Sexual trauma sustained during active military duty is a widespread and growing concern throughout the Veterans Health Administration (VHA). The annual incidence of sexual assault among active duty personnel is 3% among women and 1% among men. Sexual coercion (for example, quid pro quo promises of job benefits or threats of job loss) and unwanted sexual attention (for example, touching, fondling, or threatening attempts to initiate a sexual relationship) occur at an annual rate of 8% and 27%, respectively, for women and 1% and 5% for men (
1 ).
Research with female veterans of the Gulf War (1990–1991) found that rates of sexual assault (7%), physical sexual harassment (33%), and verbal sexual harassment (66%) were higher than those typically found in peacetime military samples, suggesting that exposure to such experiences may be more prevalent during times of combat (
2 ). Given the longer deployments and increased stressors associated with the current conflicts in Iraq and Afghanistan relative to the Gulf War, recent veterans could report even higher rates of sexual assault and harassment. The expanded role of the U.S. military, including members of the Reserves and National Guard, in meeting the national security needs posed by war in Iraq and Afghanistan, makes identification and treatment of veterans who experience deployment-related stressors, including sexual violence, a key focus for the nation's largest integrated health care system.
VHA has adopted the term "military sexual trauma" to refer to severe or threatening forms of sexual harassment and sexual assault sustained in military service. Nationwide policy requires universal screening and documentation of military sexual trauma in the patient's electronic medical record. When the electronic medical record is called up during an inpatient or outpatient health care visit, a clinical reminder appears if the patient has never been screened. The reminder prompts the provider to administer a two-item screen for military sexual trauma. The provider enters the responses directly into the electronic medical record. Designated coordinators for sexual trauma services at each VHA establishment facilitate treatment for sexual trauma when providers determine clinical need among patients that screen positive. VHA facilities screen in mental health and primary care treatment settings (
3 ). Performance monitoring indicates that 86.7% of all VHA patients have been screened for military sexual trauma as of fiscal year 2006 (
4 ), suggesting that the program is feasible and acceptable to patients and providers. This universal screening program represents one of the most comprehensive responses to sexual violence of any major U.S. health care system.
A thorough response is necessary because sexual trauma often goes undetected. Only 26% of sexual assaults in the United States are ever reported (
5 ), and victims are less likely to disclose when the assailant is an acquaintance, coworker, or intimate partner. Studies in civilian health care settings suggest that sexual violence is rarely spontaneously disclosed to health care providers (
6 ) and that universal screening may be an effective and nonstigmatizing means of detection (
7 ). Universal screening may be an especially important detection method for male patients, for whom sexual trauma is rarely a focus of provider attention. Better detection of military sexual trauma is intended to facilitate access to appropriate treatment and prevent the long-term deleterious health consequences associated with sexual violence.
Although not all VHA patients who screen positive for military sexual trauma require mental health treatment, men and women with positive sexual trauma screens are approximately three times more likely than those with negative screens to be diagnosed as having a mental disorder (
8 ). The most common conditions associated with military sexual trauma are depression, posttraumatic stress disorder (PTSD), substance use disorders, and anxiety disorders (
8,
9,
10 ). A variety of effective behavioral and pharmacological treatments are available, and utilization of mental health services following detection of sexual trauma could prevent or treat these mental health consequences. A key indicator of the clinical utility of the VA's national health care system to address this issue is the extent to which detection of military sexual trauma is associated with access to mental health treatment among patients who might otherwise not receive needed care.
The primary aim of this investigation was to evaluate the national efforts to screen for and treat military sexual trauma. In order to address this aim, we prospectively examined rates of mental health utilization in the three-month period after screening. We then compared rates of mental health service use among patients who screened positive for military sexual trauma and those who screened negative. The extent to which change in utilization among patients with positive screens exceeded change in utilization among patients with negative screens represents the effect size associated with the detection of sexual trauma. Because some screening studies have found that patients who have previously received mental health treatment may be more likely to follow up on treatment recommendations after screening (
11 ), we examined the treatment associated with screening separately for patients with and without mental health service utilization in the six months before the screening.
Our primary research question focused on patients without a history of mental health service use. Among this population, if detection of sexual trauma via screening is associated with subsequent mental health care, results would suggest that screening was associated with improved access to mental health care. A secondary research question focused on mental health care among patients with a recent history of mental health service use. Sexual trauma may remain undisclosed among patients who have sought treatment for other conditions. Even if previously disclosed, the documentation of sexual trauma in the medical chart associated with the screen may increase the likelihood of referral to appropriate services. Similar effects for screening regardless of service use history would lend greater support for universal screening. If the benefits of screening are limited only to patients without prior care, more targeted screening efforts are indicated.
Methods
Study population
After approval of the study protocol by the Stanford University School of Medicine Institutional Review Board, we extracted all screening data on military sexual trauma obtained via VHA clinical reminders in fiscal year 2005. VHA reported that approximately 86.7% of all patients have been screened (
4 ). Prior research suggests that patients who have not been screened are atypical users who use significantly fewer VHA services than screened patients (
8 ). Therefore, we excluded unscreened patients from the study as inappropriate for comparison with screened patients on utilization rates. We identified 573,640 veteran patients with valid positive or negative responses to military sexual trauma screening and at least one outpatient encounter 180 days before or after the screening date as identified by the Department of Veterans Affairs (VA) Outpatient Events File (
12 ) to verify VA service use.
Key variables
The VHA clinical reminder contains the following items: "While you were in the military … a) Did you receive uninvited and unwanted sexual attention, such as touching, cornering, pressure for sexual favors, or verbal remarks?; b) Did someone ever use force or threat of force to have sexual contact with you against your will?" Evaluation of these items against clinical interview yielded a sensitivity of .92 and specificity of .89 for the first item and a sensitivity of .89 and specificity of .90 for the second item (
13 ). The methods of evaluation and accuracy of this instrument are comparable to other widely used VHA mental health screens for depression (
14 ) and PTSD (
15 ). The screen codes patients who respond affirmatively to either screening item as positive for military sexual trauma. These discrete events are combined because sexual trauma is considered a duty-related hazard, similar to combat exposure. This occupational exposure framework accounts for the context of the unwanted sexual activity, as well as the events, and it demonstrates good construct validity (
16 ). The clinical reminder is administered for the purpose of health care delivery and treatment planning (that is, VHA) and is not associated with the process of pursuing disability compensation (that is, Veterans Benefits Administration).
Outpatient mental health services were defined as VA encounters coded as specialized mental health or substance abuse treatment clinics. We defined prescreen mental health care conservatively as one or more mental health visits in the six months before the screening for military sexual trauma. Postscreen mental health treatment was defined as having one or more mental health visits in the three months after the screening. We aggregated postscreen visits over a shorter period to limit analyses to visits most likely to be screening related.
Statistical analysis
Statistical analyses were performed with SAS (version 9.1.3). Statistical significance was set at p<.05. Patients with positive screens were compared with those with negative screens. Results were stratified by gender and prescreen mental health service use. The relative risk (RR) and 95% confidence interval (CI) were calculated as measures of the relationship between screening status of military sexual trauma and postscreen service use among patients with positive screens. To account for the potential confounding effects of age and race in the relationship between screening results of military sexual trauma and mental health service use, we also calculated the adjusted RR. Adjusted results did not significantly differ from unadjusted RRs and are not reported. We calculated the number needed to screen (
17 ) to indicate the number of positive military sexual trauma screens required for one additional patient to be treated. All analyses were conducted separately for men and women. Nonoverlapping CIs for both the RR and number needed to screen were considered to be statistically significantly different.
Results
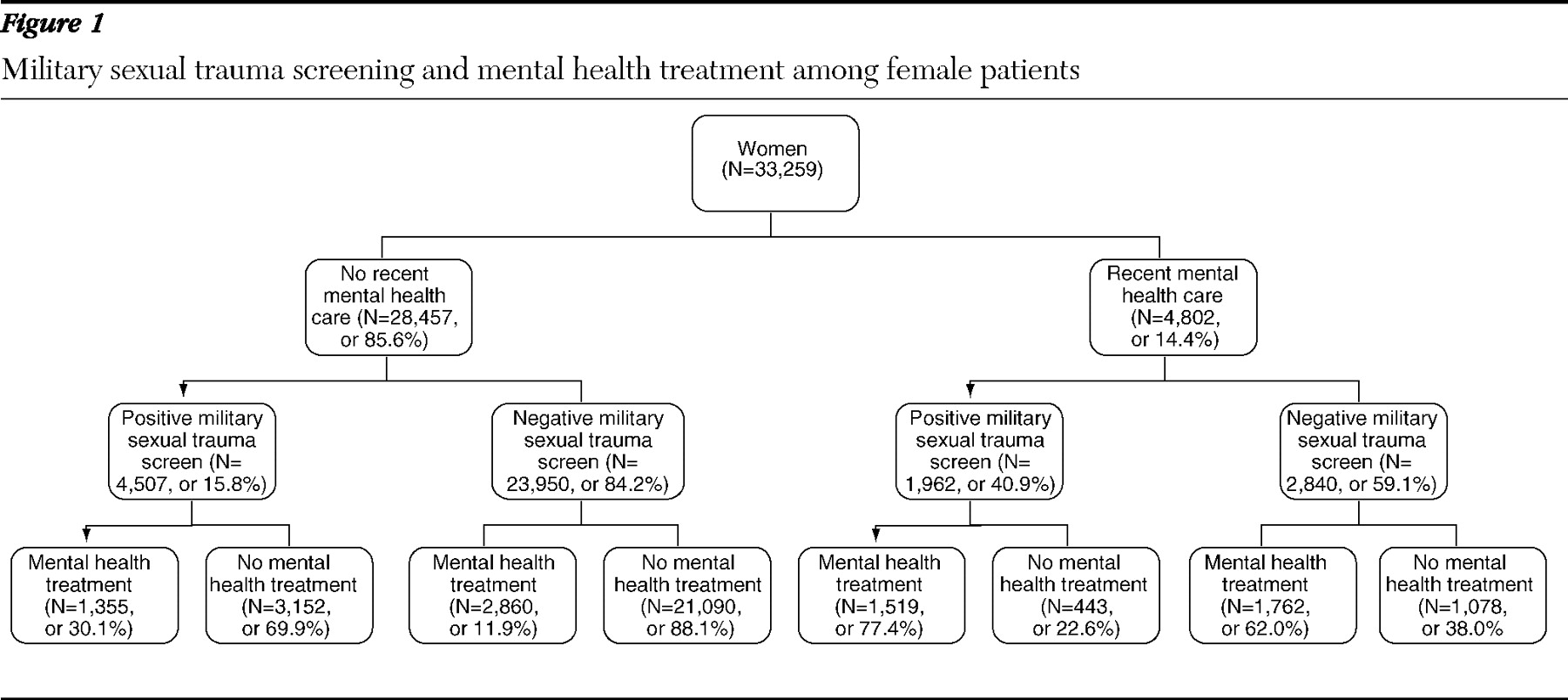
A total of 33,259 women and 540,381 men were screened for military sexual trauma, with rates of positive screens at 19.5% and 1.2%, respectively. Most individuals had not received recent mental health care in VHA, including 28,457 women (85.6%) and 487,334 men (90.2%).
Figures 1 and
2 illustrate screening and subsequent treatment among patients with and without recent mental health care.
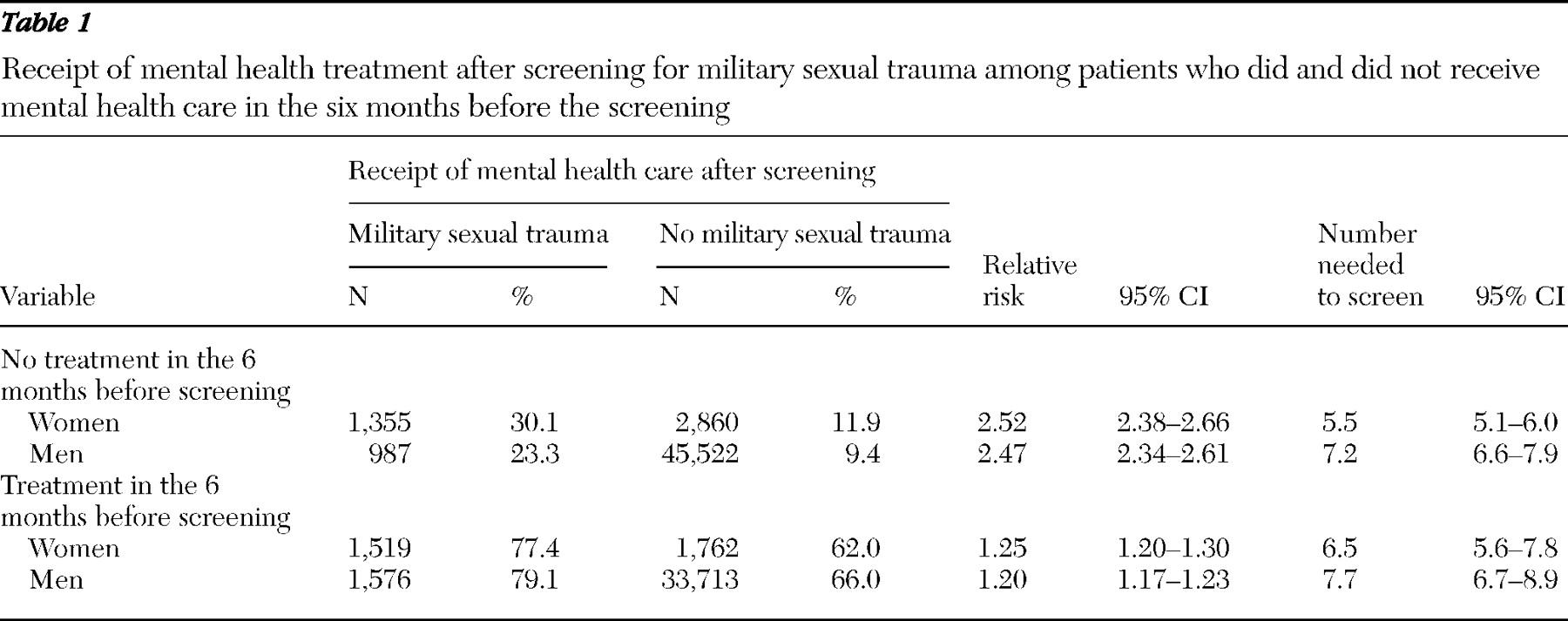
Table 1 illustrates the association of positive military sexual trauma screens to mental health treatment in the 90 days after screening among patients with no recent mental health care. For both women and men, a positive military sexual trauma screen was associated with over twice the likelihood of postscreen mental health care, compared with negative screens. We calculated the number needed to screen to provide an impact number associated with the screening. Among women, a new patient accessed care for every 5.5 positive screens. Numbers were significantly higher for men, among whom a new patient accessed care for every 7.2 positive screens.
Table 1 also displays the results for the subset of patients with recent mental health care. For both women and men, a positive military sexual trauma screen was associated with a greater likelihood of postscreen treatment, compared with a negative screen, although effect sizes were significantly weaker than those observed among patients with no recent mental health care. Impact numbers were similar to those obtained for patients with no recent mental health care, where one patient accessed postscreen care for each 6.5 positive screens among women and each 7.7 positive screens among men. Results did not differ significantly by gender.
Discussion
Our findings strongly suggest that the VHA universal screening program for military sexual trauma has increased rates of mental health treatment among patients who screen positive for such trauma. Increased rates of mental health care among treatment-seeking patients with previously undetected military sexual trauma would be a useful impact on its own. However, the VHA screening program appears to have an even greater impact on those without a recent history of mental health service use, a group for which military sexual trauma screening may increase access to needed mental health care that would not have been otherwise obtained.
We computed the number of positive screens needed for one additional patient with military sexual trauma to access mental health care after the screening. The results, ranging from 5.5 to 7.7 across groups, suggest a very good clinical impact for universal screening. These impact numbers are commensurate with clinical effects for mental health treatment use obtained from studies of depression screening that supported U.S. Preventive Services Task Force recommendations (
18 ). Effective pharmacological and behavioral treatments for trauma-related mental health disorders exist (
19,
20 ). Research studies that build on the results presented here can determine whether the increased rates of mental health treatment after screening affect more proximal patient outcomes, such as military sexual trauma–related psychiatric morbidity and quality of life.
Our findings should be interpreted in light of several limitations. We could not conduct a randomized clinical trial because randomization to a no-screening condition is precluded by Congressional mandates and VA policy. Further, our analyses excluded the relatively small proportion of VHA patients who had not been screened for military sexual trauma. This group is fundamentally different from the majority of patients in terms of their more limited use of VHA services (
8 ). Comparisons to the screened group on service use could yield biased results, increasing the chance that we would observe an inflated association between screening and utilization of mental health services. We therefore employed a design that compared the health care of patients who screened negative and positive. The use of a prospective design, rather than a case-control design, reduces bias, and inclusion of all patients nationwide lends additional validity to the analyses.
We could not measure some factors that may affect the propensity to seek VHA mental health care, such as proximity to a VHA facility, availability of mental health treatment at the nearest VHA facility, and patient comfort with using VHA services. We could not capture information on mental health care delivered outside of the VHA system. Further, our measure of VHA mental health care could be considered conservative, because we assessed only treatment administered in a mental health setting or by a specialty mental health provider; we did not assess pharmacological treatment delivered by a primary care provider.
Although our results demonstrate increased use of mental health services after positive screens for military sexual trauma, it was not possible to prove a causal link between the screening episode and the use of mental health services. Moreover, because military sexual trauma represents exposure to violence rather than a clinical condition or diagnosis, one cannot determine whether mental health care after screening is focused specifically on symptoms associated with exposure to military sexual trauma. Despite these limitations, the significant differences noted between patients who screened positive and negative over a conservatively short time frame provide prima facie evidence that detection of military sexual trauma via screening increases rates of mental health treatment for these patients.
It is important to note that the implementation of these policies to detect and treat military sexual trauma was associated with systemwide efforts to educate patients, providers, and policy makers about detection and treatment of military sexual trauma. National training efforts were focused on screening and treatment for sexual trauma, including sensitive screening methods—for example, validating the patient's experience and offering a referral to mental health care (
21 )—and recognition of psychiatric sequelae, both of which may have resulted in a greater capacity for sexual trauma patients to receive treatment.
Military sexual trauma screening, and the associated increase in mental health care utilization, has clear utility for patients whether or not they are recent users of mental health care. Although not every patient who reports a history of military sexual trauma will experience mental health sequelae or require mental health care, a history of military sexual trauma is associated with a number of mental health conditions (
8 ). A history of military sexual trauma is also associated with physical health symptoms and medical conditions across a number of domains (
22 ). Given the evidence that many survivors of sexual trauma and other forms of interpersonal violence are unlikely to disclose the experience unless specifically asked (
6,
23 ), a patient's military sexual trauma status may be unknown to treatment providers. Screening for military sexual trauma as part of a routine medical visit is an opportunity to educate patients about mental and physical health conditions associated with a history of sexual trauma, inform them of available treatment options, and increase access to effective treatments. In this way, universal screening plays a key role in secondary prevention efforts for military sexual trauma.
Although the high rates of sexual trauma experienced by veterans during their military service has required the VHA system to respond proactively to this issue, the effectiveness of the VHA's universal screening policy for sexual trauma has relevance for civilian health care settings. Many national medical organizations and advocacy groups have recommended routine screening for intimate partner violence because of the potential for early identification and intervention (
24 ). However, the U.S. Preventive Services Task Force's recommendation statement on this issue determined that, given the lack of effectiveness data for screening programs, there is insufficient evidence to recommend for or against routine screening of women for intimate partner violence.
Although screening for military sexual trauma differs in several important ways from screening for intimate partner violence, most notably a reduced risk of immediate harm and escalation of violence given that military sexual trauma among veterans would have occurred in the past, our investigation does lend preliminary support for sexual violence screening. Future research should replicate the design of this investigation in other health care settings and with screening for other forms of interpersonal violence. Research that documents outcomes associated with the detection of violence in health care will allow health care administrators to make informed decisions about policies for routine violence screening. Given that interpersonal violence represents one of the most significant and preventable sources of mental illness among women, research that guides health care system responses to detection and early intervention for these conditions is critically important.
Conclusions
The high numbers of military sexual trauma cases detected among both male and female VHA patients underscores the contention that military sexual trauma represents a significant problem with particular relevance to the VHA. As a generation of new veterans becomes users of VHA care after military service in Iraq and Afghanistan, a critical focus will be on the impact of early detection and treatment of deployment-related stressors, such as military sexual trauma, in an effort to prevent long-term deleterious health and mental health consequences in this cohort (
25 ). Future research efforts should focus on the optimal clinical management of military sexual trauma once it has been detected, such as dissemination of evidence-based treatments (
26 ). An effective screening program that promotes the detection of military sexual trauma and access to mental health care coupled with a mental health care system that provides evidenced-based care will go far in reducing the burden of illness for those who have experienced military sexual trauma.
Acknowledgments and disclosures
This research was funded by project IAE 05-291-1 from the Department of Veterans Affairs Health Services Research and Development Service. The funding organization was not substantially involved in the design and conduct of the study; in the collection, management, analysis, or interpretation of the data; and in the preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors thank Helena Kraemer, Ph.D., for her helpful comments on earlier versions of this article.
The authors report no competing interests.