Schizophrenia is a chronic psychiatric illness affecting 1% to 2% of the population. Unfortunately, suboptimal follow-through with treatment too often leads to a classic revolving-door pattern of relapse and rehospitalization. The annual cost of schizophrenia to the United States is $33 billion, with direct patient care accounting for more than half of that expense (
1 ).
Work in the past two decades has documented that community consumer support and family psychoeducation programs can significantly enhance posthospital discharge care of individuals with schizophrenia (
2,
3,
4,
5 ). Outpatient psychoeducation programs have been found to be helpful to patients with schizophrenia and their families, as well as cost-effective in reducing the need for inpatient care (
6,
7,
8 ). McFarlane's group (
8 ) documented a cost-benefit ratio of 1:34 for their multifamily group psychoeducation program: every dollar spent on the program yielded an overall savings of $34 in other treatment costs. Most of the financial gain was realized from reductions in subsequent hospitalization. The benefits of psychoeducation have the potential to be long lasting, up to seven years (
9 ), although most studies have not shown such enduring benefit (
10 ).
Potential benefits of psychoeducation have had insufficient focus in environments where it is likely to have the greatest impact: the inpatient setting, commencing at the point of contact with patients in the most severe phase of illness. Because costs of inpatient treatment far exceed outpatient costs (
11 ), this represents a potential source of savings. A recent comprehensive meta-analysis by Lincoln and colleagues (
10 ) identified seven randomized controlled trials utilizing inpatient or combined inpatient-outpatient family psychoeducation. None of these inpatient psychoeducation studies were conducted in the United States. Only four family psychoeducation programs in this review provided follow-up data on relapse or rehospitalization. Effect sizes ranged from .00 to .60 (mean .35) at one to six months and .12 to .69 (mean .55) at seven to 12 months postintervention. The study by Lincoln and colleagues concluded that family psychoeducation showed benefit over patient-only psychoeducation and that gains were observed in relapse prevention but not in symptom reduction, functioning, knowledge, or adherence.
Although the published literature has provided evidence for the efficacy of psychoeducation in academic settings, similar studies have not provided sufficient evidence of effectiveness of psychoeducation in real-world psychiatric treatment settings, such as in private practice. This randomized controlled study was conducted to determine whether efficacy for psychoeducation demonstrated in academic settings could be translated to effectiveness in nonacademic environments.
Schizophrenia Treatment and Education Programs (STEPS), an intensive family psychoeducation program specifically designed as an inpatient-initiated intervention for schizophrenia in a private-sector practice, is unique in not being based on any other existing psychoeducation program. It extends the capabilities of established psychoeducation models that are limited only to outpatients to begin the intervention during acute inpatient care, when the severity of illness and treatment intensity are maximal and the potential for benefit is large. The STEPS program translates the efficacy of psychoeducation demonstrated in academic environments into effectiveness in private-sector settings. The objective of this randomized controlled trial was to test the potential for the STEPS psychoeducation program to reduce subsequent need for rehospitalization, generating potential cost savings in private-sector care for schizophrenia.
Methods
Individuals eligible for the study included patients aged 18 or older with a diagnosis of schizophrenia who were voluntarily admitted to the Christian Hospital Northwest inpatient service in St. Louis, Missouri, between July 2001 and March 2003. All study participants had to be well enough to participate in the program and willing to be randomly assigned to usual care or the STEPS program. During the study enrollment period, 57 of 85 (67%) consecutive study-eligible patients enrolled in the study, with 28 declining participation. An additional 59 patients had illness so severe that they could not provide informed consent, complete study assessments, or join in organized activities of a psychoeducation program. A six-month follow-up study was completed, with 31 (54%) of the original 57 located and reassessed. There were no statistically significant differences between those reassessed and those lost to follow-up in terms of any demographic variable, duration of illness, symptom severity at baseline, recent history of use of inpatient or outpatient substance abuse services at baseline or use of other psychiatric services at baseline, or randomization to STEPS or the usual program.
Approval for both the index and follow-up parts of the study was obtained from the institutional host of the study, the Washington University School of Medicine Institutional Review Board. All participants provided written informed consent before the assessments at both time points and before treatment group randomization.
At baseline a computerized randomization program selected 26 patients for the STEPS program and 31 for usual care. All patients in both groups continued all other aspects of their treatment, meeting with their usual psychiatrists and being encouraged to take their medication as prescribed. Their psychiatrists and the research assessment team were blinded to patients' random assignment to STEPS or to usual care.
Usual care is the standard treatment routinely provided by psychiatric inpatient units and is received by all patients at this hospital, including those participating in STEPS. All patients at this hospital attend four to five hours of educational mental health classes seven days a week that are nonspecific to type of illness and address basic self-care and healthy lifestyles, coping skills, self-esteem, socialization skills, anger and stress management, communication with the treatment team, and the importance of participating in treatment (including taking medication and attending appointments). Group sessions allowed patient ventilation about personal issues or the hospital environment.
The STEPS program is tailored to the progress of patients through the system of care, starting during the inpatient stay and proceeding through achievement of residential stability with families or even independent living. All patients in STEPS participate in usual care as described above. The inpatient segment of the STEPS program offers additional daily structured educational activities for understanding the illness and symptoms of schizophrenia (Symptoms Education Class), and it offers a Managing Your Illness class, which provides coping skills specific to the symptoms (for example, managing hallucinations, paranoia, and delusions), daily living skills specific to the problems of schizophrenia, social skills, and personal development, all geared toward managing the illness. Program activities continue posthospital discharge through partial hospitalization and evening programs in the community and an annual full-day workshop open to the public. Families are encouraged to participate for as long as they wish in the program at every level, including attendance at inpatient family meetings, discharge planning meetings, monthly drop-in meetings for informal support and information, and semiannual picnic programs (
12 ).
A computerized version of the Diagnostic Interview Schedule (DIS) (
13 ) was administered by a trained rater before program participation. With the patient's permission, a close family member provided collateral information to supplement the patient history on the number of previous psychiatric inpatient admissions and utilization of other services by the patient in the past six months. Symptom severity was measured at baseline by the Scale for the Assessment of Positive Symptoms and by the Scale for the Assessment of Negative Symptoms (
14 ).
The computerized DIS data were put into an electronic data set, and diagnoses were scored from the raw data. Data from questionnaires and interviews were entered and merged with diagnosis data into a SAS data set. Data are presented as numbers and percentages for categorical variables and as means with standard deviations for numerical variables. Patient and family information about service use was combined into a single item for each service use category. Categorical variables were compared by using chi square analyses (substituting Fisher's exact tests when expected numbers in cells were less than five). Student's t tests were used to compare numerical variables, using Satterthwaite comparisons for data with unequal variances as well as nonparametric analysis (PROC NPAR1WAY in SAS) for determining differences in rehospitalization rates between the two study conditions. Effect sizes were calculated using Hedges' correction for small sample bias to be consistent with findings reported in the review by Lincoln and colleagues (
10 ).
Results
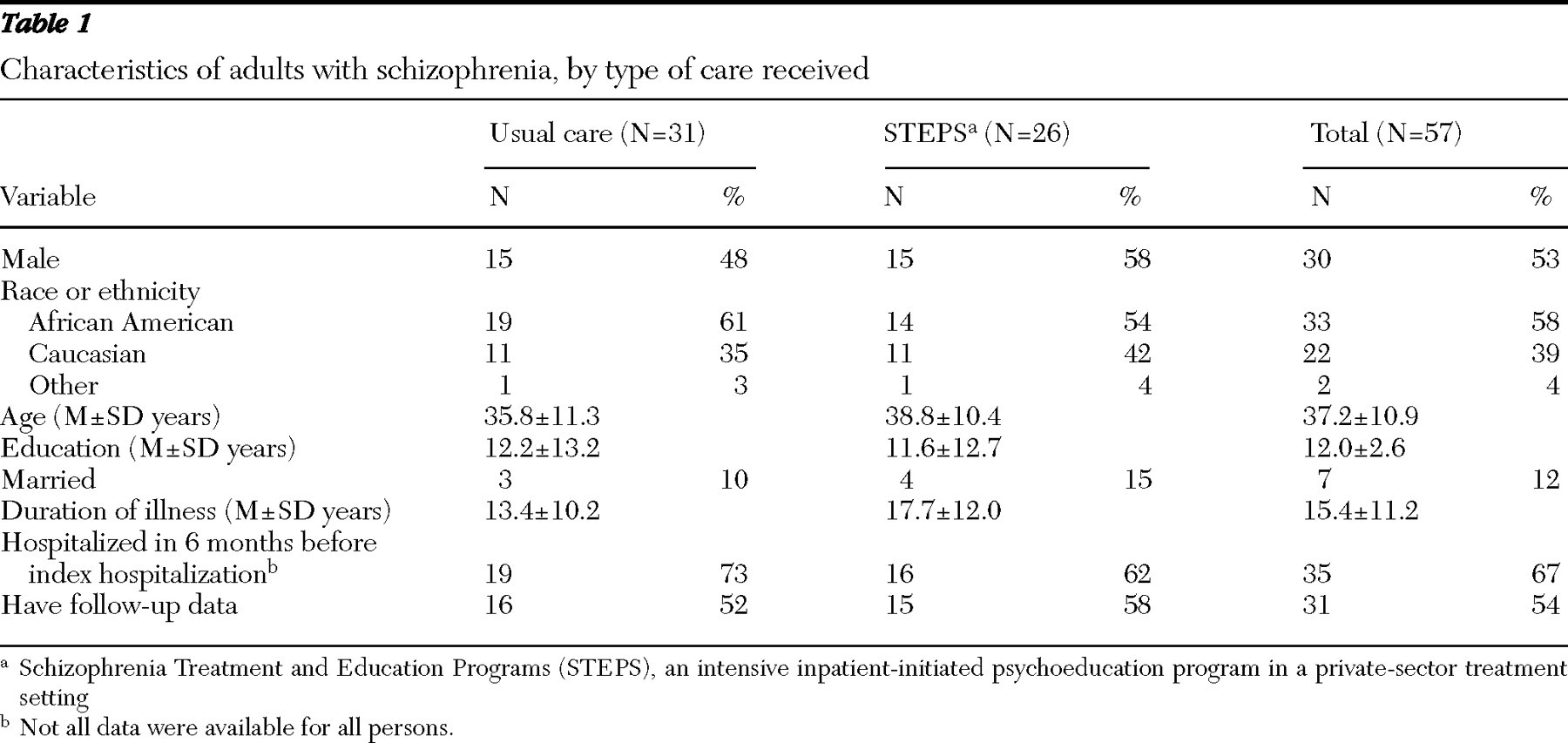
Table 1 provides details of characteristics of the study sample of 57 patients, by group. Slightly more than one-half of the sample was male and African American, the mean age was 37.2 years, and the mean number of years of education was 12.0. Few were married. The mean duration of schizophrenic illness was about 15 years, and more than half had been hospitalized in the six months before the index hospitalization.
At follow-up 31 of 57 (54%) were reassessed. (Funding constraints for the research did not permit aggressive tracking and reenlistment of study participants.) Those in STEPS were not detectably different from those in usual care on any of the baseline variables. The mean±SD length of inpatient stay was 10.7±9.4 days, and patients in STEPS did not differ from those in usual care on this variable. Study attrition between index and follow-up was not associated with gender, age, ethnicity, level of education, marital status, symptom level, or duration of illness at the time of the index hospitalization.
Over the six-month follow-up period, participants in STEPS demonstrated a significant reduction in hospitalization, compared with those receiving usual care. Results showed that nine of 16 (56%) of the usual care patients were rehospitalized in the six-month follow-up period, compared with only three of 15 (20%) STEPS participants ( χ 2 =4.29, df=1, p=.038), an effect size of .76. After reanalysis of the data to assume that all patients who were not reassessed at follow-up had been rehospitalized, the difference dropped to rehospitalization among 24 of 31 (77%) usual care program participants and 14 of 26 (54%) of STEPS participants ( χ 2 =3.54, df=1, p=.060), an effect size of .50. The mean number of rehospitalizations during the six-month follow-up period in the usual care group was 1.6±2.2, compared with .3±.6 in the STEPS group (z=2.24, df=17.3, p=.033), with an effect size of .80.
Discussion
This randomized clinical trial demonstrated that participation in the STEPS psychoeducation program significantly reduced subsequent rehospitalization. An important aspect of this study is the private-sector psychiatric treatment setting of this successful psychoeducation program, a program that translated well-established effectiveness demonstrated in academic or other rarified treatment settings to real-world settings of the private-care sector.
Several methodological strengths of this study merit mention. The STEPS psychoeducation intervention was compared with a control group receiving usual care, and data collection was blind to randomization status. Data were gathered prospectively for the purpose of examining effects of the STEPS program on subsequent hospitalization. Structured diagnostic interviews were used to document the diagnosis of schizophrenia among all patients. The study was limited, however, by the severity of illness of the study population; many were too ill to engage in research or psychoeducation activities, and problems of study attrition in this very ill population over the follow-up period reduced the study's statistical power and the potential representativeness of the data. Despite these difficulties, the study documented a lower rate of subsequent hospitalization among those who participated in STEPS and completed the study.
Larger, more comprehensive studies are needed to replicate these findings and identify the active components of the STEPS program that might be responsible for the apparent reduction in subsequent hospitalization. Given the remarkable cost savings demonstrated in the study by McFarlane and colleagues (
8 ) of a psychoeducation program in an outpatient setting, it should not be surprising to find even larger potential for savings for psychoeducation programs initiated in inpatient settings, where the greatest amount of psychiatric care costs are incurred (
8,
15 ).
Acknowledgments and disclosures
This research was supported by a grant from Barnes-Jewish Hospital Innovations. Dr. Vickar is the medical director of STEPS SM, a program he developed in 1985. The service mark for STEPS ensures that any organization that uses the materials complies with the program as described and as approved by Dr. Vickar. There are no royalties associated with it, and it is not a franchise or network. The contents of this report do not represent the views of the Department of Veterans Affairs.
The authors report no competing interests.