mental health care. Students may avoid seeking care that would result in being formally labeled as having a mental disorder, thereby avoiding any potential status loss or discrimination from belonging to a stigmatized group.
Methods
Data
The data came from the Healthy Minds Study, a cross-sectional Internet-based survey administered in October 2005 to a randomly selected sample of undergraduate and graduate students at a large, Midwestern, public university. The survey yielded a sample of 2,782 students (55.4% completion rate) who completed all measures used in this analysis. Weights were constructed to adjust for survey nonresponse bias by using demographic and academic data from an administrative database for all 5,021 students recruited for the study, as well as measures of depression and mental health services use collected from a random sample of initial nonrespondents. More detailed information about the sample and nonresponse weighting methodology is available elsewhere (
19 ). All participants completed an online informed consent form after reading a description of the study. The University of Michigan Health Sciences Institutional Review Board approved all aspects of the study.
Measures
The measure of perceived public stigma regarding mental health service use was adapted from the Stigma Scale for Receiving Psychological Help, a five-item scale that has been used in other recent research (
23,
24 ). The scale was adapted to pertain to stigma associated with receiving any treatment for emotional or mental health problems, broadly defined. The scale had good internal consistency within our sample (Cronbach's alpha of .74) and was created by summing the score (0–3) for each item, yielding a continuous variable ranging from 0, lowest perceived stigma, to 15, highest perceived stigma.
We measured perceived need for help by asking respondents, "In the past 12 months, did you think you needed help for emotional or mental health problems such as feeling sad, blue, anxious, or nervous?" Mental health services utilization was measured by asking respondents whether they took any psychotropic medications or used any therapy or counseling in the past 12 months. These items were taken from the Healthcare for Communities Study questionnaire (
25 ). Depressive and anxiety disorders were measured with the Patient Health Questionnaire (PHQ), an instrument developed to screen for current major depression, other depression (including less severe depression, such as depression not otherwise specified or dysthymia), panic disorder, and generalized anxiety disorder (
26 ). Other variables in our analyses—including perceived treatment effectiveness, social contacts with treatment users, and sociodemographic characteristics—are shown in the tables and described in more detail elsewhere (
19 ).
Statistical analyses
To address the first research question, we used bivariate linear regression models to test for significant differences in perceived public stigma between sociodemographic groups and groups defined by mental health characteristics, social contacts with mental health service users, and beliefs about mental health services. To address the second research question, we used multivariate logistic regression models to assess the association between perceived public stigma and the odds of perceiving a need for services among those with probable depressive or anxiety disorders (positive PHQ screens). To address the third research question, we used multivariate logistic regression models to assess the association between perceived public stigma and the odds of using services among those with probable disorders and a perceived need for help. We also estimated these multivariate models after stratifying the sample by whether students were aged 18–22 or older than 22 (for the most part, undergraduates versus graduate students), because these groups may have very different characteristics and social contexts. All multivariate logistic regressions included as covariates gender, age group (where appropriate), race or ethnicity, U.S. versus international student, family's socioeconomic background, and depression severity (as measured by the raw PHQ score, which can range from 0 to 27). All analyses were conducted with Stata 9.0 and were weighted to adjust for nonresponse.
Results
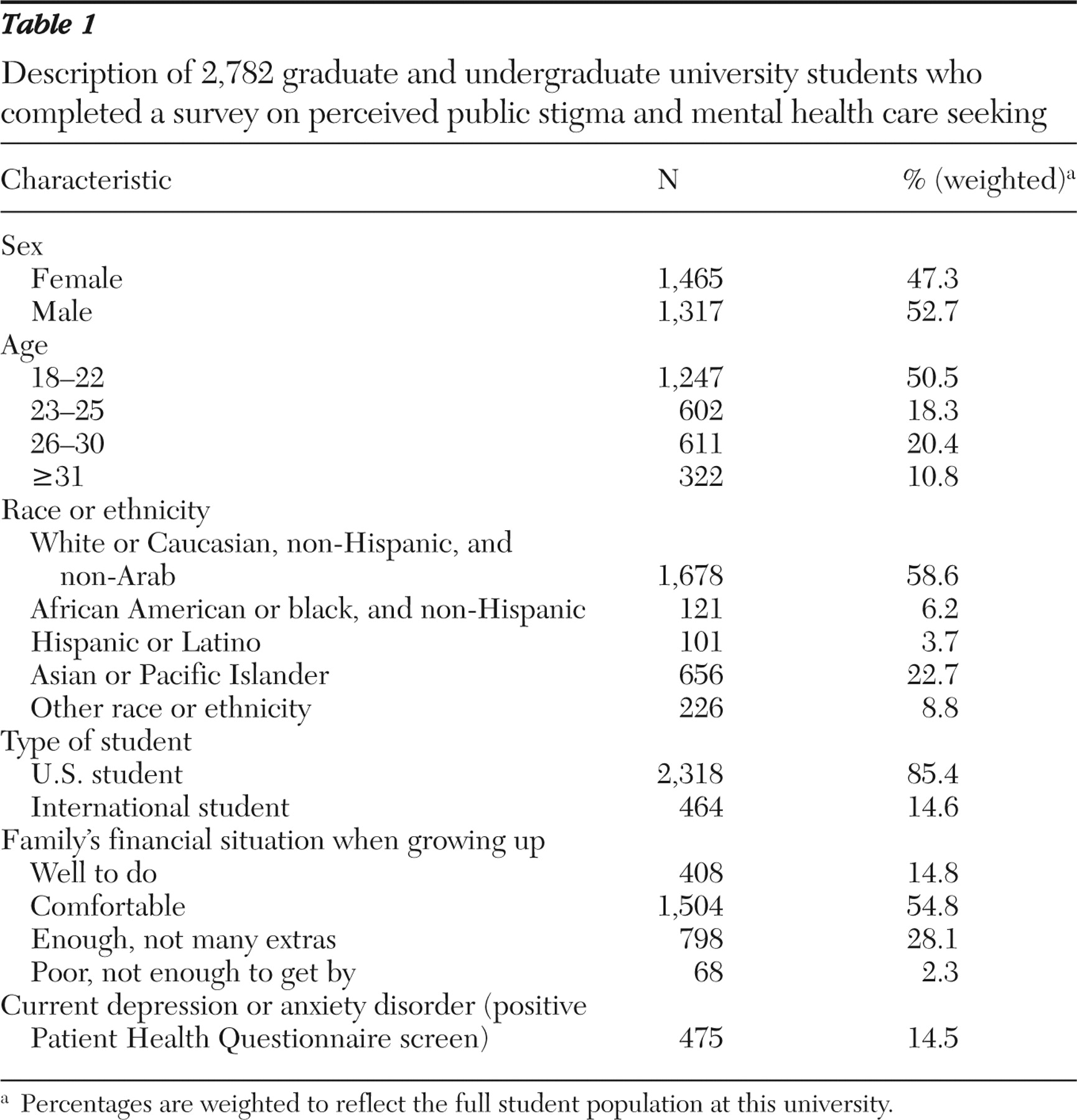
Table 1 displays the demographic and mental health characteristics of the sample. Of note, 475 respondents (14.5%) screened positive for a disorder on the PHQ (depression or anxiety). Among those respondents, 302 (65%) perceived a need for help over the past 12 months, of whom 156 respondents (52%) also utilized mental health services in the past 12 months.
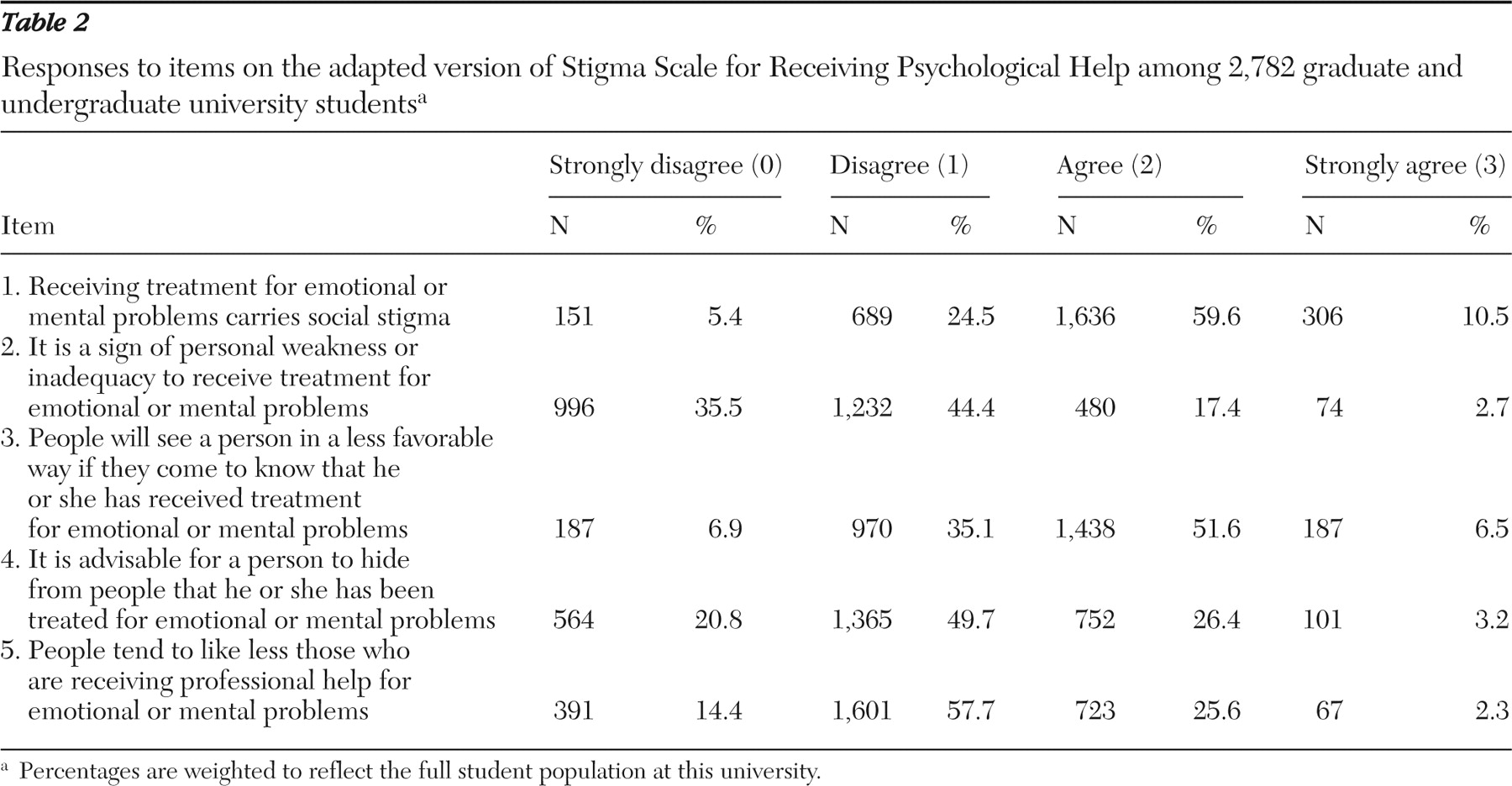
Table 2 shows the frequencies of item response for the perceived stigma scale. The mean level of perceived stigma in the study population was 6.48±2.58, below the midpoint of the scale (range of 0–15).
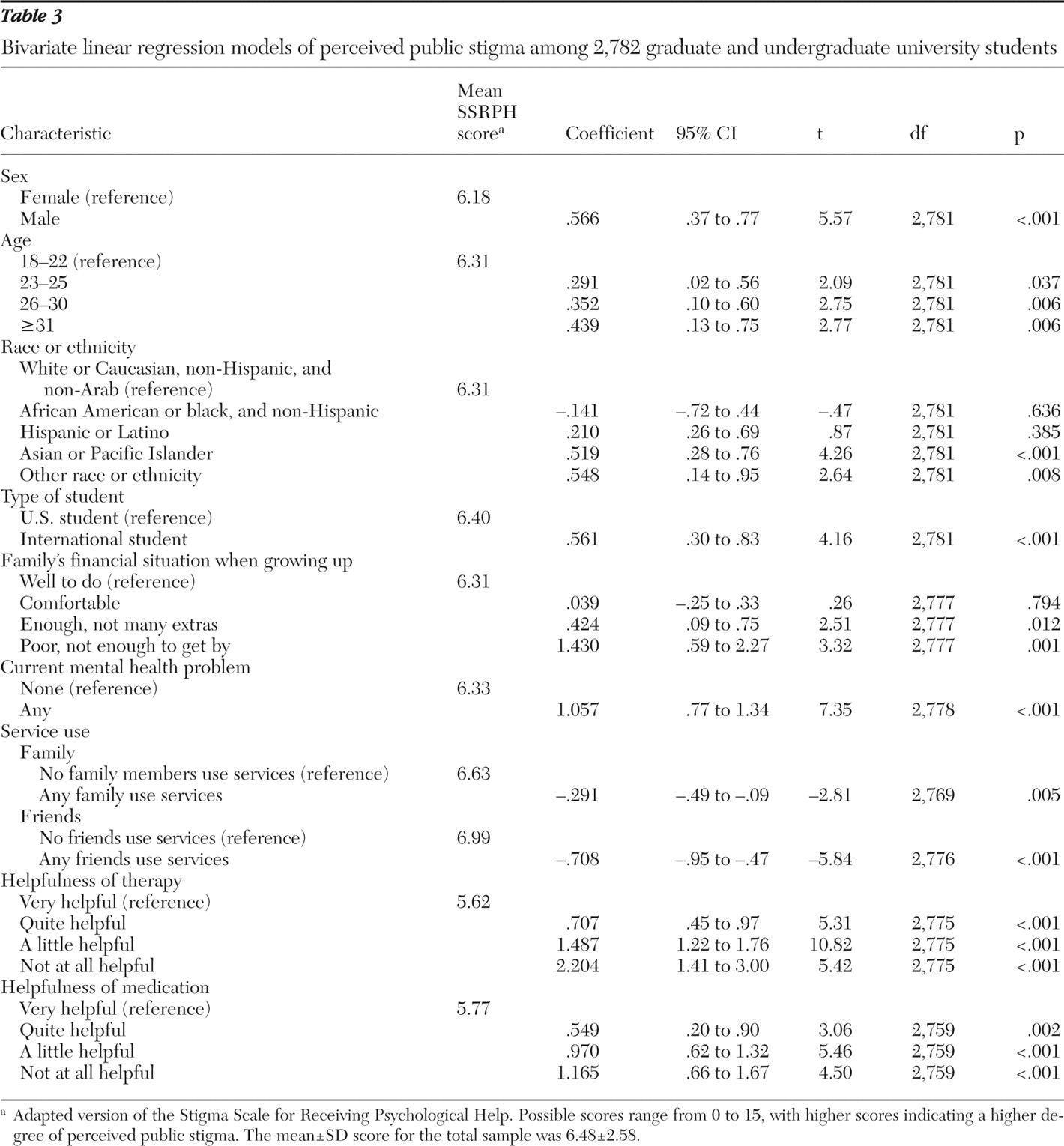
The bivariate linear regression analyses displayed in
Table 3 show that men perceived higher levels of stigma than women, older individuals perceived higher levels of stigma than younger individuals, Asian or Pacific Islanders and individuals in the "other race" category perceived higher levels of stigma than whites, and international students perceived higher levels of stigma than American students. There were also significant socioeconomic differences in perceived stigma, because those who reported coming from poor families had higher levels of perceived stigma than those who reported coming from more financially well-off families. Social contacts with service users and positive beliefs about treatment effectiveness were both significantly associated with lower perceived stigma. Having a probable depressive or anxiety disorder was significantly associated with higher perceived stigma.
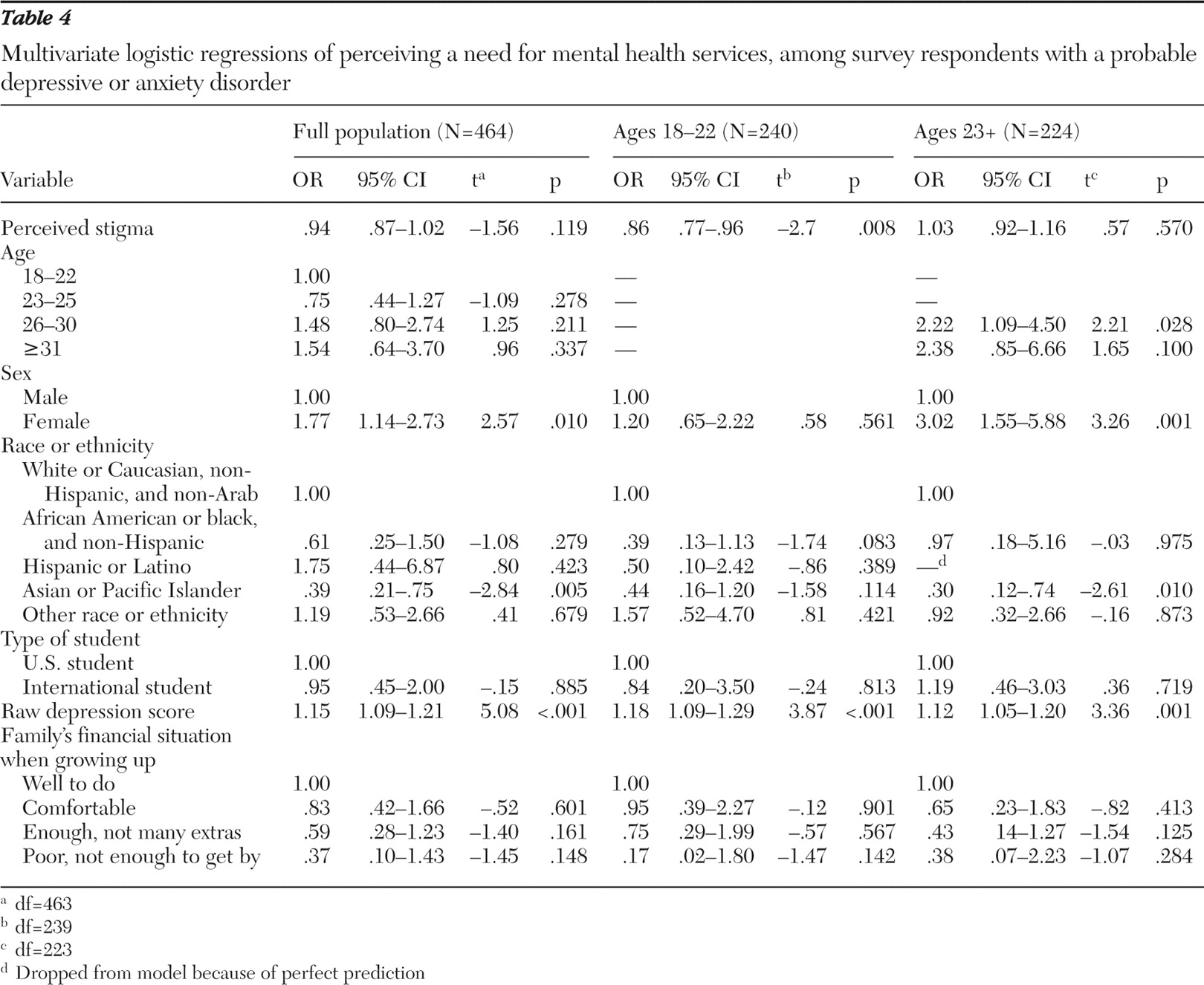
As shown in
Table 4, in the multivariate analysis of perceiving a need for help over the past 12 months among those who screened positive for a disorder on the PHQ, the odds ratio for perceived stigma was in the expected direction (OR=.94), but it was not statistically significant. Among the covariates, only being female and having a higher depression severity score significantly predicted perceiving a need for help, although Asians and Pacific Islanders were significantly less likely to perceive a need for help. After the sample was stratified by age, perceived stigma was associated with a reduced probability of perceiving a need for help among 18- to 22-year-olds (OR=.86, p=.008), but the finding was not significant among older students (OR= 1.03) (
Table 4 ).
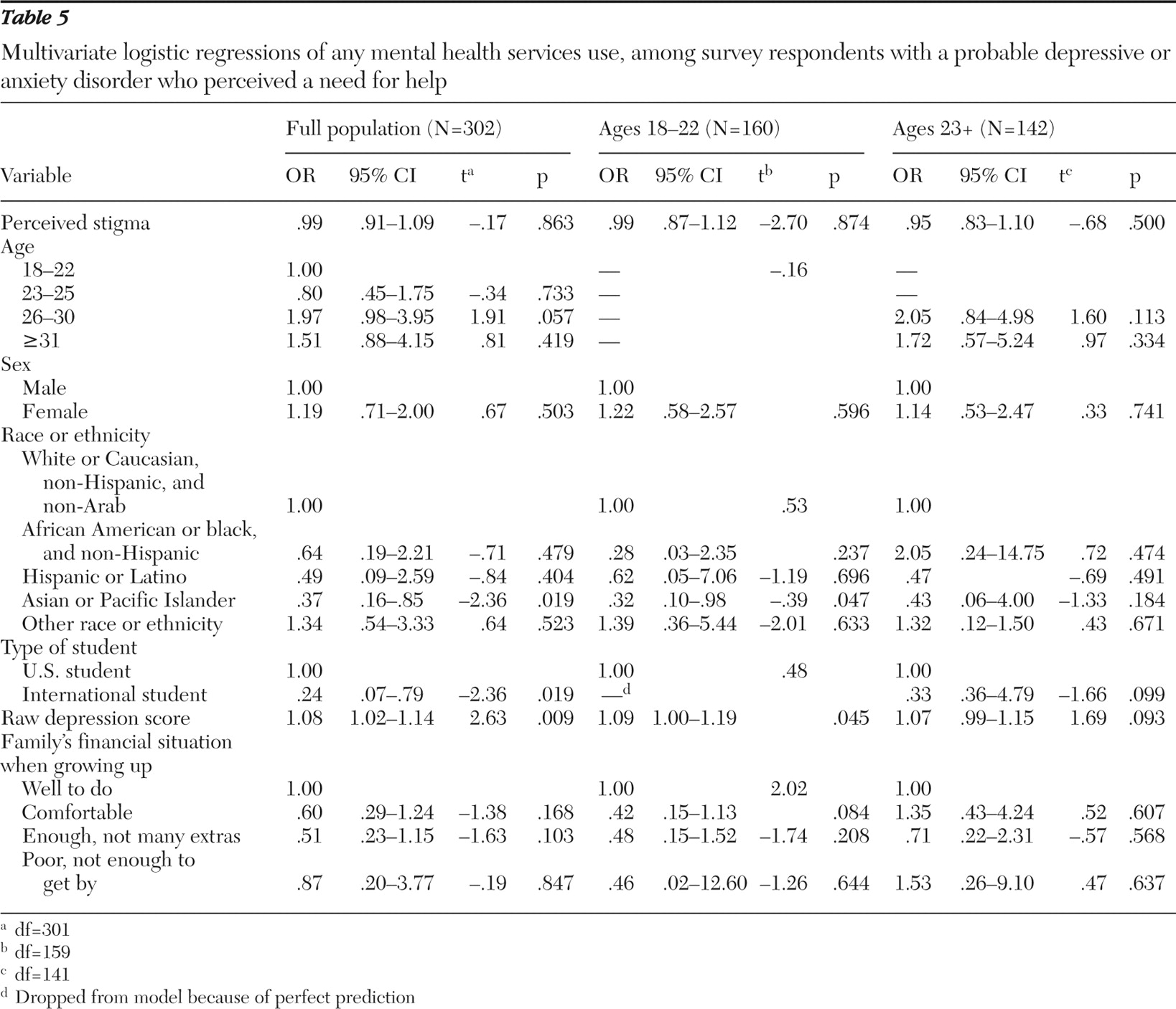
There was no relationship between perceived stigma and service use in the multivariate analysis (
Table 5 ). This was still the case after stratifying by age. Only respondents with higher depression severity scores were significantly more likely to use services, whereas Asians and Pacific Islanders and international students were significantly less likely to use services.
Discussion
Among studies of the association between perceived stigma and mental health care seeking, this study is unique in its focus on university students, its use of a representative sample of students from a university (as opposed to a convenience or clinical sample), its investigation of perceived need (in addition to utilization), and its use of a multiple-item stigma measure. We found that perceived public stigma was negatively associated with the probability of perceiving a need for help among individuals aged 18–22, but this relationship did not hold for older students. We also found that, contrary to our expectations, perceived stigma was not significantly associated with utilization. This result is consistent with results from a study that found that perceptions of discrimination toward individuals with depression were not associated with subsequent use of mental health services in a community sample of Australian adults (
16 ).
There are a variety of reasons why perceived stigma may have been associated with reduced perceived need among younger students but not among older students. Younger students are more likely to be experiencing symptoms of mental disorders for the first time. Thus they may be less likely to have already accepted a tacit label of having a mental disorder, or they may be more resistant to accepting the tacit label. An alternative explanation may be that the older students in our sample were mainly graduate students, who are a unique population in terms of education level and other unobserved qualities that may modify the relationship between perceived public stigma and help-seeking behavior. Future research on more diverse populations will improve our understanding of how and why this relationship varies between groups.
We found moderate levels of perceived stigma toward mental health services overall. In comparison, data from the National Comorbidity Survey–Replication indicate that 35% of American adults reported that they would be embarrassed if friends were to know that they received professional help (
13 ). Another study of college students that used a comparable scale found somewhat lower levels of perceived stigma than we did (mean score of 5.79 versus 6.48 on the Stigma Scale for Receiving Psychological Help) (
23,
24 ). However, this difference in perceived stigma could be explained by the study's use of a convenience sample of psychology students, in contrast to our random sample.
Levels of perceived stigma in our sample differed by gender, age, race or ethnicity, nationality, and socioeconomic background. These findings may be useful for identifying groups to target for interventions to reduce stigma. Additionally, the finding that levels of perceived stigma varied by perceptions of the effectiveness of mental health treatment and by social contacts with mental health services users suggests that these factors may be important to address in stigma-related interventions.
This study has several limitations. First, we cannot infer causal relationships from this cross-sectional study, because of possible reverse causation and unobserved confounders. Furthermore, the interpretation of our results is complicated because we used a 12-month reference period for our measures of perceived need and service use, while using measures of current perceived stigma and current depression and anxiety. As such, our interpretation may mask heterogeneity within important subgroups. For instance, we assumed that students with a positive PHQ screen who reported service use in the past 12 months were those who recently entered needed treatment; we hypothesized that low levels of perceived public stigma contributed to their decision to seek care. However, this group may also include individuals who sought treatment that was unsuccessful in reducing their depressive symptoms. Such individuals may perceive more stigma after an unsuccessful treatment episode. Lumping these two subgroups together may explain our lack of association between stigma and service use. Future work using longitudinal data and more comprehensive measures of the timing of mental disorders and service use will address this limitation more effectively.
Second, although the multiple-item measure of perceived stigma toward mental health treatment is an improvement over single-item measures, it does not specifically measure stigmatizing attitudes toward mental illness, nor does it assess structural stigma, which can impose macro-level barriers to care—for example, less generous insurance coverage for mental health services (
17 ). Future research that evaluates other aspects of stigma will enhance the understanding of how stigma influences mental health care. Third, certain items in the measure of perceived stigma (items 2 and 4 on the Stigma Scale for Receiving Psychological Help) may assess respondents' own stigmatizing attitudes, to a certain extent, rather than purely measuring perceived public stigma. Our results, however, proved robust to sensitivity analyses (not shown) that excluded these items from the perceived stigma scale. Fourth, the measures of service utilization focused exclusively on mental health care that was delivered by a physician or other mental health professional, whereas our measure of perceived need for help did not explicitly distinguish between professional and informal sources of help. Prior research has shown that utilization studies can be improved by also measuring informal sources of help for emotional or mental problems, such as clergy, family, or friends (
27 ).
A final limitation relates to generalizability. This study population predominantly consists of young adults pursuing higher education and generally has higher socioeconomic status than the general population. Younger people and those with higher socioeconomic status may demonstrate a different relationship between stigma and mental health care than older groups or groups with lower socioeconomic status. A recent study found that perceived stigma was associated with increased treatment discontinuation among older patients, but not younger patients, with depression (
11 ). We must compare our findings with those from similar studies of other populations before coming to broader conclusions about the relationship between stigma and mental health services use. Nevertheless, because half of young adults attend postsecondary education (
28 ), this study population has some relevance for young adults in general.
Despite these limitations, this study has several strengths. Few studies of levels of perceived public stigma toward mental health services have used a nonclinical sample that is representative of its study population. In addition, although other researchers have focused on individuals' self-report of their own stigmatizing attitudes, individuals' perception of public stigma may be as important a barrier to mental health care (
5 ). This study population is also important because there is a lack of studies that are representative of university students and because young adulthood is a sensitive period for the onset of mental disorders. Facilitating timely access to mental health care in this population may therefore yield substantial improvements in mental health status. Furthermore, this population is particularly interesting from a policy perspective. Financial factors, such as lack of insurance, are some of the most important barriers to seeking mental health care (
29 ). However, there is nearly universal (94%) health insurance in our study population, and at least some mental health resources are available to all students at no charge through on-campus counseling and health services. Therefore, this research may provide hints about perceived stigma's role as a barrier to mental health services after financial barriers have been reduced (as advocates of mental health parity desire).
Our findings raise the question of why there were no observed significant associations between perceived stigma and use of mental health care. One explanation is that many respondents had confidence that their service use would remain confidential and could thus avoid the consequences of being labeled as having a mental disorder. An alternative explanation is that our data represent a younger cohort for whom stigma may be a lesser barrier to care because of stigma reduction efforts and increased awareness about mental disorders and treatments during this group's developing years (
1 ). Understanding more about why there is no strong association between perceived stigma and service utilization in this population is a promising direction for future research and may lead to lessons for reducing stigma's role as a barrier to care in other populations.
Conclusions
Although this study is limited in its ability to make causal inferences, the results suggest that among university students, perceived stigma toward mental health treatment may not be as strong a barrier to using mental health services as the current policy discourse assumes. This is not to suggest that this study tells the whole story about the overall effects of stigma for people with mental disorders, nor does it suggest that stigma associated with mental illness or mental health services is unimportant for policy. Regardless of its effects on help-seeking behavior, stigma represents a form of discrimination and has been shown to have significant negative social, psychological, and clinical consequences for people with mental illness (
10,
17 ). However, this study implies that if the policy objective is to facilitate the use of mental health services among university students, other interventions that improve knowledge of and availability of services, which have been shown to be key barriers in university populations (
19 ), may hold more promise than reducing the stigma associated with mental health service use.
Acknowledgments and disclosures
Funding was provided by grant 1069.II from the Blue Cross Blue Shield Foundation of Michigan. Funding was also provided from the University of Michigan through grant OVPRE 10000 455200 from the Office of Vice President of Research; through grant C112871 from the School of Public Health, Rackham Graduate School; through the McNerney Award in the Department of Health Management and Policy; and through the University of Michigan Depression Center Innovation Fund. The authors gratefully acknowledge assistance designing and implementing the survey from Jennifer Hefner, M.P.H., and helpful comments from Paula Lantz, PhD., Joanna Kempner, Ph.D., and Kara Zivin, Ph.D.
The authors report no competing interests.