This review examines prisoner suicides that occurred in the California Department of Corrections and Rehabilitation (CDCR) from 1999 to 2004. The review was conducted pursuant to Coleman v. Schwarzenegger, a federal district court case decided in late 1995 in which the plaintiffs, a certified class of state prison inmates, successfully challenged the adequacy of mental health services available to them. The litigation culminated in the appointment of a special master and a deputy master to oversee the development and implementation of a constitutionally sound mental health services program in CDCR. These persons were appointed by the court to remedy constitutionally inadequate mental health care and to promote other constitutional requirements in the program.
CDCR's mental health services delivery system is intended to provide reasonable access to screening, assessment, and treatment for prisoners with serious mental illness. The mental health services delivery system comprises several levels of care, including the correctional clinical case management system (that is, an outpatient program for prisoners within the prison setting), the enhanced outpatient program (which consists of specialized housing units with enhanced mental health treatments), mental health crisis bed units with 24-hour nursing care (that is, an infirmary setting) for suicidal prisoners or prisoners in crisis, and acute and intermediate inpatient care in programs operated by the California Department of Mental Health located within two CDCR facilities and within hospitals run by the California Department of Mental Health that are outside CDCR.
This review is not intended to provide a comprehensive analysis of the mental health services and programs provided by CDCR. Rather, it focuses solely on the suicides that occurred in CDCR during the covered six-year span; on the recorded events before, during, and after each suicide that help facilitate an analysis of the potential suicide risk; and on the clinical and custodial factors relevant to each completed suicide.
Results
The third leading cause of death in U.S. prisons is suicide, exceeded by natural deaths and deaths from AIDS (
3 ). At least six well-known demographic characteristics of persons who commit suicide are shared by the U.S. general population and the incarcerated subpopulation, including age, gender, ethnicity, drug and alcohol abuse, history of psychiatric treatment, and prior suicide attempts (
4,
5 ). For the community, more than 90% of people who die by suicide have a combination of those risk factors, such as male gender and increasing age (
4,
5 ). For the incarcerated population these risk factors are similar with the exception of the highest rates of suicide being in the 31 to 40 age range because of fewer numbers of inmates aged 41 and older. The rates for inmates older than 50 are 9%, similar to the 14% rate in the community (
4 ). In prisons, such as the CDCR, younger inmates comprise the majority of inmates, with declines in numbers over time. The percentage of suicide reflects these declining numbers by age but is consistent with prevalence in the community (
4,
5 ). From 2000 to 2002 state prisoner suicide rates ranged from 13 to 14 suicides per 100,000 prisoners for every age group over 18 (
6 ). Men are four times more likely than women to commit suicide (
7 ). Non-Hispanic Caucasian males are the highest-risk group (
7 ). The rate of suicide is highest among non-Hispanic Caucasian men, regardless of whether they are inside or outside of correctional facilities (
5,
7 ). Family conflict, bereavement, and loss of support are well-known risk factors. First incarceration, which usually takes place in a jail, is a widely known risk factor, as described by Metzner and Hayes (
5,
8 ) and others (
6,
9,
10,
11 ).
In contrast to society at large, where ready access to a handgun is identified as a risk factor and handguns are the most common method of suicide, hanging was the most frequently employed method of suicide in custody found in this and other studies. This was not surprising in view of the crucial role played by a readily accessible method. In the sample presented here, hanging was employed in 85% of cases. This finding was consistent with the literature on incarcerated populations (
5,
6,
8 ) and with the Missouri samples of completed suicides in prisons (N=37) described by Daniel and Fleming (
11 ), who found that hanging was the most frequent method of suicide, employed in 81% of cases.
Although the suicide rate in jails dropped more than 50% between 1983 and 2002 in the United States, from 129 per 100,000 down to 47 per 100,000, as described by Mumola (
6 ), jails continue to have a much higher rate of suicide than prisons. Suicide rates in state prisons also dropped, from 34 per 100,000 in 1980 to 16 per 100,000 in 1990, with further decline to 14 per 100,000 by 2004 (
5,
6,
7,
9 ).
Recently there have been indications that suicide rates among Hispanics and suicide attempts among young African-American men are rising nationwide (
6 ). Regarding the incarcerated population, non-Hispanic Caucasian inmates commit suicide at the highest rate (96 per 100,000), compared with rates of 30 per 100,000 among Hispanics in custody and rates of 16 per 100,000 among African Americans in custody (
6 ). In the sample presented here, the number of Hispanic men who committed suicide approached that of non-Hispanic Caucasians, while the number of African Americans who committed suicide remained low.
The body of literature on suicide risk factors suggests hypotheses—some already codified in standards promulgated by the American Correctional Association and the National Commission on Correctional Health Care (
1,
12 )—that should elicit keen interest among those charged with the care of incarcerated individuals.
The accompanying tables provide graphic representation of the demographic data collected during each of the six years covered in the study.
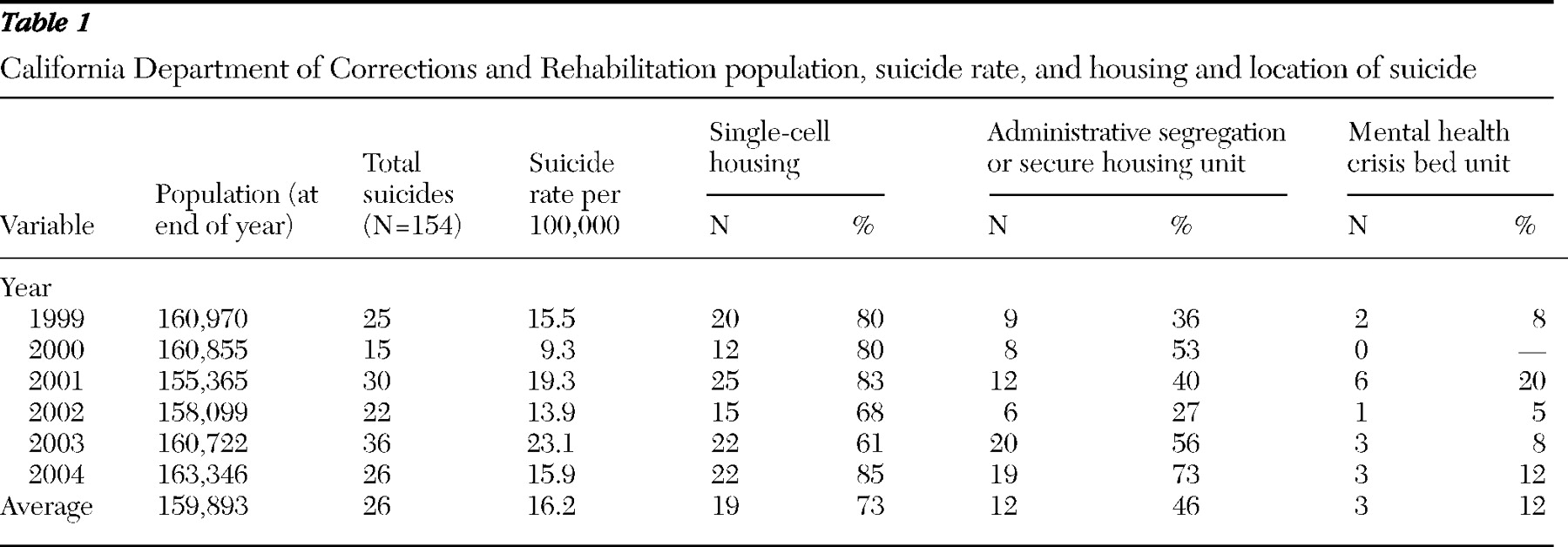
The number of annual suicides occurring during the covered period ranged from a low of 15 in 2000 to a high of 36 in 2003. On the basis of the institutional population of CDCR at the end of each of these respective years, the suicide rate ranged from 9.3 per 100,000 to 23.1 per 100,000. The variability in the annual rate of suicides is tracked for each of the covered years in
Table 1 .
The wide range of variability illustrates the pitfalls of comparing annual rates of an event with a low base rate event in a small, fluctuating population. Even with large samples, a minimum of five years of data are needed for meaningful analysis because of year-to-year variability and other factors affecting mental health resources (
10,
11,
13 ).
Table 1 also provides a breakdown of the annual end-of-year overall CDCR population and the annual number of suicides per year in each type of housing unit where prisoners resided at the time of their deaths. Three different types of housing units were examined: single cell, administrative segregation or secure housing, or mental health crisis bed. Single-cell units are defined as one inmate per cell and can be for the general population or for inmates with specialized needs. Administrative segregation and secure housing units can have one or two persons in a cell. Administrative segregation consists of housing units where inmates are generally locked in their cells 23 hours per day, for days to months at a time, and secure housing units are a "super maximum" security setting where inmates are typically locked in their cells for 23 hours per day for one to many years. Mental health crisis bed units or outpatient housing units have one person in a cell and have nursing and clinical staff on the units 24 hours per day. The breakdown of suicides occurring in single-cell housing in administrative segregation or secure housing units and in the general population (that is, nonspecialized housing units) is also included in
Table 1 . The data indicate that 73% of all suicides were completed in single cells, while 46% of completed suicides occurred in single cells in administrative segregation or secure housing units and 12% occurred in mental health crisis beds.
These findings regarding the importance of environmental stressors unique to prison conditions, such as isolation, punitive sanctions, severely restricted living conditions, and acquisition of new charges or imposition of an unexpected sentence were consistent with previous reports (
11,
14,
15 ). We found that the conditions of deprivation in locked units and higher-security housing were a common stressor shared by many of the prisoners who committed suicide. Liebling (
16 ) found that recent punishment, segregation, long or unexpected sentences, and high levels of reported distress, including symptoms of depression and anxiety, were reported by a sample of men who attempted suicide. In Liebling's (
16 ) sample of 50 cases, 24% had recently experienced punishment or were in segregation and 22% had recently received a long or an unexpected sentence.
Among the 154 prisoners who committed suicide during the six-year period, 149 (97%) were male, and four (3%) were female. Sixty-two (40%) were Caucasian, 55 (36%) were Hispanic, 25 (16%) were African American, four (3%) were Asian, and eight (5%) were of another race or ethnicity. Seventy-three (47%) of the prisoners who completed suicide were aged 31–40 years, 42 (27%) were 18–30 years, 24 (16%) were 41–50 years, 14 (9%) were older than 50 years, and one (1%) was younger than 18 years.
The methods utilized by prisoners who completed suicide included hanging (N=131, or 85%), lacerations or exsanguinations (N=9, or 6%), overdose (N=5, or 3%), and other (N=9, or 6%).
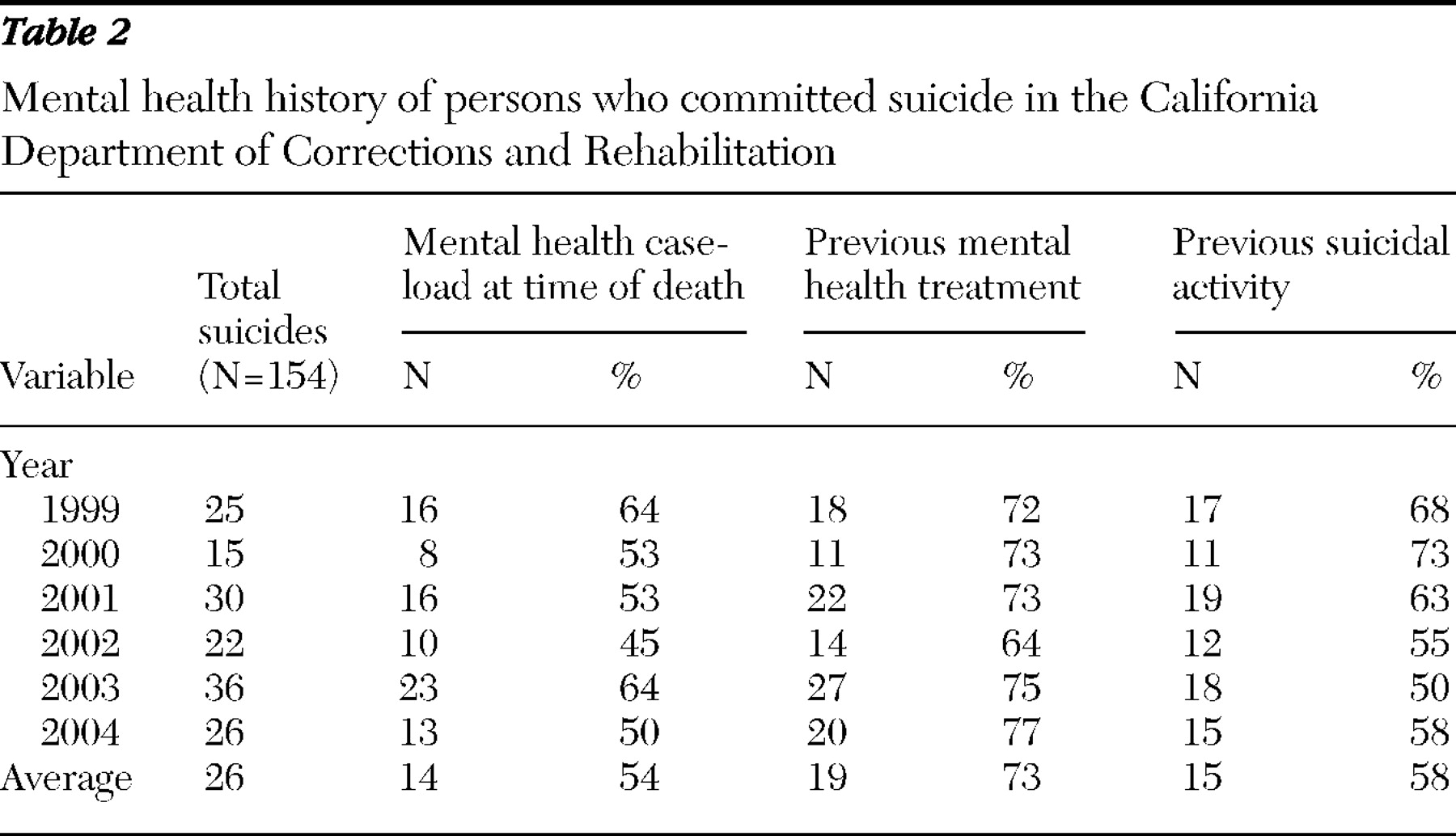
Among prisoners who completed suicide during the six-year period, 73% had a history of mental health treatment, and 62% had a history of suicidal behavior or statements. The breakdown of these numbers for each year is provided in
Table 2 .
Among the 154 suicides completed during the covered period, 87 (56%) involved prisoners on the mental health caseload.
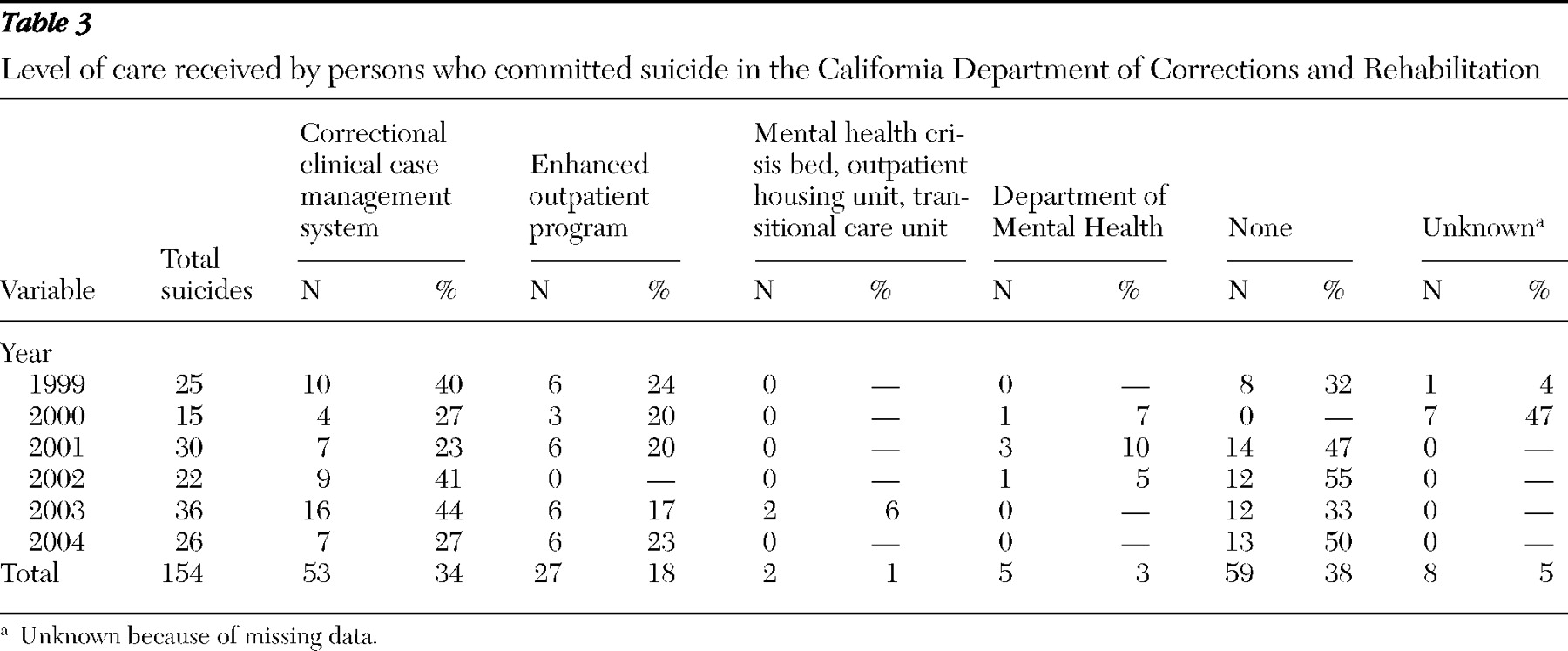
Table 3 provides the breakdown. One caveat: prisoners housed in a mental health crisis bed unit or a Department of Mental Health inpatient program may have been at any level of care before their placement in those beds, including "none." The level of mental health care for the 87 prisoners included in the CDCR mental health caseload at the time of their suicides was as follows: five (3%) were at the Department of Mental Health inpatient (hospital) level of care; two (1%) were at a crisis level of CDCR care (in a mental health crisis bed unit, outpatient housing unit, or transitional care unit); 27 (18%) were in the enhanced outpatient program; and 53 (34%) were in the correctional clinical case management system program.
These findings are consistent with Daniel and Fleming's ten-year review (
11 ) of prison suicides in Missouri. These findings point to the need for thorough suicide risk assessment of prisoners who appear to be relatively high functioning or who are found not to be in need of ongoing mental health treatment. In the group of suicides presented here, 59 (38%) were not in need of mental health treatment (as determined by the CDCR clinical treatment staff), a percentage that was higher than Daniel and Fleming's finding that nearly 30% of the prisoners who committed suicide over a ten-year period in Missouri presented with no mental health problems (
11 ). For eight (5%) inmates, mental health treatment status was unknown because of missing data. In our California sample, like the Missouri sample, the prevalence of prior treatment was higher than current need for treatment. Both findings reflect a well-known indicator of elevated suicide risk in society at large—that is, history of psychiatric treatment. A total of 112 of 154 (73%) of the persons who committed suicide in our sample had a history of psychiatric treatment; however, 101 of the 112 (90%) had axis I diagnoses. Seventy-three percent of the total Missouri sample had been diagnosed as having an axis I disorder at some point in the past, and 66% of our total sample had a diagnosis of an axis I disorder at some point in the past (
11 ).
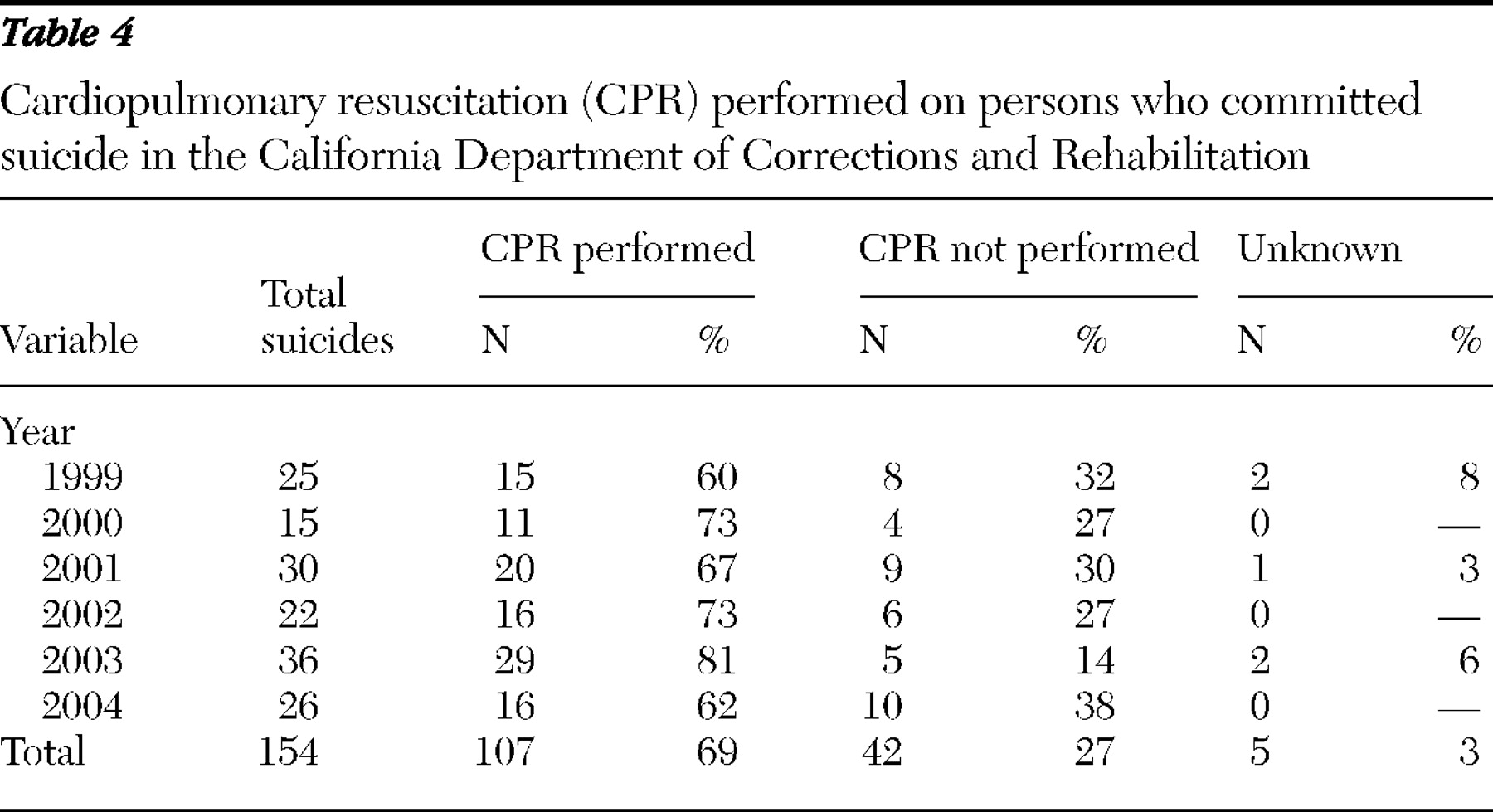
Also reviewed were emergency responses to inmates who were unresponsive when they were discovered and who subsequently were determined to have committed suicide. The reviews focused on the timely initiation and continuation of cardiopulmonary resuscitation (CPR) by first responders. Policy requires that CPR be initiated and continued with very few exceptions, exceptions such as the presence of rigor mortis, lividity, or obvious trauma, such as severe head injury or decapitation. For the six-year review period, CPR was performed in a timely and appropriate manner on 107 inmates who committed suicide (69%), CPR was not performed in a timely and appropriate manner on 42 inmates (27%), and it could not be determined on the basis of the available documentation whether CPR was performed in a timely or appropriate manner on five inmates (3%). These results are presented by year in
Table 4 .
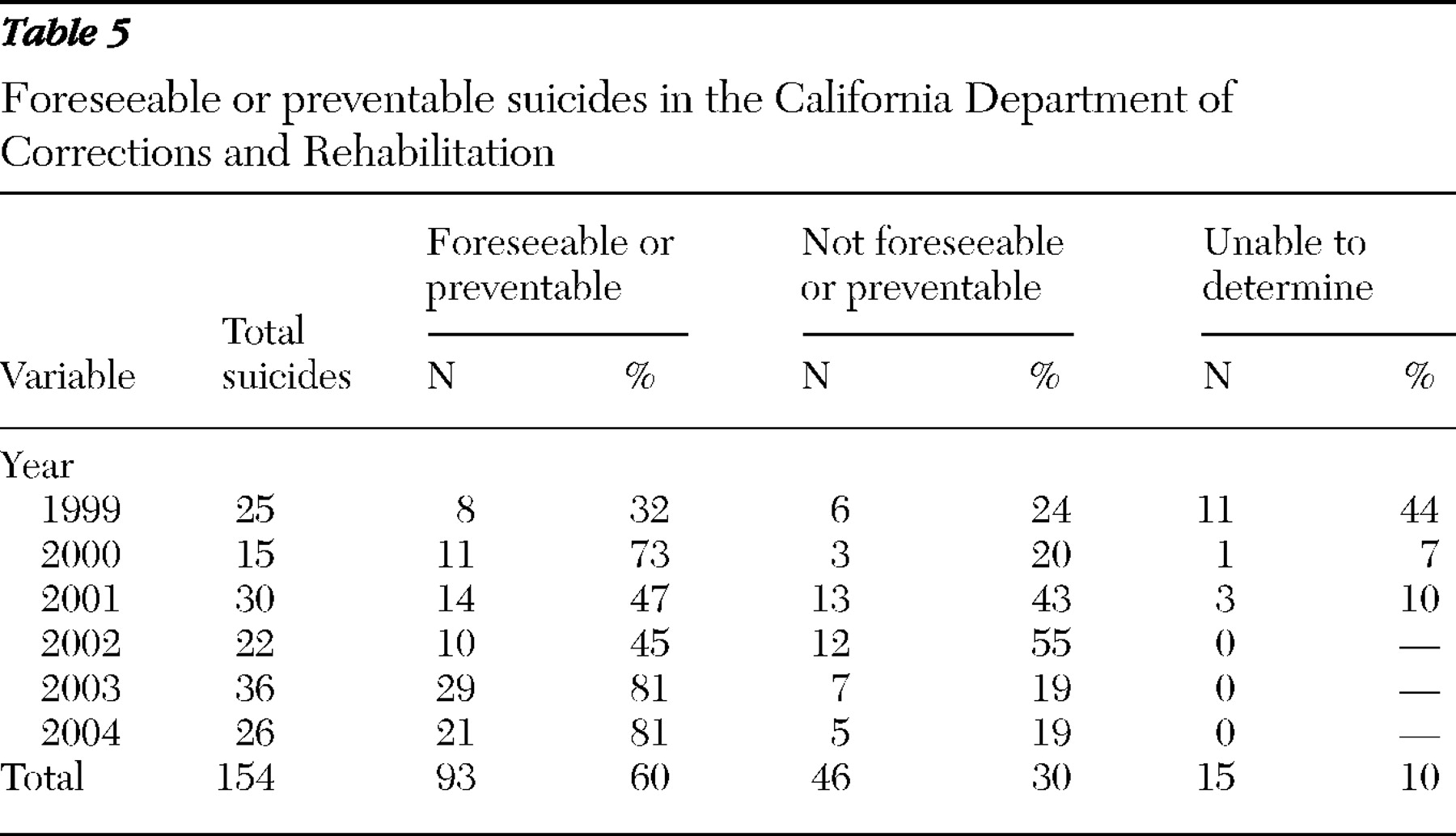
Sixty percent of all the suicides covered in this six-year period were either foreseeable or preventable, and some were both. The term "foreseeable" refers to cases in which already known and reasonably available information about an inmate indicates the presence of a substantial or high risk of suicide that requires responsive clinical, custody, or administrative interventions to prevent self-harm. The term foreseeable is not to imply "predictable," because suicide is not predictable, but rather to refer to the presence of an elevated risk to substantial or high risk, which requires appropriate clinical or custodial intervention or monitoring.
The term "preventable" applies to situations where if some additional information had been gathered or some additional interventions had been undertaken, usually as required in existing policies and procedures, the likelihood of a completed suicide might have been substantially reduced. The concept includes, but is not limited to, situations where inmates report self-injurious behaviors or threats but do not receive appropriate evaluation or treatment, are not transferred to a more clinically appropriate or safe environment, or fail to receive appropriate lifesaving procedures, such as timely CPR.
Table 5 shows the breakdown of foreseeable and preventable suicides by year. Major contributing factors in foreseeable or preventable deaths included inadequate clinical assessments, inappropriate interventions, incomplete referrals, missed appointments and appointments that were not rescheduled, unsupported diagnoses, failure to review records, assignments to inappropriate levels of mental health care, failure to provide protective housing, and the provision of inadequate or untimely resuscitation efforts. In numerous cases, multiple such factors contributed to the outcome.
Discussion
During the period covered by this review, both the scope and quality of CDCR's review process improved significantly. In 1999 psychological autopsies were rarely included in reviews, and many of the psychological autopsies were conducted by personnel who were clinically involved directly or indirectly with the specific inmate who committed suicide. By 2004 clinicians not involved in specific inmates' care and treatment had performed psychological autopsies for all inmates who had committed suicide. In 1999 the special master's reports recommended improvements in the review process that included clarification of the duties of local reviewers, mandated time frames for completion of reviews, and the development of corrective action plans. Subsequent procedural recommendations focused on specific timelines for the preparation of responsive corrective action plans by institutions.
The review process did not focus solely on procedural elements. From the beginning of the study period the annual review helped prompt substantive changes and improvements in suicide prevention policy and practices, including, for example, requirements for increased clinical monitoring of prisoners in high-security units, both for those who were and for those who were not on the mental health caseload; the development of clinical and custody follow-up monitoring regimens for suicidal prisoners discharged from mental health crisis beds and their alternatives; the effective provision of group therapy for prisoners on the mental health caseload in administrative segregation units; the development of routinely administered suicide risk assessments; efforts to keep suicidal prisoners out of cells with heating, ventilating, and air conditioning vents with large-mesh screens to facilitate hanging; a ban on the substitution of video monitoring for the personal observation of prisoners on suicide watch; and the development and implementation of improved CPR policies and practices.
The suicides by four female inmates and the sharp rise in the number of suicides in locked units, particularly administrative segregation, led to greater attention to both areas. Failure to use a suicide risk assessment instrument as required by departmental policy was a factor in the female suicides, and corrective measures were taken. The rising rate of suicide in administrative segregation initiated a two-year effort to analyze the causes and prescribe remedies. The latter have included, among other initiatives, custody monitoring of new arrivals at 30-minute intervals, preplacement mental health screenings, better tracking of history of suicidal behavior, easing of property restrictions for protective custody prisoners, and improved physical safety in cells for newly arrived prisoners. Several of these remedies were based upon data indicating that suicides occurred most often within three weeks of a prisoner's placement in an administrative segregation unit. In the California cases, 39 of 74 (53%) of the suicides that occurred in administrative segregation or secure housing units occurred within three weeks of placement. Individuals housed in administrative segregation and secure housing units are more isolated than those in the general prison population, and these housing changes may represent a very different and stressful environment for inmates as they are placed in these environments because they incurred charges or for safety and protective custody reasons (typically these environments involve 23 hours per day in cell confinement with some exceptions for out-of-cell time for yard activities and showers).
Conclusions
Over the six years of the study, the suicide review process has identified characteristics that ought to draw the attention of staff to certain categories of prisoners, including the following:
• Prisoners with a history of serious mental illness
• Prisoners with a history of suicide attempts
• Prisoners housed in a single cell, particularly in administrative segregation or a secure housing unit
• Prisoners expressing safety concerns with associated anxiety and agitation
• Prisoners with serious medical concerns
• Prisoners with both severe personality disorders and coexisting mental illness
• Prisoners whose legal status has undergone significant change—for example, individuals returning from court after denial of appeals and those receiving third-strike determinations or other additions to their sentences
• Caucasian prisoners, although the number of suicides among Hispanic prisoners increased rapidly during the six-year period.
The above categories may help identify prisoners who might warrant focused attention. CDCR's experience with completed suicides over the study period highlights both clinical practices and physical conditions that ought to be addressed, including the following:
• The failure of clinical staff to refer potentially suicidal prisoners to programs with more intensive monitoring and care
• The provision of prompt and adequate access to higher levels of monitoring and care to prisoners identified as potentially suicidal
• The elimination of physical safety deficiencies in cells and other housing for prisoners most at risk of suicide—for example, large mesh vents or other protuberances regularly used for hanging
• The lack of adequate confidential interviewing space in most high-custody housing units, which inhibits the ability and willingness of potentially suicidal prisoners to communicate effectively with clinicians about their risk of suicide
• Clinicians' failure to review fully and carefully available documentation, such as health and classification records, for indices of prior suicidal activity or ideation
• The timely completion of all of the documentation associated with the institutional or departmental elements of the suicide review process, including the documentation of implemented remedies and adverse personnel actions.
This review suggests the following recommendations and considerations for correctional administrative, clinical, and custody staff members to assist in their efforts to establish and manage an effective suicide prevention program:
• The development and timely implementation of effective policies and procedures
• Training and supervision of all staff regarding adherence to policies and procedures
• Development and implementation of a systematic quality management process with review of all completed suicides
• Use of screening criteria, clinical rounds, and timely access to care for inmates in isolated conditions of confinement, especially administrative segregation
• Access and timely transfers to higher levels of care when indicated
• Provision of a timely and complete emergency response system, including CPR, first aid, and transfer to medical units or facilities
• Consideration of the impact of overcrowding and staffing deficiencies.
Prisons and prison life create enormous stress, even for individuals who are mentally healthy. The strain for offenders with mental illness, who are often both fragile and intensely vulnerable, sometimes exceeds their ability to cope. One surpassingly critical purpose of mental health services in prisons is to help identify such individuals for intervention and provide the monitoring, treatment, and physical safety needed for their survival. This review attempts to provide some clues about recognizing prisoners most at risk of suicide and to identify some of the failed practices and inadequate conditions that often combine to prevent the provision of adequate protection and treatment. This review identifies several risk factors, as well as necessary administrative, clinical, and custody staff involvements and responsibilities for an effective suicide prevention program.