Depression carries a high social burden, with significant losses in workplace productivity and substantial reduction in quality of life (
1,
2,
3,
4 ). Standardized diagnostic tools appropriate for use in field surveys now allow for better understanding of mental health status and treatment needs (
5 ). They have not, however, been widely used for local surveillance of mental health disorders.
New York City is a complex urban environment; more than one-third of the population is foreign born, and two-thirds are nonwhite (U.S. Bureau of the Census American FactFinder database, 2000 and 2004 data). Local telephone surveys have provided estimates of the burden of nonspecific psychological distress among adults and identified very high rates of distress among Hispanic residents (
6 ). However, nonspecific psychological distress correlates with several mental disorders, including major depression, social phobia, manic episodes, and panic disorder; interpretation of these data is thus limited (
7 ). Recently published data suggest that mental health issues are a growing priority among U.S. immigrant populations (
8,
9,
10,
11,
12 ). Community-specific estimates of the prevalence of mental disorders in diverse populations are important for targeting efforts to improve both detection and care of mental illness.
We used NYC-HANES data to estimate the 12-month prevalence of major depression and generalized anxiety disorder and assessed risk factors for each condition. We also estimated and evaluated risk factors for diagnosis and treatment among New York City adults with depression and anxiety. These data can inform programs that aim to reduce the burden of mental illness in New York and other large, diverse communities.
Methods
NYC-HANES was a population-based, cross-sectional survey of New York City's noninstitutionalized adult residents (age 20 years or older). Data were collected from June to December 2004. A three-stage cluster sampling was used to capture a representative sample. In the first sampling stage, 144 geographic segments (consisting of city blocks or groups of blocks) were randomly selected, with probability proportional to a measure of size from 21,169 segments across the city. In the second stage, households in the 144 segments were enumerated, and a sample of 4,026 households was randomly selected. In the third stage, eligible adults age 20 and older within households were randomly selected on the basis of an a priori computer-generated algorithm. The target sample size of 2,000 adults ensured statistical power comparable with that of the national-level survey.
Participation included an interview to assess demographic variables (including race and ethnicity), health conditions, and behaviors and a clinical examination to obtain physical laboratory measurements. The interview consisted of a fully automated computer-assisted personal interview. Data on mental health status were collected with the World Health Organization's CIDI, a standardized instrument for assessing mental disorders according to
DSM-IV and
ICD-10 criteria. The instrument was designed for administration by lay interviewers as part of epidemiologic and cross-cultural studies (
13 ). Questions on sexual behavior and drug use were asked in an audio-computer-assisted self-interview, which provides more accurate information on sensitive questions than face-to-face interviews (
14 ). The NYC-HANES protocol was approved by the New York City Department of Health and Mental Hygiene Institutional Review Board. Detailed information on data collection and study design has been published elsewhere (
15 ).
From a total of 4,026 households approached, 3,388 completed the eligibility screening questionnaire (yielding an 84% response rate); 3,047 eligible participants were identified. Of these, 1,999 completed the interview and at least one component of the examination, yielding a cooperation rate of 66%. The final survey response rate was 55%. The CIDI was completed with 91% of participants (N= 1,817). Written informed consent was obtained from all participants after the study procedures were fully explained.
Dependent measures
The prevalence of depression and anxiety was estimated from scores generated by a computer algorithm (based on responses to the CIDI) indicating diagnoses of generalized anxiety and major depressive disorder. The CIDI has good interrater and test-retest reliability and validity (
16 ). CIDI assessments were conducted in English and Spanish. For languages other than English or Spanish, the interview was translated if trained study staff spoke the participant's language.
To assess the prevalence of mental health treatment, we asked participants the following questions: "During the past 12 months, have you seen or talked to a mental health professional such as a psychologist, psychiatrist, psychiatric nurse, or clinical social worker about your health?" and "During the past 12 months, have you taken any prescription medication that was prescribed to you to treat a mental or emotional condition?" Participants who answered yes to either question were defined as currently receiving treatment for a mental health condition.
Analysis
Survey data were weighted to account for differential selection probabilities and survey nonresponse. Weights were post-stratified to reflect New York City population totals and were adjusted further to address component- and item-level nonresponse. Analyses were performed with SAS version 9.0 (
17 ). SUDAAN version 9.0 was used to obtain standard error estimates by Taylor-series linearization (
18 ). Prevalence estimates were age adjusted to the 2000 U.S. standard population. Relative standard errors and 95% confidence intervals (CIs) were computed for means and percentages. Estimates with relative standard errors greater than 30% were noted as unreliable.
Generalized linear-contrast t tests were used to compare subgroups and to compare risk factors between adults with depression and those with neither depression nor anxiety and to compare adults with anxiety and those with neither disorder.
Logistic regression with manual stepwise backward elimination was performed to determine factors associated with diagnosis and treatment. Predicted marginal prevalence estimates (adjusted for other covariates) from the logistic models were used to calculate prevalence ratios and their CIs.
Results
Prevalence of current depression and anxiety
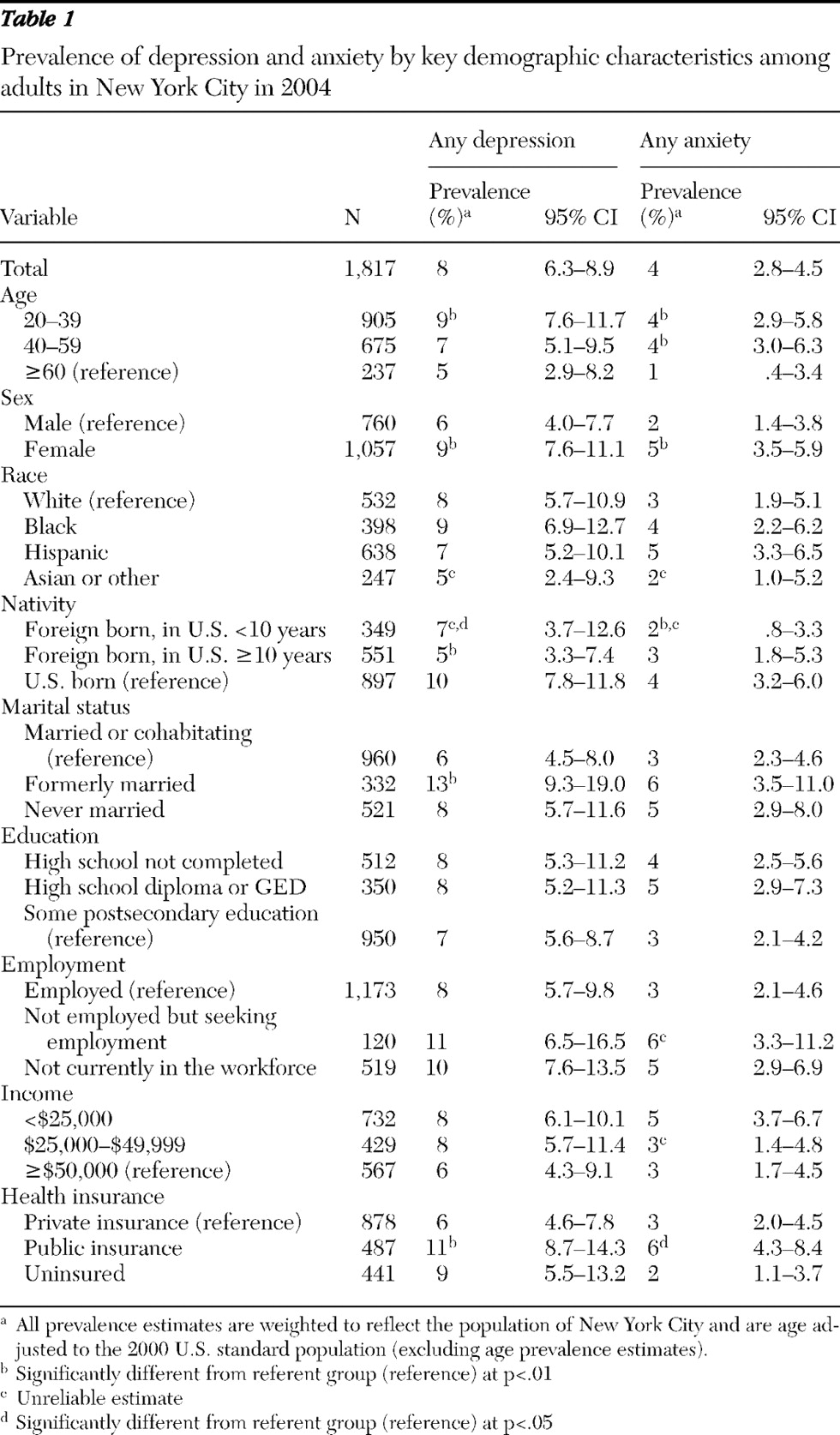
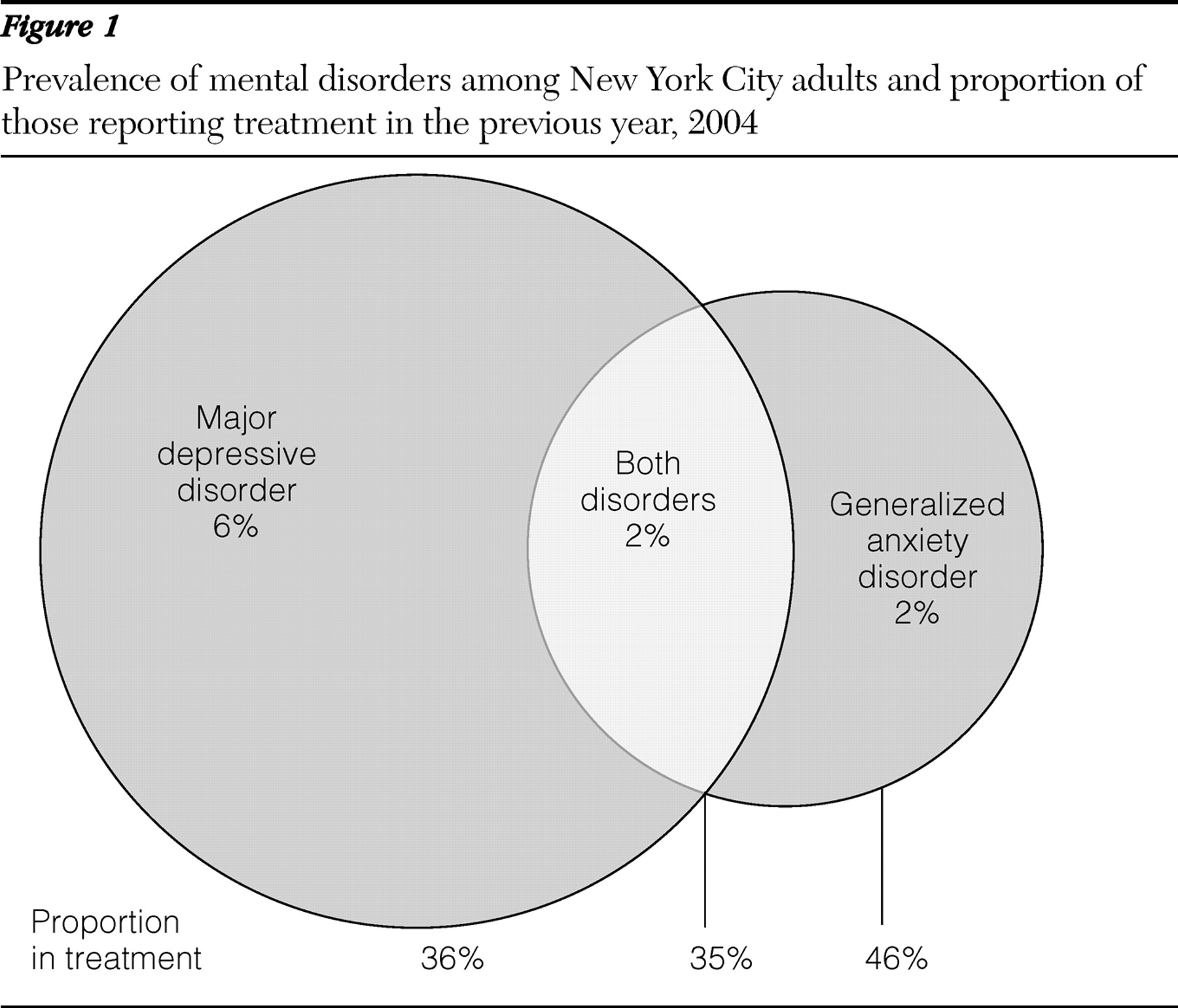
Survey responses indicated that the prevalence of major depression in New York City was 8% (approximately 440,000 people). Four percent (approximately 210,000 people) had a current diagnosis of generalized anxiety disorder (
Table 1 ). Ten percent of the population had either condition (CI=8.1–11.0). In regard to co-occurrence, one in five (21%) adults with depression also had anxiety, and nearly half (48%) of adults with anxiety also had depression. The prevalence of comorbid depression and anxiety was 2% (CI=1.1–2.3).
The rate of depression was highest among persons who were formerly married (13%), those seeking employment (11%), those not in the workforce (10%), and those with public health insurance (11%). Prevalence of depression was low among men (6%), foreign-born persons in the United States ten years or more (5%), and persons 60 years of age or older (5%).
Prevalence of anxiety was highest among persons who were formerly married (6%), those with public health insurance (6%), and the unemployed (6%). Anxiety was significantly less prevalent among adults ages 60 and older than among younger adults (1% versus 4%; p<.001) and slightly less prevalent among foreign-born adults than among U.S.-born adults, although numbers were small and this difference was not statistically significant. Among foreign-born respondents, the prevalence of anxiety tended to increase with length of time in the United States, from 2% among those living in this country for less than ten years to 3% among those who were in the country for ten years or more, although this difference did not reach statistical significance. Compared with U.S.-born adults, only persons in the United States for less than ten years had significantly lower rates of anxiety (2% versus 4%; p<.01).
Health and functional effects of depression and anxiety
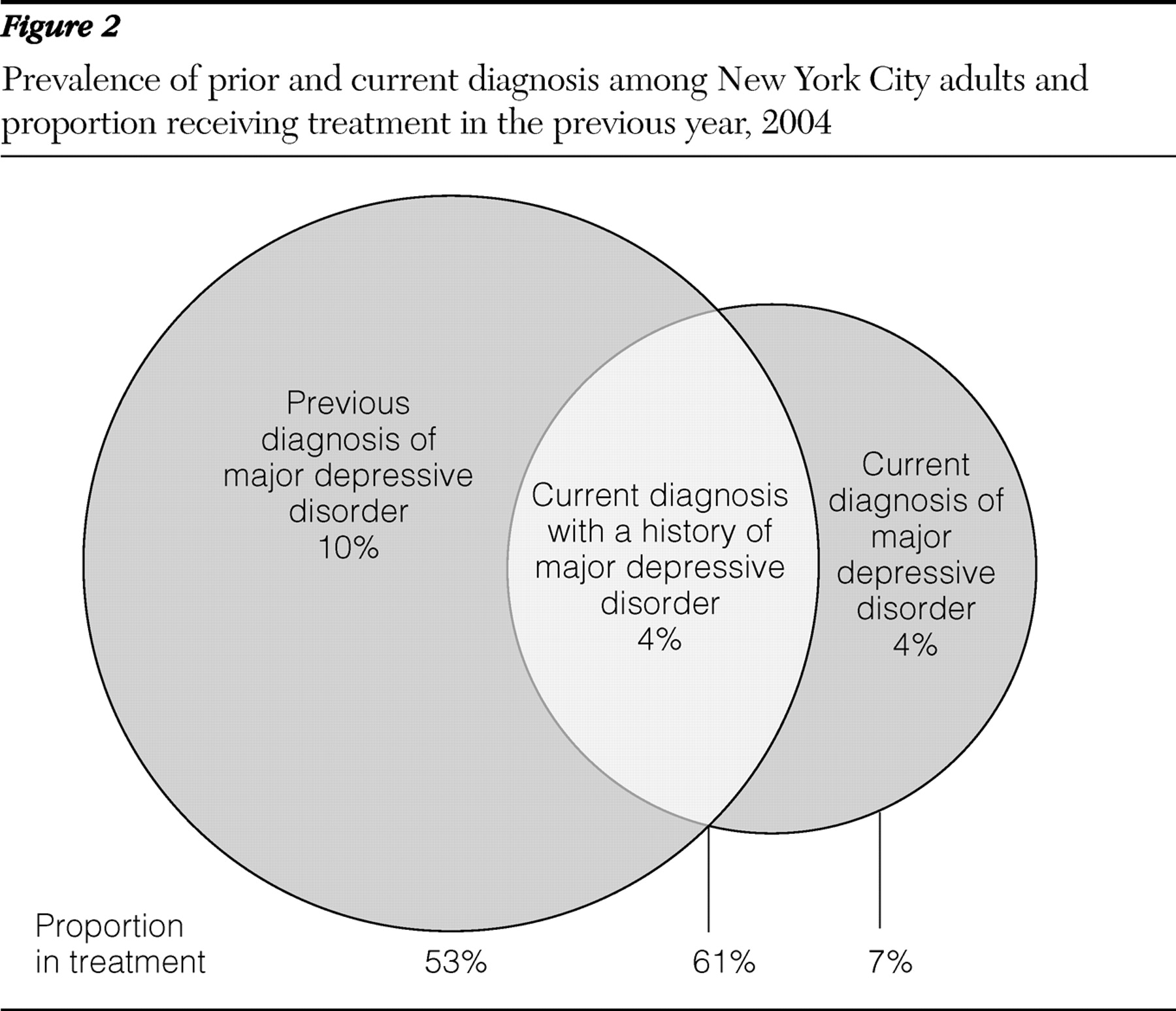
Smoking was twice as prevalent among adults with either depression or anxiety compared with adults with neither diagnosis (
Table 2 ). Alcohol use was significantly higher among persons with depression than among those with neither diagnosis (63% versus 57%; p=.005) and among those with both anxiety and depression than among respondents with anxiety only (79% versus 45%; p=.001).
Respondents with anxiety demonstrated the highest levels of functional impairment. Nearly one in four (23%) adults with anxiety reported that mental health problems limited their ability to work—17 times that of adults with neither diagnosis (p<.001). They also were more likely than respondents with neither diagnosis to report asthma (24% versus 11%; p<.01) and ulcers (21% versus 7%; p<.05). Adults with depression also experienced work limitations. Those with either diagnosis were approximately twice as likely as other adults to have diabetes and report needing more emotional support. Persons with depression were almost twice as likely as those with neither depression nor anxiety to have had 50 or more sex partners in their lifetime (13% versus 7%, comparison not statistically significant), and persons with anxiety or depression were similarly likely to perceive themselves to be at moderate or high risk of having a sexually transmitted infection (6% versus 4%, comparison not statistically significant).
Diagnosis and treatment
Slightly more than half (55%) of respondents with depression had ever been told that they had depression. About a third (38%) of adults with either depression or anxiety reported that they were currently receiving treatment.
Figure 1 displays the relationships between depression, anxiety, and treatment. Recent treatment was reported by 36% of respondents with depression alone, 46% of respondents with anxiety alone, and 35% among those with both diagnoses.
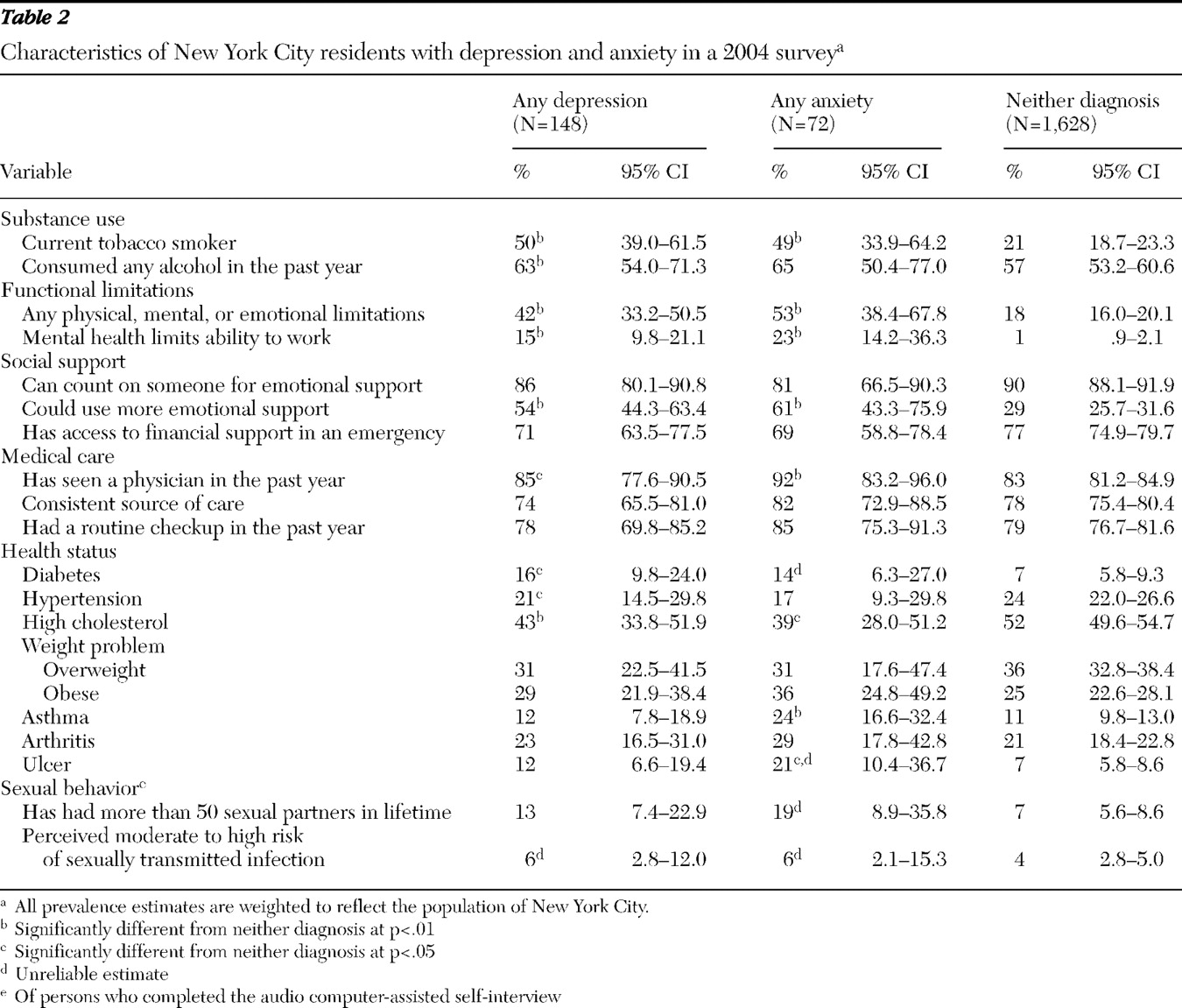
Previously diagnosed depression, current depression, and the proportion of each of the groups receiving treatment are shown in
Figure 2 . Of adults who had been diagnosed as having depression at some point in their life, 71% did not meet CIDI criteria for a current diagnosis of major depression. Half (53%) of these respondents had received recent mental health treatment, which suggests that a current disorder may be adequately treated and thus not measurable in this study. Among adults with current depression, those with a previous diagnosis were more than nine times as likely to have had treatment in the past year than those with no previous diagnosis (61% versus 7%; p<.001).
A combination of medication and counseling was reported by 23% of respondents with current depression, 28% of those with current anxiety and 23% of those with either disorder. Among persons with depression, 8% received counseling only and 5% reported medication only. Of the persons with diagnosed depression, 44% were currently taking antidepressants; of those taking antidepressants, 67% were taking selective serotonin reuptake inhibitors. Among respondents with anxiety, use of counseling only (6%) and use of medication only (5%) were similarly infrequent.
When education and nativity were included in a multivariable model, both predicted undiagnosed depression. Adults who had at least a high school diploma or GED were more likely to have undiagnosed depression than those who had not (adjusted prevalence ratio [aPR]=1.7, CI=1.0–2.7). Foreign-born adults were 60% more likely than U.S.-born adults to have undiagnosed depression (aPR= 1.6, CI=1.2–2.2). The absolute proportion of undiagnosed depression among the foreign born was 64% compared with 39% among the U.S. born.
Factors associated with treatment among respondents with depression in a multivariable model were a previous diagnosis of depression (aPR=2.9, CI=1.5–5.7), reporting that mental health problems limited one's ability to work (aPR=2.5, CI=1.8–3.6), and being born in the United States (aPR=1.7, CI=1.1–2.7). Among those with anxiety, predictors of recent mental health treatment included having a regular source of medical care (aPR=3.4, CI=1.3–9.4) and reporting that mental health problems limited one's ability to work (aPR= 2.4, CI=1.5–3.9).
Discussion
Major depression and generalized anxiety disorder were relatively common in New York City (8% and 4% of the adult population, respectively), yet they were often undiagnosed (45% of those with depression) and usually untreated (62% among those with either depression or anxiety). Although underdiagnosis and undertreatment affected all demographic groups, persons born outside the United States were especially at risk of having undiagnosed and untreated depression, and those with at least a high school education were more likely to have undiagnosed depression. In addition, depression and anxiety caused significant disability among New York adults (15% and 23% among those with depression and anxiety, respectively).
Our findings suggest that mental disorders in New York City are slightly more common than recent national estimates, which indicate that 3.1% of U.S. adults have anxiety and 6.7% have depression (
19 ). Differences may be due to the local demographic profile. Although New York City has larger foreign-born (35.9% versus 11.1%), black (26.6% versus 12.3%), and Hispanic (27.0% versus 12.5%) populations than the rest of the U.S. and persons in racial and ethnic minority groups have demonstrated lower rates of depression than whites in national studies (
19 ), poverty also has a strong correlation with depression, and New York City has a higher proportion of people living in poverty than the country as a whole. The 2004 poverty rate was 20.3% in New York City versus 13.1% in the United States (
20 ).
Consistent with findings from other studies, we found a significantly lower prevalence of depression among foreign-born adults (
21,
22,
23 ). Although some studies have shown that certain immigrant groups, primarily refugees from countries experiencing armed or political conflict, have a higher prevalence of mental disorders, those choosing to immigrate to the United States under less severe conditions may be more psychologically resilient (
23,
24 ). Some studies suggest that immigrants experience increased rates of psychiatric disorders with increasing length of U.S. residency (
8,
9 ). Our finding that anxiety slightly increased with duration of residency is consistent with these findings.
We found that foreign-born persons were less likely to have been diagnosed or treated for depression than persons born in the United States. This finding likely reflects the fact that foreign-born New Yorkers have less access to health care in general (
25 ). Further, cultural misconceptions about mental disorders and stigma (especially among those with limited acculturation) may create additional barriers to obtaining appropriate mental health services. Given that the number of immigrants living in U.S. households has increased 16% in the past five years and that the total immigrant population increased 57% between 1990 and 2000, detection and care of mental health conditions will be a public health priority for U.S. areas with large or growing immigrant communities (
26,
27 ).
Unlike national studies, our study did not find significantly lower rates of depressive disorders among black and Hispanic persons than among whites (
3,
19 ). The fact that depression among Hispanics was not higher than the rate among whites is surprising, because local telephone surveys showed much higher rates of nonspecific psychological distress among Hispanics than among whites (
6 ). Elevated rates of nonspecific psychological distress among Hispanics could reflect differences in the prevalence of dysthymia and other less severe depressive conditions rather than major depression. Riolo and colleagues (
28 ) similarly found lower rates of depression and higher rates of dysthymia among black and Hispanic groups than among whites. Nonspecific psychological distress among Hispanics may also reflect disorders other than depression, such as anxiety. Although our sample was too small to show statistically significant differences in the prevalence of anxiety across racial-ethnic groups, we found that the prevalence of anxiety among Hispanics was 52% higher than among whites. This finding is consistent with other epidemiologic findings (
29 ).
Lower socioeconomic status has consistently been linked with depression (
3,
30 ). Although lower family income and education were not associated with increased depression, we found that persons with public health insurance had more depression than those with private insurance. Type of insurance may be a better proxy for socioeconomic status than classifications based on family income, because eligibility for public insurance is based on income as well as the number of children living in a household. When we evaluated the impact of socioeconomic characteristics on treatment for depression, we saw no significant association with any of these socioeconomic variables. This is contrary to findings observed nationally and may result from New York City's extensive public health care network, which makes low-cost health care available to all New Yorkers, regardless of ability to pay (
31 ).
Depression and anxiety were often disabling; 15% of persons with depression and 23% with anxiety reported that their conditions affected their ability to be productive at work. Although anxiety was less than half as common as depression, nearly as many people reported workplace disability from it. Overall, more than 1% of the population reported workplace disability from one or the other condition. The high rate of medical conditions and unhealthy behaviors among those with mental health conditions indicated that depression and anxiety impose significant economic and social costs. Given that most adults with depression or anxiety are inadequately treated and that significant clinical improvement has been shown for approximately 70% to 80% of appropriately treated patients (
32 ), an important opportunity exists to reduce the burden of these disabling conditions through expanding treatment.
A major risk for not being treated was not being diagnosed. Increased detection is necessary to reduce the burden of mental disorders and is particularly important for at-risk groups, including women, the formerly married, those who are publicly insured, and immigrants. Evidence suggests that primary care physicians and other nonpsychiatrists can effectively screen for and manage most cases of depression. The New York City Department of Health and Mental Hygiene, for example, has undertaken an initiative to widely disseminate a standard self-administered scale to allow providers to screen for depression and monitor the effectiveness of treatment (
33 ).
There are limitations to the interpretation of these data. The response rate of 55% might have resulted in selection bias, although it is not clear whether persons with mental health problems would be more likely or less likely to participate. We attempted to address selection bias by adjusting survey weights for factors influencing nonresponse, such as age, borough, and group-level characteristics from the U.S. Census such as percentage black, average household size, and median household income. Another limitation was the exclusion of institutionalized and homeless persons, likely resulting in an underestimation of the true burden of depression and anxiety. Also,
DSM criteria, as operationalized by the CIDI, might incorrectly capture persons with reactive depression, a reversible phenomenon caused by environmental stressors that is not fueled primarily by the biological processes that manifest in major depression (
34 ). The data are also subject to recall bias and measurement error; however, standardized quality assurance procedures from the national survey protocols were used to reduce these potential sources of error. In addition the CIDI was not consistently translated into languages other than Spanish, and estimates may not represent persons from more linguistically isolated populations. Finally, small samples of certain subgroups limited more detailed analyses.