Problematic substance use is common among individuals with psychiatric disorders (
1,
2,
3,
4,
5,
6,
7 ). For patients treated in inpatient psychiatric settings, the presence of a substance use disorder is a strong predictor of poor prognosis and subsequent rehospitalization (
7,
8,
9,
10 ). Given the high prevalence of substance use disorders among psychiatric inpatients and the established relationship between substance use and poorer outcomes, psychiatric treatment programs need to develop and implement successful strategies for patients with co-occurring psychiatric and substance use disorders (
11 ).
Research suggests that enhancing utilization of continuing care for both psychiatric and substance-related problems can lead to improved treatment outcomes, such as reduced likelihood of rehospitalization (
12,
13,
14,
15,
16,
17 ). Accordingly, many inpatient psychiatric treatment programs take explicit steps to link patients with appropriate psychiatric and addictions treatment services after discharge (
11,
16,
18 ). Despite a clear rationale for improving the utilization of continuing care among patients with co-occurring disorders, research on its effectiveness for this patient population is still preliminary (
19 ).
Current performance measures by the Health Employer Data and Information Set and the Washington Circle emphasize the importance of enhancing continuing care engagement (
20,
21 ). These performance measures highlight the value of rapid engagement (within 30 days of discharge) as a core component of continuing care. To the best of our knowledge, no one has explicitly evaluated the comparative influence of continuing care for psychiatric and substance use disorders among patients with co-occurring disorders.
Given the high cost of providing inpatient psychiatric treatment and the high risk of readmission among patients with co-occurring disorders, it is important to examine the association between continuing care and the likelihood of subsequent inpatient psychiatric treatment for these patients. This study used treatment records of patients with co-occurring psychiatric and substance use disorders who received inpatient care (the index episode) in the Department of Veterans Affairs (VA) within a given year. After describing the characteristics of patients who received continuing care within 30 days of discharge and after we controlled for baseline and index treatment-related predictors, we determined the relative associations between psychiatric continuing care, substance use disorder continuing care, and their combination and the risk of readmission within 90 days after discharge.
Methods
Procedures
The sample was derived from electronic treatment records for all patients discharged from inpatient or residential psychiatric programs between July 1, 2004, and June 30, 2005, according to the VA's National Patient Care Database (
22 ). To qualify for the sample, a patient had to have received diagnoses of an axis I psychiatric disorder and a substance use disorder during the index psychiatric episode. Qualifying diagnoses were defined by the
International Classification of Diseases, 9th revision, Clinical Modification diagnostic codes. Institutional review board approval was obtained for all analyses.
The patient's first qualifying psychiatric stay during the selection time frame was defined as the index episode. However, if a patient was discharged and then readmitted for another psychiatric stay within one day, the two stays were considered to be continuous. Medical records were used to determine whether patients died during the study period, and patients' records were censored in the event of patients' death.
Measures
Psychiatric rehospitalization. As our primary outcome, we determined whether each patient had been readmitted to psychiatric inpatient or residential treatment within 90 days after discharge from the index episode. For those who were readmitted, we determined the length of time from discharge to readmission. Patients not readmitted during the 90-day period were censored from the study at 90 days. For a set of supplementary analyses, we used a similar approach to examine readmission in the 365 days after discharge.
Demographic information. Demographic information available for each patient included age, gender, race and ethnicity (categorized into Caucasian versus "other or unknown"), marital status, and a measure of service-connected status, which indicates whether the patient's disorder was considered to be connected to his or her military service, thus making the patient eligible for benefits.
Substance use disorder and psychiatric diagnoses. All diagnoses were drawn from the treatment records during the index episode.
Psychiatric treatment. We determined the number of weeks of inpatient psychiatric treatment in the year before the index admission and calculated the length of the index stay in weeks. Next, we determined whether the patient received continuing outpatient psychiatric care in the 30-day period after discharge from the index episode and before any subsequent psychiatric rehospitalization and the day on which this care occurred. This information was used to create a time-dependent indicator variable of psychiatric continuing care (coded no or yes).
Substance use disorder treatment. We used the same procedure just described to determine whether the patient received any outpatient treatment for substance use disorder and the timing of this care. Timing of care was used to examine continuing care for a substance use disorder in the first 30 days as a time-dependent indicator variable. Similarly, we created a mutually exclusive indicator of whether patients received treatment for both psychiatric and substance use disorders in the first 30 days after the index episode. For the creation of the time-dependent indicator of receiving care for both psychiatric and substance use disorders, we used the first day that patients received the second category of care. For example, if a patient received psychiatric care on the third day and substance use disorder care on the seventh day, the time-dependent indicator for psychiatric and substance use disorder care indicated that this care was received on the seventh day.
Statistical analyses
First, the sample was classified into four groups on the basis of patients' participation in continuing care in the 30 days after discharge—that is, no care, substance use care only, psychiatric care only, or both substance use and psychiatric care. Baseline differences between these four groups were examined with either Kruskal-Wallis nonparametric analysis of variance by ranks or chi square tests. For post hoc comparisons, we used Dunn's multiple-comparisons test for continuous variables or Tukey-type multiple-comparisons tests for proportions for categorical variables (
23,
24,
25 ). A chi square test was used to examine differences in unadjusted rates of readmission in the four groups. Next, we used a Cox regression that included the diagnostic and treatment-related variables as covariates and time-dependent indicators of whether the three categories of continuing care were received within the first 30 days after the index episode (
26,
27,
28,
29 ). To examine the longer-term impact of continuing care, in a supplementary analysis we repeated the Cox regression analysis of risk of rehospitalization in the 12 months after the index episode.
Results
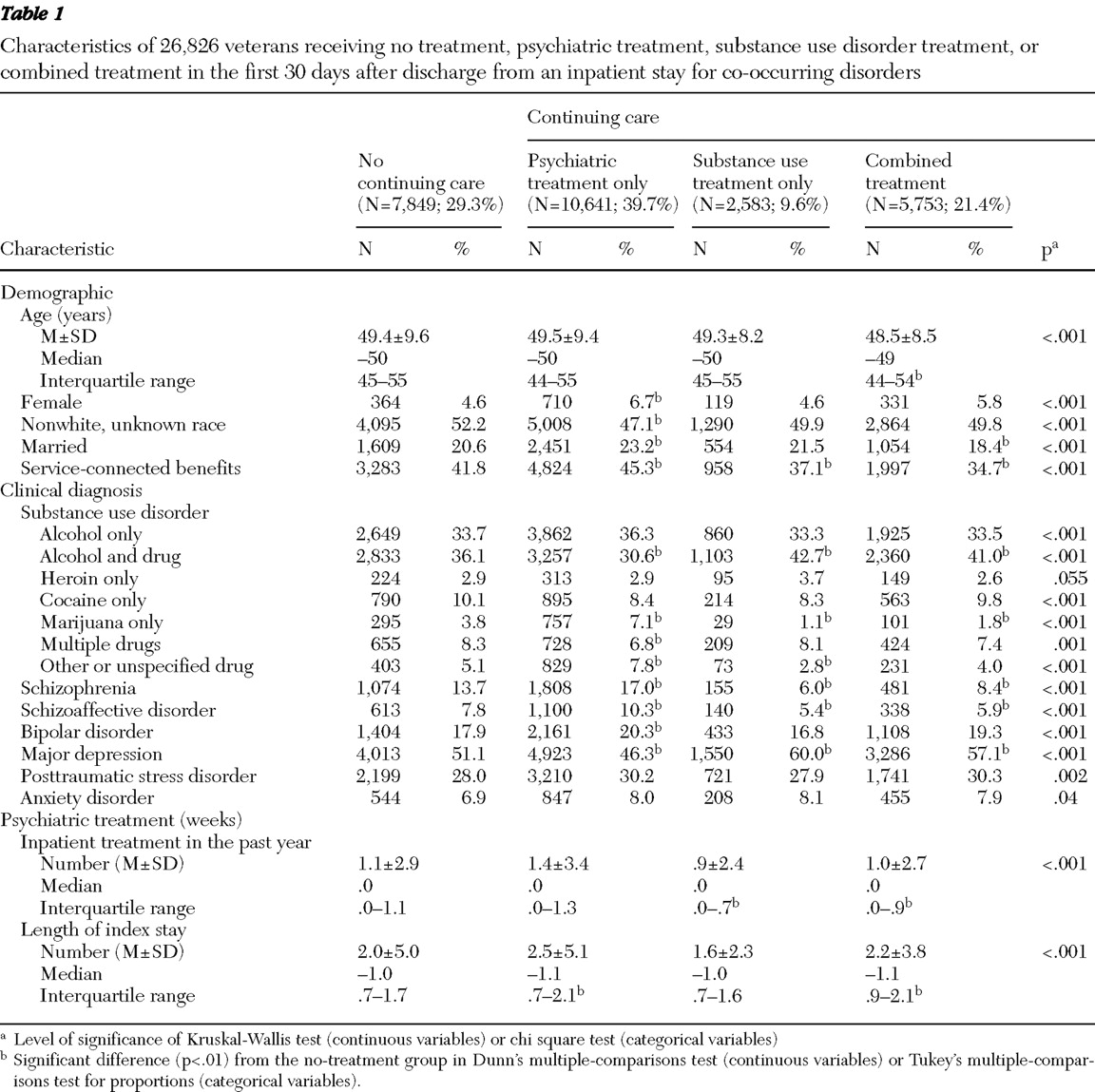
We identified 26,826 patients who met the qualifications for inclusion. Of these patients, 29.3% (N=7,849) received no continuing care, 39.7% (N=10,641) received psychiatric care only, 9.6% (N=2,583) received care for only a substance use disorder, and 21.4% (N=5,753) received both psychiatric treatment and substance use disorder treatment in the 30 days after the index episode of care.
Patients who received both psychiatric treatment and substance-related continuing care were significantly younger and less likely to be married than those who received no continuing care (
Table 1 ). Individuals in the psychiatric care-only group were more likely to be female and married than those in the no-continuing-care group and less likely to be of nonwhite or unknown race. The group receiving continuing care for a substance use disorder and the group receiving combined psychiatric and substance use disorder treatment had fewer patients with service-connected conditions, and the psychiatric care group had more such patients than the no-continuing-care group.
Compared with patients who received no continuing care, patients in the psychiatric care group were more likely to have a marijuana use disorder or an unspecified drug-related diagnosis and less likely to be diagnosed as having both an alcohol use disorder and a drug use disorder or a diagnosis of a drug use disorder for multiple drugs. Patients in the psychiatric care group also had higher rates of schizophrenia, schizoaffective disorder, or bipolar disorder and lower rates of depression than did those with no continuing care. The substance-related treatment group and the combined-care group both had higher rates of combined alcohol and drug use diagnoses and lower rates of use of only marijuana than the no-continuing-care group. Also, compared with the no-continuing-care group, the groups receiving continuing care for only a substance use disorder or for psychiatric and substance use problems had significantly lower rates of schizophrenia and schizoaffective disorders and higher rates of depression.
Patients in the psychiatric care and the combined treatment groups had longer index stays than the no-continuing-care group. Those treated for a substance use disorder only and those with combined treatment had fewer days of prior inpatient psychiatric treatment than the no-continuing-care group.
Within 90 days after discharge, 23.4% (6,280 of 26,826) of the sample was rehospitalized for psychiatric care. By group, 25.4% (1,991 of 7,849) of the no-continuing-care group was rehospitalized versus 24.7% (2,625 of 10,641) of the psychiatric care group, 19.7% (510 of 2,583) of the substance abuse treatment group, and 20.1% (1,154 of 5,753) of the combined continuing care group ( χ 2 =81.5, df=3, p<.001). In multiple-comparisons tests for proportions, the group receiving continuing care for a substance use disorder and the group receiving combined continuing care differed from the no-continuing-care group and the psychiatric care group (p<.01 for all comparisons), but not from each other. The no-continuing-care and the psychiatric care groups did not differ significantly from one another.
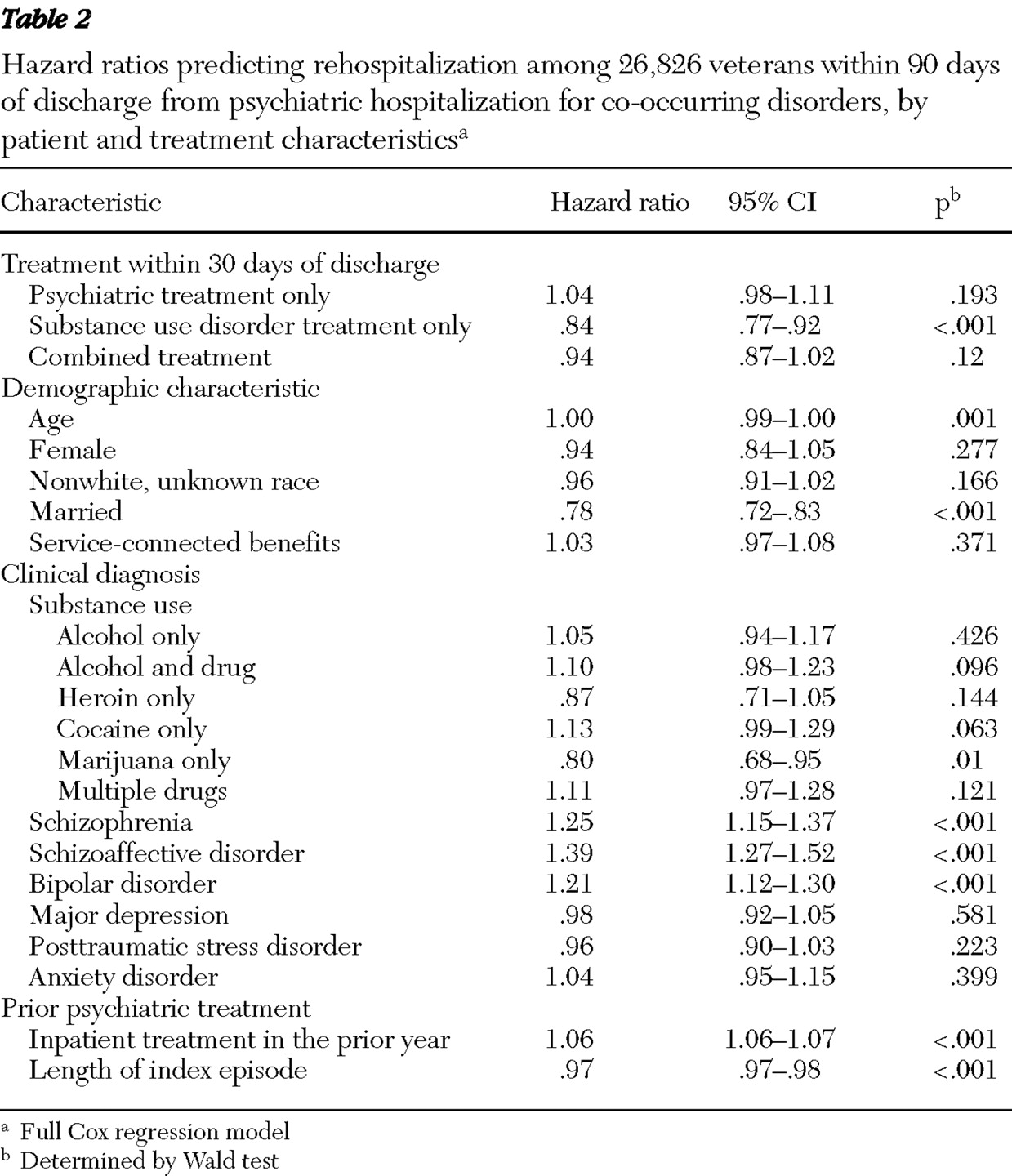
Table 2 shows the results of the full Cox regression model, which included all variables from
Table 1 as predictors, as well as measures of continuing care participation, which were entered as time-varying indicators. A total of 26,681 patients were included in the analysis (145 were dropped from the analysis because of missing data on marital status). Continuing care for substance use disorder was associated with a 16% (95% confidence interval=8%–23%) reduction in the risk of rehospitalization in the 90 days after the index episode compared with no continuing care. Psychiatric treatment and combined psychiatric and substance use disorder treatment were not significantly associated with readmission.
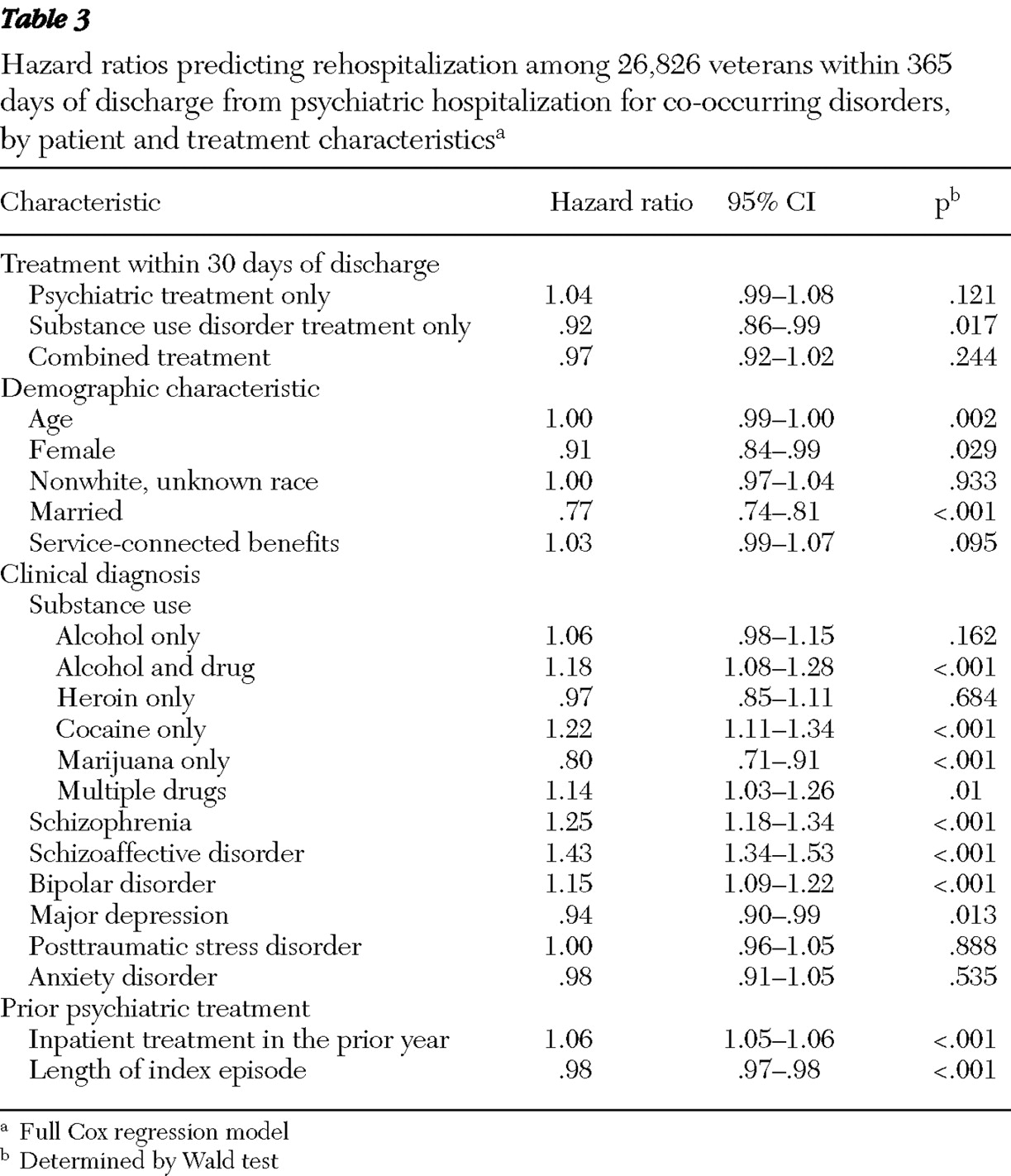
In a supplementary analysis, we repeated our Cox regression analysis to examine the associations between effects of the same set of predictors and risk of rehospitalization in the 12 months after the index episode. The results were similar except that the association between continuing care for a substance use disorder and rehospitalization, although still significant, was diminished. In addition, the associations between some patients' personal characteristics (diagnoses of alcohol and drug use disorders, cocaine use disorder only, and multiple-drug-use disorder) and rehospitalization were stronger (see
Table 3 ).
Discussion
Analyses of a national sample of all patients with co-occurring psychiatric and substance use disorders treated in VA inpatient psychiatric treatment during one year indicate that over 23% of these patients were readmitted for additional inpatient psychiatric treatment within 90 days. Time to readmission was influenced by pretreatment patient characteristics, aspects of the episode of care, and continuing care soon after discharge. In particular, receipt of postdischarge substance use disorder outpatient treatment predicted a lower likelihood of rehospitalization. Receipt of psychiatric continuing care, either alone or in combination with substance use disorder continuing care, was not associated with reduced risk of rehospitalization.
In this sample of patients with co-occurring disorders, those who were younger, unmarried, and diagnosed as having schizophrenia, schizoaffective disorder, or bipolar disorder were more likely to be rehospitalized. The pattern of results is broadly similar to what has been described in more general samples of patients with psychiatric disorders (
7,
8,
9 ). These findings suggest that patients with fewer personal resources, such as being unmarried, and those with a psychotic disorder are at particularly high risk of readmission. In addition, a longer length of stay in the index treatment episode was associated with a lower likelihood of readmission. Previous research has yielded inconsistent results about the impact of length of stay, which has been associated with both a lower (
30,
31 ) and a higher (
32 ) likelihood of readmission. This discrepancy in findings is likely a result of the tendency for patients with more severe illness to receive longer stays. Within our sample, it is possible that a longer index stay allowed for greater stabilization of the patients' symptoms or provided an opportunity for better discharge planning. Also, programs that provided longer episodes of index treatment may have had other attributes that allowed for more effective inpatient or postdischarge treatment.
Although it may seem straightforward that treatment of patients with co-occurring disorders should involve both psychiatric and substance use disorder treatment (
19 ), only 21% of the patients in this sample attended at least one session of both forms of continuing care. Yet over 70% of the sample attended at least some form of postdischarge continuing care within 30 days of discharge. A small minority of patients (9.6%) received continuing care for a substance use disorder only. This low proportion may reflect the fact that few patients with co-occurring psychiatric and substance use disorders are referred to only substance use disorder treatment. Also, it is possible that substance use disorder treatment providers are hesitant to accept individuals with co-occurring psychiatric disorders unless those individuals also receive concurrent outpatient psychiatric treatment. Involvement in postdischarge treatment for a substance use disorder was associated with a lower likelihood of rehospitalization even after analyses controlled for other patient-related and index episode-related predictors. This finding is consistent with several other studies that provide evidence for the importance of improving engagement in continuing care (
14,
17,
33 ).
These findings provide empirical support for current performance measures designed to encourage use of continuing care (
20,
21 ). The findings also highlight the importance of examining continuing care beyond the 30 days postdischarge. In our analyses, there was a significant association between continuing care for a substance use disorder and a lower risk of subsequent hospitalization, although it was somewhat smaller over the course of 12 months than over 90 days. This suggests that current performance measures, which focus on initial engagement in continuing care, could be supplemented by an improved understanding of the importance of sustained participation.
The lack of a consistent significant protective relationship between psychiatric continuing care and risk of rehospitalization was surprising. This may reflect the fact that psychiatric continuing care is provided for patients with the most severe psychiatric problems who remain at high risk of rehospitalization despite the potential benefits of this form of treatment. This explanation is consistent with our finding that patients who received psychiatric continuing care had higher rates of serious mental illness than patients who received either continuing care for a substance use disorder or no continuing care. It is also possible that because our sample was recruited from psychiatric settings, patients discharged from inpatient care had already achieved some form of psychiatric stabilization and psychiatric continuing care did not account for much additional variance. Also, individuals receiving outpatient continuing psychiatric care may be more closely monitored for deteriorations in functioning and, consequently, more likely to be readmitted after an increase in problematic symptoms.
The findings related to continuing care for a substance use disorder are similar to those of McKay and colleagues (
33 ) and indicate that continuing care may be beneficial for patients with co-occurring disorders, even if this treatment is specifically focused on reducing only problematic substance use. Although more integrated forms of treatment (such as those outlined by Drake and colleagues [12]) are likely to be ideal, these results indicate that in real-world settings that may lack integrated services, providers should still consider referring patients to separate substance use disorder programs for continuing care after discharge.
The observational nature of the study prevents determination of the extent to which any of the predictors in our models directly caused or prevented subsequent readmission. The results presented in
Table 1 show a number of differences between patients who did not receive any continuing care and those treated in psychiatric or substance use disorder treatment settings. These and other unmeasured patient characteristics likely influenced the recommendations and referrals given to patients when discharged from the hospital, the likelihood of their attending continuing care, and their responsiveness to the type of care that they received. In particular, the lack of a significant relationship between psychiatric continuing care and lower likelihood of rehospitalization was unexpected and, as noted earlier, may reflect the fact that patients with more severe psychiatric problems were more likely to receive psychiatric continuing care. Also, despite the statistical significance of the effect of continuing care for a substance use disorder, the effect size was modest, and the high rates of readmission in each group highlight the need for improved interventions among patients with co-occurring psychiatric and substance-related problems.
Because all results were based on analyses of patient treatment records, more finely grained information about patient symptoms, diagnoses, and components of treatment was unavailable. The sample was composed predominantly of male veterans. Also, the measures of race and ethnicity in this study were imprecise. Similarly, the design allowed for the examination of rehospitalization to only VA facilities; rates and predictors of receipt of non-VA care are unknown. Finally, although we have focused on predicting readmission as a proxy for poor outcome, in some cases, readmission can be an indicator of better patient self-awareness and may reflect a treatment system that is responding more effectively to the patients' needs (
34 ). However, given the personal and economic cost of inpatient treatment for patients and the health care system as a whole, in many cases rehospitalization is a negative outcome.
Conclusions
Despite these limitations, this study is a first attempt to understand the interrelationships between patient functioning, index treatment, postdischarge continuing care, and readmission to psychiatric treatment in a large national sample of patients with co-occurring psychiatric and substance use disorders. Although guidelines highlight the importance of integrated care for patients with co-occurring disorders (
12,
13,
35,
36 ), only 21% of these patients were contacted for both psychiatric treatment and substance-related treatment within 30 days of discharge from inpatient psychiatric treatment. Receipt of postdischarge substance use disorder treatment was consistently associated with decreased likelihood of psychiatric readmission. Although preliminary, this finding provides initial information about the type of care that could be beneficial for patients with co-occurring disorders discharged from inpatient psychiatric treatment. An important next step is to conduct randomized controlled trials of the impact of specific linkage strategies on rates of continuing care attendance, rehospitalization, and patient functioning. Results from a pilot study with this design are consistent with our findings and indicate that this line of research may be promising (
17 ).
Acknowledgments and disclosures
This work was supported by Merit Review Entry Program Award MRP 05-137 from the Department of Veterans Affairs (VA) Health Services Research and Development Service. This funding was in the form of a career development award and did not directly shape the design or conduct of this specific study. The views expressed in this article are those of the authors and do not necessarily represent those of the VA.
The authors report no competing interests.