Social anxiety disorder, also known as social phobia, involves persistent fear of one or more social or performance situations in which a person is exposed to unfamiliar people or to possible scrutiny by others. Fear focuses on the potential for embarrassment or humiliation, and impairing avoidance often results (
1 ). Social anxiety disorder is the most common anxiety disorder and the third most common psychiatric disorder, following depression and alcohol abuse (
2 ), with a lifetime prevalence of 12.1% (
3 ). It produces substantial functional impairment even when studies have controlled for concurrent depression, with reduced functioning in a variety of specific life domains (
4 ), including family life and social relationships (
5 ), and in overall quality of life (
6,
7 ). Persons with this disorder experience dysfunction comparable to that reported by patients with obsessive-compulsive disorder and panic disorder and by nonpsychiatric patients with multiple sclerosis, rheumatoid arthritis, and end-stage renal disease (
6 ). It is an early-onset disorder and usually precedes the numerous other psychiatric disorders with which it is highly comorbid (
8 ), raising the possibility that early intervention could reduce the rates and burdens of later developing problems.
In a variety of ways, occupational functioning is also limited among most persons with social anxiety disorder (
9 ). Persons with this disorder turn down job offers or promotions as a result of social fears (
10 ). They report impaired work productivity, with increased absences and reduced performance when at work (
2,
8,
11 ). Their occupational success is also limited by reduced educational achievement (
2,
5,
8,
12,
13 ). Occupational dysfunction leads to heightened levels of unemployment (
14 ), financial dependence (
15 ), and reduced income (
12 ).
Although social anxiety disorder has a negative impact on a variety of vocational domains, it has not been adequately studied with regard to welfare status. Significant welfare policy changes in the United States in the past decade have directed increasing attention toward factors that impede the success of required work attainment activities among welfare recipients (
16,
17 ). Psychiatric disorders are common among welfare recipients and have been shown to increase their reliance on welfare and reduce their likelihood of work attainment (
18,
19,
20 ). Anxiety disorders have been directly linked to chronic unemployment and welfare payments (
21 ), lower income and lowered educational attainment (
2 ), and decreased probability of successful return to work (
22,
23 ).
Given the influence of mental health problems on welfare dependence and the negative impact of social anxiety disorder on occupational function, it is likely that social anxiety disorder among welfare recipients will substantially undermine economic self-sufficiency. The study presented here directly tested the hypothesis that social anxiety disorder impedes self-sufficiency among women receiving welfare by impeding their employment efforts. Documenting the impact of this disorder on women receiving welfare benefits may be a first step toward developing and testing interventions that could enhance quality of life for many families and reduce public economic burden.
Methods
Participants
The women in this study all participated in the Women's Employment Study (WES), a longitudinal survey of welfare recipients in an urban Michigan county. Data for this report were collected from women who participated in the first through fourth waves (that is, approximately annual interviews) of the WES. Fifty-six percent (N=344) of the 609 respondents in the study reported here were non-Hispanic black, and 45% (N=273) were non-Hispanic white. Of the total sample, 23% (N=141) were younger than 25 years, 48% (N=290) were between the ages of 25 and 34, and 30% (N=186) were between the ages of 35 and 54. Just over one-third (N=211, or 35%) were caring for a child under the age of two. A majority were living in poverty, with 62% (N=376) having household incomes below the poverty line in the month before the interview.
The response rate for wave 1 was 86% (753 of 874 persons); for wave 2, 92% (693 of 753 persons); for wave 3, 91% (632 of 693 persons); and for wave 4, 91% (577 of 632 persons). The wave 4 sample therefore consisted of 66% of the original intended sample. Attrition analyses were conducted utilizing administrative data available for the entire universe from which the sample was drawn. These analyses confirmed that, as of wave 3, the data set was representative of the initial wave 1 sample and of welfare recipients in the county overall. The initial sample (that is, wave 1) included randomly selected single mothers between the ages of 18 and 54 who were welfare recipients within the selected urban county, had a racial identity of either black or white (non-Hispanic) and were United States citizens. Because noncitizens and other ethnic or racial groups comprised a very small proportion of the overall welfare caseload, sample size was insufficient to examine these groups in detail.
Study overview
In the fall of 1997 trained interviewers conducted face-to-face interviews with a random sample of 753 women who received welfare in February 1997. Michigan's Family Independence Agency, which administers the state's Temporary Assistance to Needy Families program, provided names and addresses of all single-parent recipients. In accordance with our procedures, which were approved by the University of Michigan's institutional review board, interviewers obtained informed consent from all respondents. Respondents from the wave 1 data collection were reinterviewed in the fall of 1998 and again in 1999 and 2000. In all four waves, information was collected on a comprehensive set of indicators of economic and psychosocial well-being, physical health, mental health, partner violence, demographic characteristics, income, current or most recent job, current welfare status, and work and welfare history. Measures included in the study presented here are described below.
Measures
Interview questions included measures of social anxiety disorder, other mental illness diagnoses, welfare and work status, and a variety of control variables. These were as follows.
Social anxiety disorder. Social anxiety disorder was assessed at waves 2 and 3 via the World Health Organization's Composite International Diagnostic Interview-Short Form (
24 ) (CIDI-SF). The CIDI-SF yields a score that is interpreted as the probability that a respondent would meet full
DSM-IV diagnostic criteria if given the complete CIDI interview. Positive CIDI-SF scores have high rates of classification accuracy; specifically, a positive CIDI-SF score correctly classifies respondents'
DSM-IV status across major
DSM-IV disorders 93% to 99% of the time (
25 ). We applied the CIDI-SF guidelines for defining a dichotomous outcome—that is, whether the respondent meets full nonhierarchical diagnostic criteria for social anxiety disorder. The CIDI-SF assesses disorders in the past 12 months; thus a positive score indicates that the participant would meet
DSM-IV criteria for social anxiety disorder during the past year.
Other psychiatric variables. We also used the CIDI-SF at waves 2 and 3 to designate a dichotomous variable indicating the probability that a given respondent met DSM-IV criteria for major depressive disorder, posttraumatic stress disorder, and alcohol or drug abuse in the past 12 months.
Control variables. In the multivariate analysis, we controlled for a number of demographic variables, health and mental health status, and barriers to employment. Demographic variables included race (black versus white, non-Hispanic), age (respondent's age at each wave in three groups: ages 18 to 24, 25 to 34, and 35 to 54), the number of children given care at each wave (the number of children younger than age three and between the ages of three and five for whom the respondent had primary responsibility in her household), and cohabitation status (whether the respondent was cohabiting with an intimate partner at each wave).
Employment barriers that fluctuated over time were measured at each wave. Partner violence was assessed with a modified version of the Conflict Tactics Scale (
26 ). A dummy variable was created to indicate whether a respondent experienced at least one of six types of severe abuse in the past 12 months. Respondents reported on their physical health, using items from the physical functioning subscale of the 36-Item Short-Form Health Survey (
27 ). Respondents who reported being in fair or poor health and who scored in the lowest age-specific quartile for physical limitations (based on population norms) in a wave were defined as having physical limitations. We categorized respondents as "having a child with a health problem" if a respondent reported that she had a child younger than 18 years who had a physical, emotional, or learning problem that limited his or her activity. Respondents who lacked access to a car or who did not have a driver's license constituted those defined as having a transportation problem.
Employment barriers that were not likely to fluctuate appreciably were measured at a single point in time. Relevant human capital variables were measured at wave 1. Years on welfare was defined as the number of years in which the respondent had received welfare as of the initial interview. Low levels of prior work experience were measured by whether the respondent had worked in less than 20% of the years since she turned 18. Women who had not attained high school graduation or equivalency by the initial interview were designated as having less than a high school education. We measured lack of knowledge of work norms with items adapted from Berg and colleagues (
28 ). Lack of knowledge of work norms was considered a barrier if the respondent recognized less than five out of a set of nine problematic work behaviors as problematic. We included a measure of perceived job discrimination based on respondents' reports of experiencing more than four types of workplace discrimination out of a possible 16; types of discrimination included race, gender, or welfare status (
29 ). Two additional work barriers were assessed in the wave 3 interview: literacy (scoring at fifth grade or lower on the Wide Range Achievement Test [30]) and having ever been convicted of a crime.
Results
The prevalence of social anxiety disorder within the past year was 8% at wave 2 and 8% at wave 3.
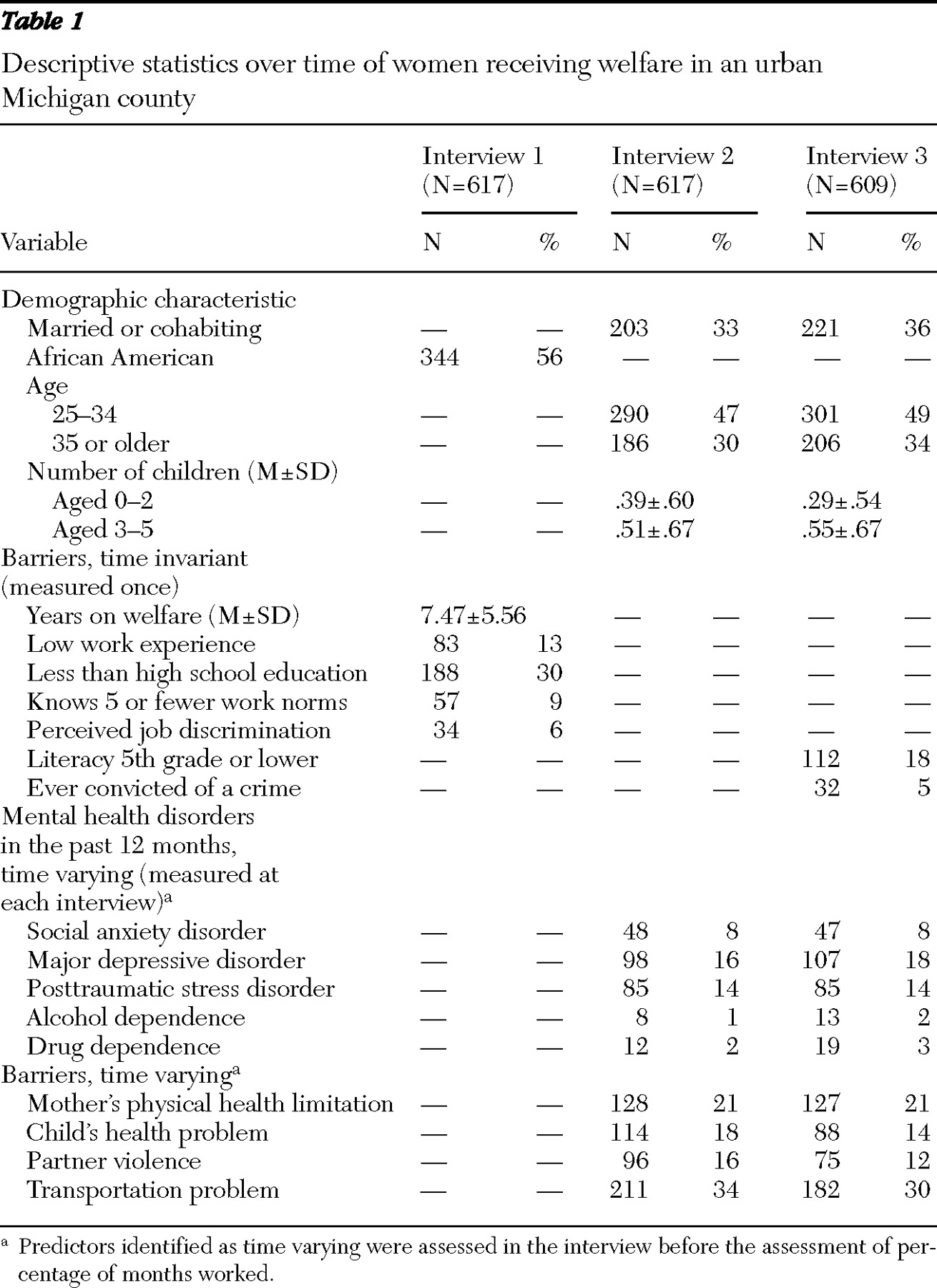
Table 1 describes other relevant demographic variables and independent variables included in the study.
To determine the influence of social anxiety disorder—along with other relevant mental health disorders, demographic characteristics, and human capital variables (for example, job skills and experience)—relevant to work attainment, a linear fixed-effects regression analysis for survey data (
31 ) was done using statistical software from the Stata Corporation (
32 ). This analytic strategy accounts for potential analytic errors that result from repeated measures sampling and clustering without requiring full model specification—that is, all possible relevant predictor variables. It controls for stable differences among people, including the effects of confounding variables that are not explicitly measured, allowing the analysis to focus on the longitudinal effects of predictors that change over time. The dependent variable in these analyses was the percentage of months worked between waves of data collection. Predictors were lagged—that is, they were measured at the interview before each assessment of work—in order to ensure that the measurement of predictors, such as onset of mental health disorders and experience of work barriers, preceded the measurement of work outcomes (for example, social anxiety disorder assessed at wave 2 predicted work outcomes that occurred in the 12 months between waves 2 and 3 and were reported in the wave 3 interview). Structuring the analysis in this way served to clarify the temporal direction of influence.
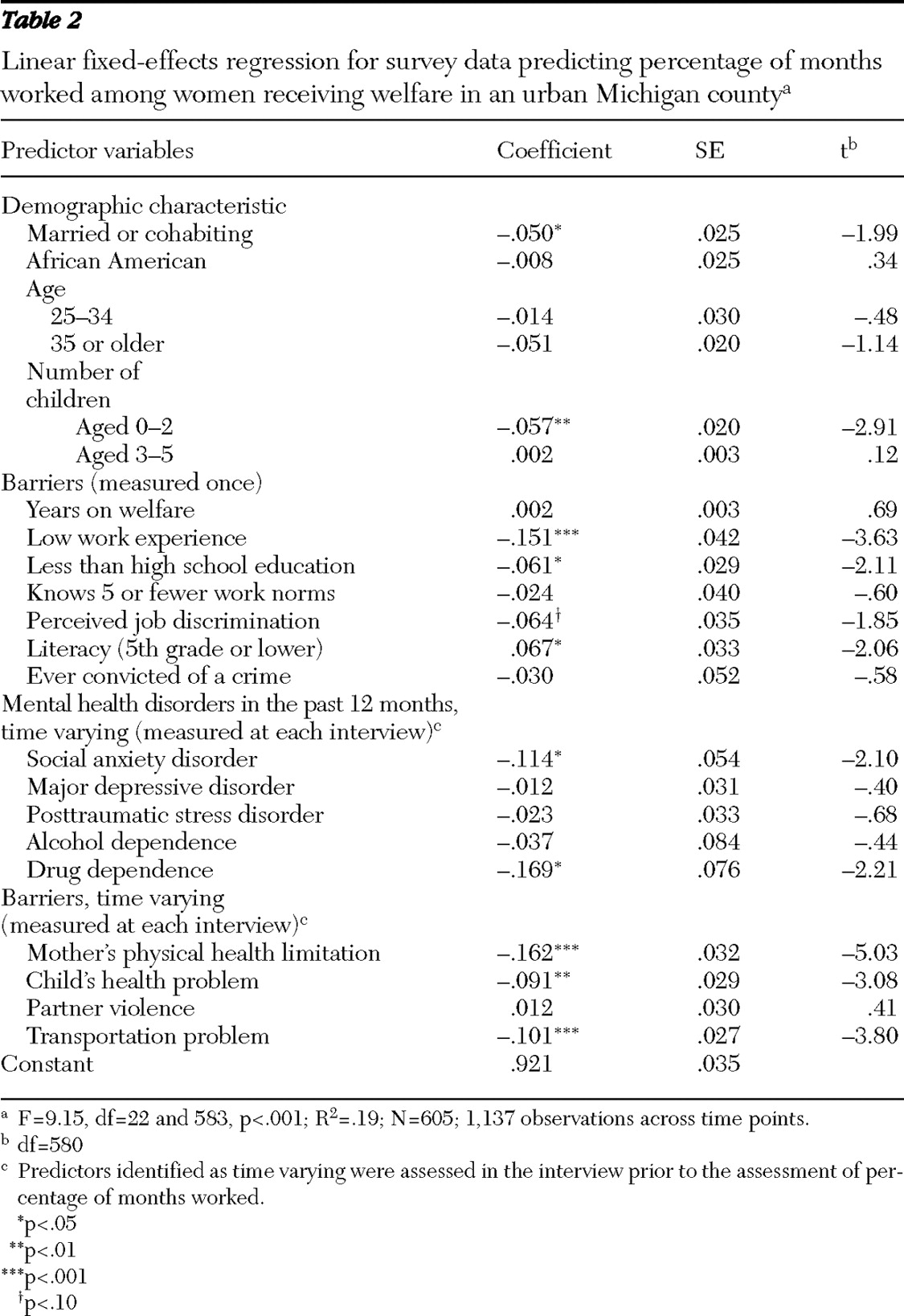
The resulting analysis (presented in
Table 2 ) found several significant negative predictors of work attainment. As hypothesized, social anxiety disorder was negatively associated with percentage of months worked, even after the analyses controlled for other relevant variables, such as demographic characteristics and human capital variables. Other significant predictors of poor work attainment included cohabitation or marriage, having less than a high school education, low literacy, and drug dependence. Additional negative predictors included the number of children younger than two in the recipient's household, as well as having children with health problems. Perceived discrimination tended toward, but did not reach, significance in the model. Low levels of work experience, recipients' health problems, and transportation barriers had the strongest effect sizes in the model. Notably, depression, posttraumatic stress disorder, and alcohol dependence were not significant predictors of the percentage of months worked in this sample. The regression model as a whole accounted for approximately one-fifth of the variance in the percentage of months worked.
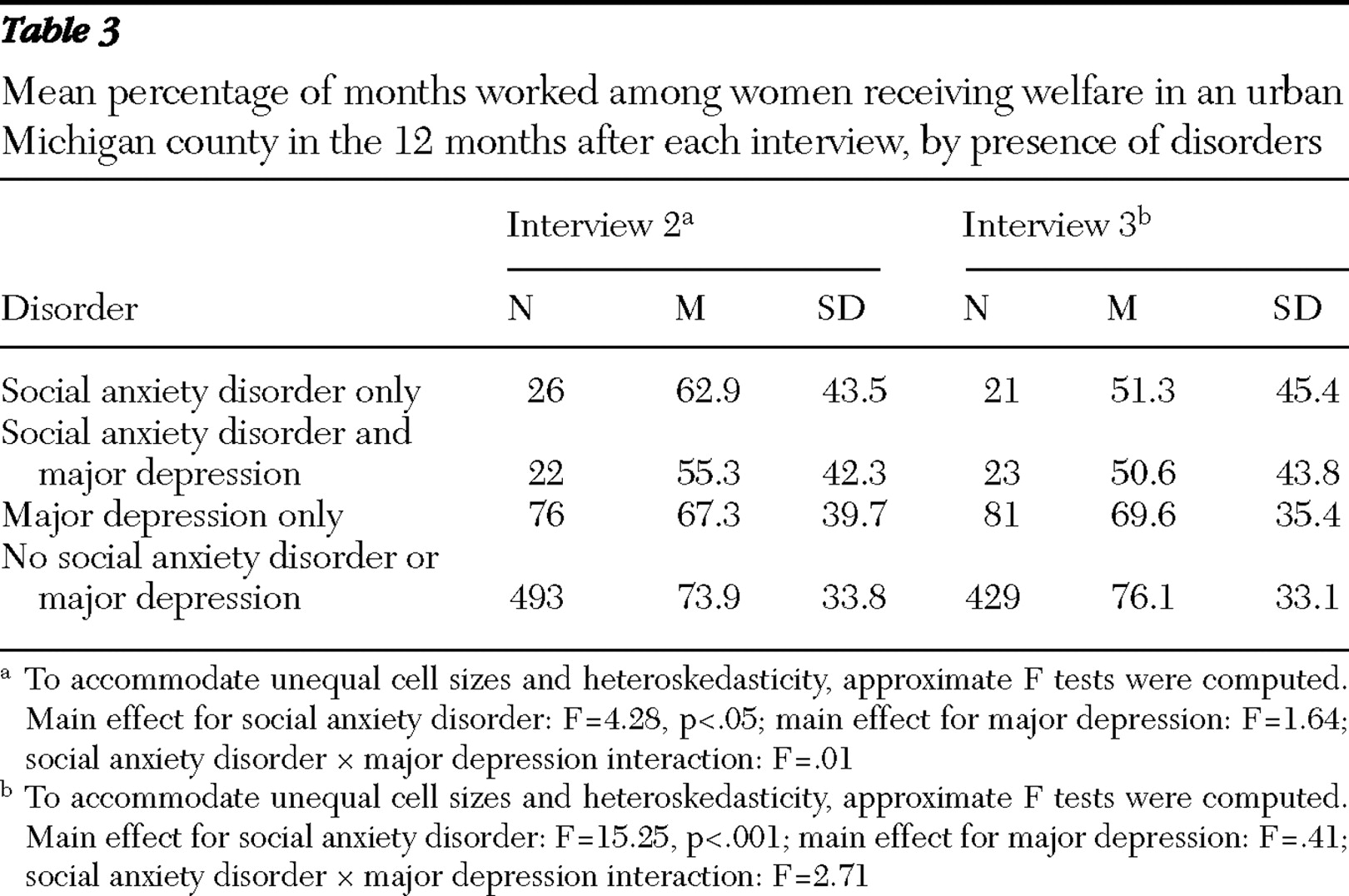
Given the somewhat surprising finding that social anxiety disorder but not major depressive disorder had an impact on work status, we sought confirmation by descriptively examining the percentage of months worked among respondents with social anxiety disorder, major depressive disorder, both disorders, or no disorder. These results are presented in
Table 3 for work in the 12 months after the interviews at both waves 2 and 3. At both time points, the percentage of months worked was lower for women with social anxiety disorder, regardless of the presence of major depressive disorder. For both interviews, statistical tests (two-way analyses of variance using approximate F tests to accommodate unequal cell sizes [33]) indicated a significant effect for social anxiety disorder but not for major depressive disorder or for the interaction between social anxiety disorder and major depressive disorder. These comparisons are consistent with the impression that social anxiety disorder undermined capacity to work and had a clearer impact than depression on this capacity.
Our data allowed us to determine whether women in the study had received mental health services, but they did not include information about whether the women did so for a specific disorder. Our data indicated that women with social anxiety disorder were largely untreated. Only 23% (13 of 48 women) of the women with social anxiety disorder reported ever receiving mental health services in their lifetime for any reason, and only 15% (seven of 48 women) had received mental health services for any reason in the past year.
Discussion
These results demonstrate that the presence of social anxiety disorder was associated with less time worked among mothers on welfare, suggesting that this disorder is a significant impediment to employment for welfare recipients. With the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 and associated legislation, considerable attention has been focused on obstacles to the success of the work attainment efforts that are now required of welfare recipients (
16,
17 ). By adding social anxiety disorder to the list of documented barriers, we have identified an obstacle that should be correctable, since effective treatments for social anxiety disorder are available (
34,
35 ). The potential importance of addressing social anxiety disorder is highlighted by our data indicating that social anxiety disorder appeared to impair work more than depression, which is recognized as one of the most disabling disorders in the world in terms of lost work time (
36 ). Unlike some previous research (
7 ), our study did not find that comorbid depression was associated with greater work impairment for the women in our study. However, depressive comorbidity might be associated with greater disability in other domains that we did not measure.
The impact of social anxiety disorder in inhibiting work efforts for women on welfare should not be surprising given the extensive documentation of its impact on occupational functioning in other populations (
2,
7,
8,
12,
15,
36,
37 ). It is also consistent with the expected social distress and avoidance characteristics of this disorder, which directly undermine efforts to obtain or maintain employment. Although there has been debate about the seriousness and functional significance of very common epidemiologically ascertained mental health disorders (
3,
38 ), our data suggest that social anxiety has a real impact on work efforts and has potentially meaningful consequences among those using the welfare system. Documentation of the prevalence and impact of social anxiety disorder may be particularly important among women on welfare, where psychiatric problems are often unrecognized, rarely treated, and have direct economic impacts at both the individual and social levels.
Our findings also highlight that other barriers remain a significant concern for women in this disadvantaged economic group. These barriers include poor physical health of the women and their children, low educational attainment and lack of literacy, and inadequate transportation. As others have shown, the accumulation of multiple barriers creates growing interference with work efforts (
17 ). Some of these additional barriers, such as impaired health (
39 ), low educational attainment, early pregnancy, and reduced marital stability, are also correlates of social anxiety (
8 ). Although these additional barriers should be directly targeted by policy and practice intervention, they may also be reduced by efforts to treat social anxiety disorder.
This study presents certain limitations. The CIDI-SF does not contain all the clinical significance probes of the longer form and may have a lower threshold for diagnosis. If we are counting subthreshold cases, however, this would make the magnitude of impact on functioning that we detected even more impressive. Furthermore, the operating characteristics of the CIDI-SF relative to the full CIDI are well described (
25 ), and the reliability and validity of the full CIDI for phobic disorders are well documented (
40 ). Also, the social anxiety disorder prevalence rates in our sample were not unduly high and are consistent with rates in other samples—for example, primary care (
10 ). Because our sample consisted exclusively of women, we do not know whether our findings are relevant to low-income men, who are generally denied public welfare benefits in the United States.
Conclusions
As long as social anxiety disorder remains a significant, unrecognized impediment to successful employment, it will undermine efforts to reduce welfare costs through return-to-work programs, and persons with this disorder will be deprived of access to economic self-sufficiency. Systematic return-to-work programs can be successful in enhancing work attainment (
41 ), but socially anxious individuals will have difficulty utilizing such programs, because they may avoid contact altogether or perform poorly when they do have job interviews. Because of the chronicity of social anxiety disorder and the low rates of treatment seeking in our study and others (
12 ), the disorder's impact is likely be compounded over time. Social anxiety disorder is a potentially modifiable barrier to employment (
34,
35 ), and its effective management could increase workforce participation among low-income women who receive welfare benefits. We have recently obtained funding to test this hypothesis. For success with this population, it is likely that treatment adaptations and local delivery will be necessary. Development and dissemination of effective approaches could greatly improve the quality of life for these disadvantaged women, as well as provide significant public health and economic benefits.
Acknowledgments and disclosures
Funding for the Women's Employment Survey was provided by the Charles Stewart Mott Foundation, the Joyce Foundation, and the John D. and Catherine T. MacArthur Foundation and by grant R24-MH51363 from the National Institute of Mental Health.
The authors report no competing interests.