Clinical work with diverse populations requires assessment and treatment planning that are sensitive to ethnocultural background and social context (
1,
2,
3 ). To assist clinicians in identifying clinically relevant aspects of patients' cultural background,
DSM-IV introduced an outline for cultural formulation (
4,
5 ). The cultural formulation has not been widely incorporated into standard clinical practice; however, and despite a report that identified the refinement of cultural formulation as a high priority in preparation for
DSM-V (
6 ), there are no published evaluations of its utility. This study assessed the usefulness of the
DSM-IV Outline for Cultural Formulation from the perspective of consultants working for a Cultural Consultation Service (CCS) in an outpatient psychiatry department of a general hospital in Montreal, Canada (
7 ).
Methods
The CCS is based in an urban area where 45% of the population comprises immigrants and refugees (
8 ). The service receives requests for assistance from primary care providers and mental health professionals throughout the region who are facing difficulties with the assessment or treatment of ethnically diverse patients. The CCS has a clinical coordinator and a network of interpreters; cultural consultants, who are clinicians; and culture brokers, who are nonclinicians with specific cultural knowledge and who assist a CCS clinician in conducting the assessment.
The CCS developed and uses an expanded version of the
DSM-IV-TR (
9 ) Outline for Cultural Formulation, which has specific questions on migration history, citizenship status, multiple cultural backgrounds and identities, and extended family network (the expanded version is available at www.mcgill.ca/ccs). Additional areas explored in this expanded version of the cultural formulation include details on migration trajectory (origins, reasons for migration, route, time in refugee camp or other intermediate locations, and exposure to violence; situation of family members left behind, plans for reunification, and current status of family members in receiving country); ethnocultural identities, affiliations, and practices of the patient and family members; cultural illness models represented as "procedural knowledge" or prototypes in addition to explicit explanatory models (
10 ); psychosocial stressors and supports related to extended family and local and transnational family, the community, and political conflicts; impact of racism and discrimination; and mutual perceptions of power and position of patient and clinician, including the history of relationships between their respective cultural background groups (
11 ).
After initial screening and intake over the telephone by the clinical coordinator, a consultant (with the aid of an interpreter or culture broker, as needed) assesses the patient in one to several interviews. After the interviews, the consultant or the culture broker writes a cultural formulation report. The formulation and recommendations are discussed at a clinical case conference and sent to the referring clinician. Of the 66 consultants and culture brokers who worked with the CCS in a five-year period, 60 used the cultural formulation and were interviewed for this study, generally within three months of starting work for CCS. Surveys were given between 2002 and 2006.
Two 5-point Likert items inquired about familiarity with the DSM-IV Outline for Cultural Formulation before working with the CCS and perceived usefulness of the cultural formulation (scores range from 0, not at all, to 4, extremely). Closed questions asked about use of the cultural formulation to organize clinical data or to write up the case, and open-ended questions asked about useful or not useful aspects of the cultural formulation and suggestions for its refinement. Mann-Whitney U and chi square tests were used for comparisons on Likert and dichotomous variables, respectively.
Open-ended questions were analyzed for content by a research assistant (TJ) and grouped into major themes. The grouping was confirmed by a psychiatrist (LJK), and discrepancies were resolved by discussion to reach consensus.
The project was approved by the Research Ethics Board of the Jewish General Hospital.
Results
The mean±SD age of consultants was 41.9±11.0 years. Most consultants (N=39, or 65%) were women. There were 18 physicians (30%) (ten psychiatrists, five psychiatry residents, and three general practitioners), 14 psychologists (23%), 17 social workers or related professionals (28%), and 11 non-health professionals or paraprofessionals (18%) (for example, anthropologists and community workers). Ethnocultural backgrounds included Euro-Canadian (N=11, or 18%), Middle Eastern (N=12, or 20%), South Asian (N=9, or 15%), European (N= 7, or 12%), African (N=5, or 8%), Caribbean (N=4, or 7%), East Asian (N= 4, or 7%), Hispanic or Latino (N=4, or 7%), and other (N=4, or 7%).
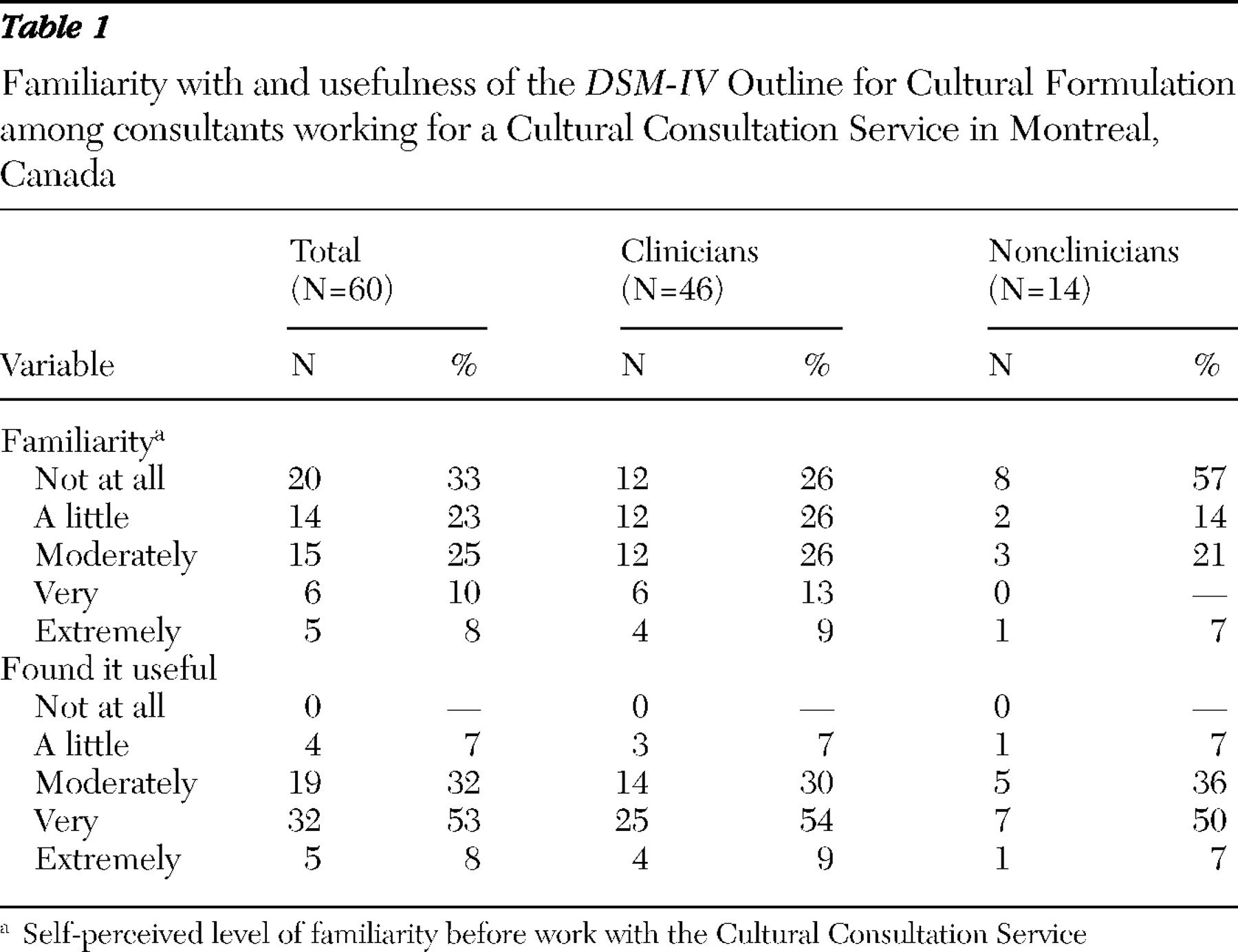
Table 1 presents results on perceived familiarity and usefulness of the cultural formulation. More than half of consultants and culture brokers (N=34, or 57%) reported little or no prior familiarity before working with the CCS; only 11 (18%) were very or extremely familiar with the cultural formulation. There was a trend for clinicians to be more familiar than nonclinician culture brokers with the cultural formulation (p=.06). Among clinicians, 65% (26 of 40 clinicians) had never used the cultural formulation previously, and only seven (18%) had used it more than five times.
Most respondents (N=56, or 93%) found the cultural formulation moderately to extremely useful; perceived usefulness did not differ between clinicians and nonclinicians. In their CCS work, 47 respondents (78%) reviewed the cultural formulation before interviewing patients in order to guide the interview and 55 (92%) reviewed the cultural formulation after the interview in order to organize the report. Nonphysicians (median=3.00, interquartile range=2.00–3.00) found the cultural formulation significantly more useful than did physicians (median=2.00, interquartile range=2.00–3.00) (p=.02); this difference was maintained when psychologists (median=3.00, interquartile range=2.75–3.25) were compared to physicians (p=.04) (median=3.00, interquartile range=2.75–3.25; 11 psychologists, or 79%, found the cultural formulation very or extremely useful, and seven physicians, or 39%, found the cultural formulation very or extremely useful) (p=.02). None of the other comparisons of the three professional groups (physicians, psychologists, and social work-related practitioners) were significant regarding utility or familiarity with the cultural formulation.
The professional groups differed in terms of diversity. Psychologists spoke more languages (median=3.00, interquartile range=2.75–4.75) than psychiatrists (median=3.00, interquartile range=2.00–3.00) (p=.03). In addition, there were more psychologists than psychiatrists of non-European heritage (11 psychologists, or 79%, compared with five psychiatrists or psychiatric residents, or 33%) ( χ 2 = 5.24, df=1, p=.02). Social work–related professionals also spoke more languages (median=3.00, interquartile range=2.50–4.00) than psychiatrists, although this finding was not significant. Also, social work-related professionals were more likely to be from non-European backgrounds (14 social work-related professionals, or 82%) ( χ 2 =7.9, df=1, p<.01).
Most consultants (N=46, or 77%) found the cultural formulation useful as a framework, guide, or organizing structure during and after the interview, thus aiding with the assessment or report writing process. Some consultants (N=20, or 33%) specified certain sections as particularly useful (for example, migration history), while others noted the cultural formulation facilitated understanding the patient or aspects of the case (N=10, or 17%), aided with evaluation (N=8, or 13%), promoted openness and cultural sensitivity (N=5, or 8%), and helped guide treatment planning (N=4, or 7%). Four consultants (7%) suggested that the cultural formulation would be most helpful for those with less experience in cultural assessment. Some consultants (N=18, or 30%) found the expanded cultural formulation too lengthy, detailed, or cumbersome to use, but several (N=5, or 8%) noted that the length and detail would be helpful for a less experienced consultant.
Even with the expanded version, consultants felt that certain conceptual information or clarifying details were missing (N=16, or 27%). They reported that there was insufficient attention to migration history and to religious identity, practice, and spiritual experience; that there was no clear place for socioeconomic and social structural issues; and that there was no guidance on how to collect information or integrate it into an overall formulation. In some cases (N=10, or 17%) the consultants felt that the content of the cultural formulation was not sufficiently oriented to specific cultural groups or did not inquire into crucial aspects of social and cultural context. This was especially true for refugees and indigenous peoples.
Recommendations for improvement of the cultural formulation included additions or changes to its structure, content, and implementation. Nine consultants (15%) suggested developing a shorter form (for example, a semistructured interview or checklist) or separate training version. With regard to content, the consultants recommended listing information needed to clarify ethnocultural and sociopolitical identity with a higher degree of specificity (for example, to distinguish relevant ethnic and socioeconomic differences between regions within a country), including detailed sections on migration (for example, to track multiple migrations, problems in adjustment, and losses), strengthening the family and developmental sections, and making modifications for First Nations or Inuit clients (for example, integrating information on acculturation). Other suggestions included giving explicit attention to the relationship between the patient and the culture broker or the interpreter, establishing a time line of help seeking, and making explicit links with treatment interventions.
In terms of use, nine consultants (15%) suggested that there was a need for changes in training and institutional practices to promote the use of the cultural formulation. Suggestions included promoting awareness of the cultural formulation in training and clinical settings, providing specific training that goes beyond the guidelines, and considering the role of different resource people in collecting different aspects of the data. In particular, it was suggested that professionals need training in working with interpreters and culture brokers and in addressing the sensitive nature of some types of information (for example, information related to trauma).
Discussion and conclusions
This is the first assessment of the perceived usefulness of the cultural formulation and demonstrates that consultants working in the setting of a specialized CCS find the cultural formulation to be a useful tool. Many cultural consultants and culture brokers (both clinical and nonclinical) were unfamiliar with the cultural formulation before their work with the CCS. This lack of familiarity may have been due to the limited training and professional continuing education available on the use of the cultural formulation. Nonmedical consultants (especially psychologists) found the cultural formulation more useful than did physicians. This difference in perceived utility could not be explained by any significant differences in perceived familiarity between these two professional groups, but it may reflect greater ethnocultural and linguistic diversity within the nonphysician group. Different emphases in training or working conditions between psychologists and physicians also may have contributed to this difference in perceived utility of the cultural formulation.
This study also examined the use of the expanded version of the DSM-IV Outline for Cultural Formulation by nonclinicians working as culture brokers. Although such nonclinical culture brokers tended to be less familiar with the cultural formulation, they found it comparably helpful in their work. This suggests that the cultural formulation is readily applied to organizing cultural information and supports its use by nonclinical consultants or culture brokers, when appropriate.
The main suggestions for refinement of the cultural formulation centered on adding sections to address the experience of specific ethnocultural groups or populations, including religious identity and religious practices and expanding sections on migration history. Other suggestions included providing various versions of the cultural formulation, including a checklist. The aim of this more detailed outline is to capture the salient dimensions of cultural variation in clinical populations, enabling clinicians to go beyond stereotypes to a clinically useful picture of how social context, knowledge, and practice shape illness experience (
12 ).
The study had important limitations. The sample size was small and although the consultants were diverse, they were drawn from only one geographical region. Because the respondents in this survey were working for a specialized CCS, the results may not be generalizable to the general population of mental health providers. Nonetheless, this study provided preliminary evidence for the clinical usefulness of the DSM-IV Outline for Cultural Formulation. Studies to examine the impact of the use of the cultural formulation on clinical outcomes are urgently needed to support efforts to address culture in professional training and practice standards, as well as upcoming revisions of DSM.