Inclusion criteria
Clients who were 18 to 50 years of age, who spoke English or Spanish, who had public insurance (Medi-Cal, Medicare, or both) (
15 ) or no health insurance, who were not HIV positive, who had verifiable contact information to assist with follow-up, and who were able to provide informed consent were eligible to participate. Clients with private insurance were excluded because of their greater access to care than those without. Documented HIV-positive clients were not enrolled in the study because they had access to specialized services. Clients who could not provide at least one verifiable contact for follow-up and those planning to leave San Francisco within the year were also excluded because of the anticipated loss of follow-up information. Intake interviews, including a comprehensive diagnostic assessment, were conducted within 72 hours of admission.
A total of 1,484 clients were identified as new entrants and potentially eligible for the study. Of this group, 537 (36%) were found to be ineligible, 377 (25%) refused participation, and 570 (38%) provided informed consent. Of those providing informed consent, 476 participants (84% of 570) completed the intake assessment battery and 420 (74%) provided useable diagnostic data. Of these 420, a total of 226 participants had co-occurring diagnoses, and of them, 224 had utilization data from the billing-information systems. The 224 composed the study sample: 118 participants from substance abuse and 106 from mental health settings. A total of 54 clients who did not provide usable data consisted of 21 persons who had no diagnoses assigned because of incomplete diagnostic data and 33 persons whose diagnoses were deemed unreliable because they did not endorse symptoms consistent with their treatment setting (for example, clients from the detoxification programs who did not endorse substance use). The excluded group of 54 persons did not differ from the included group in terms of age, gender, ethnicity, or education.
Measures and data collection
Demographic data. Demographic data were collected directly from participants during the study intake interview and consisted of age, gender, race and ethnicity, and homelessness in the 30 days before treatment entry.
Clinical data. Diagnostic data were obtained during the study intake interview by research assistants who were trained to administer the Diagnostic Interview Schedule for DSM-IV (DIS-IV) (
16 ) by a senior clinician who was trained on the instrument. With this measure, current 12-month psychiatric and substance use diagnoses were identified. For all disorders assessed, the DIS-IV includes questions about whether symptoms occurred only when the individual was under the influence of alcohol, illicit drugs, or prescription medications or were the result of a medical condition. For schizophrenia spectrum disorders, individuals were asked whether each endorsed type of delusion or hallucination was experienced only while under the influence of substances.
Current psychiatric diagnoses were grouped into four binary (yes-no) variables: schizophrenia spectrum disorders (schizophrenia, schizoaffective, and schizophreniform disorders), bipolar disorders (bipolar I and II), depressive disorders (major depression and dysthymia), and anxiety disorders (specific phobia and social phobia and panic, generalized anxiety, obsessive-compulsive, and posttraumatic stress disorders). These categories were not mutually exclusive; participants with more than one diagnosis were counted in each diagnostic category. Current substance use disorders comprised five binary variables and included use of alcohol, cocaine, amphetamines, opiates, and marijuana. Abuse and dependence diagnoses were collapsed into a single category because of paucity of participants meeting only abuse diagnoses. Co-occurring disorders were defined as having both a current mental disorder and a current substance use disorder.
Indicators of problem severity were collected during the intake interview. For analytic purposes, we operationalized psychiatric problem severity as "ever" being hospitalized for psychiatric problems, and we operationalized drug use severity as the number of current substance use diagnoses.
Utilization data. Electronic utilization data were obtained from the billing-information systems of the county mental health and substance abuse treatment systems. All county-run or county-contracted services report into these billing-information systems. Utilization data for the 24-month periods before and after study entry were downloaded, verified, and coded in consultation with county data system managers.
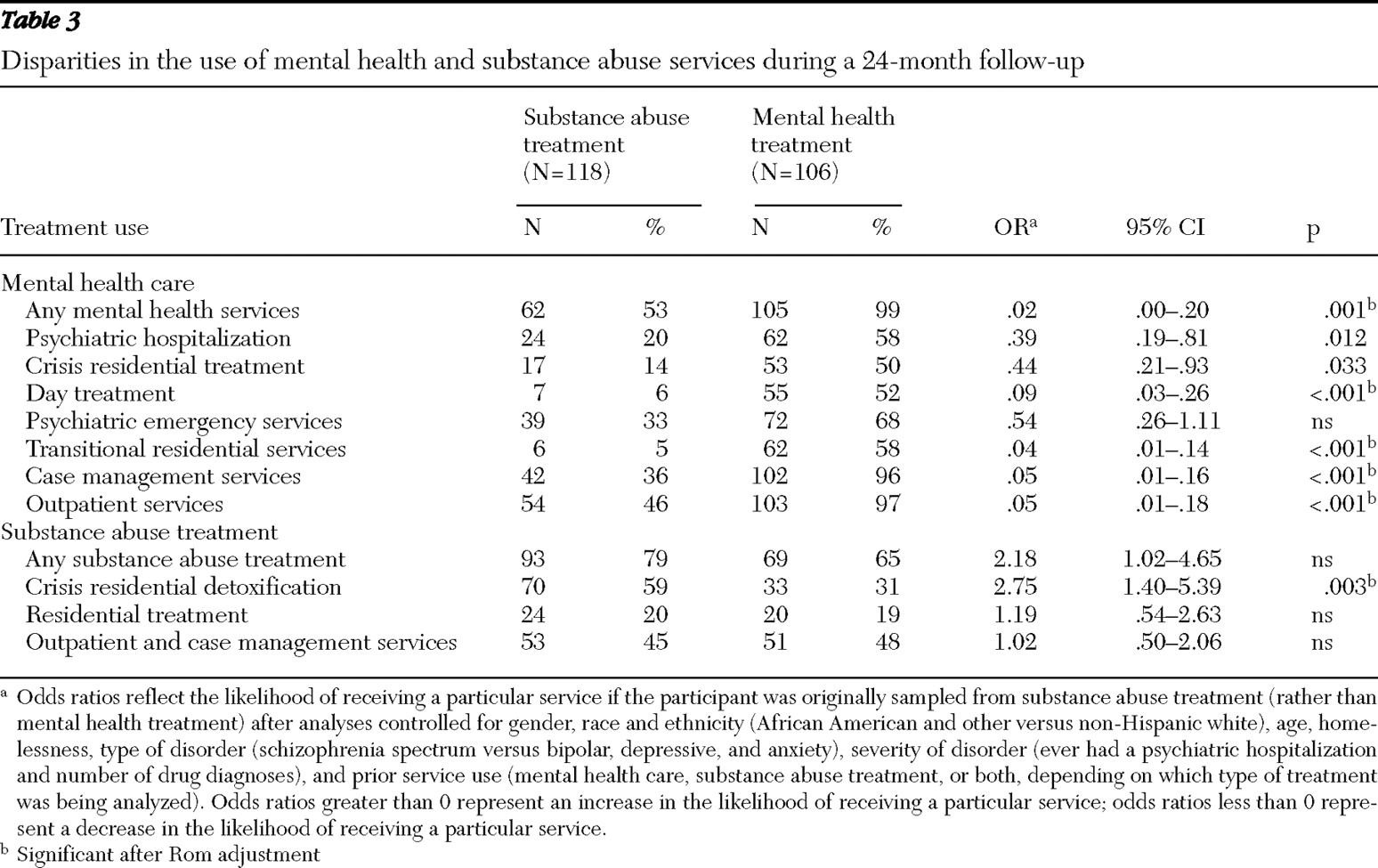
Two aggregate binary utilization variables were constructed: use of any mental health services and use of any substance abuse treatment services in the 24 months after treatment entry. Frequently used treatment services (subscribed to by 10% or more of the participants) were examined individually and transformed into binary variables as well. These included acute psychiatric hospitalization, mental health crisis residential treatment, mental health day treatment, psychiatric emergency services, mental health transitional residential services, mental health case management and (other) mental health outpatient services, crisis residential detoxification, residential drug-free treatment, and non-methadone-related outpatient services.
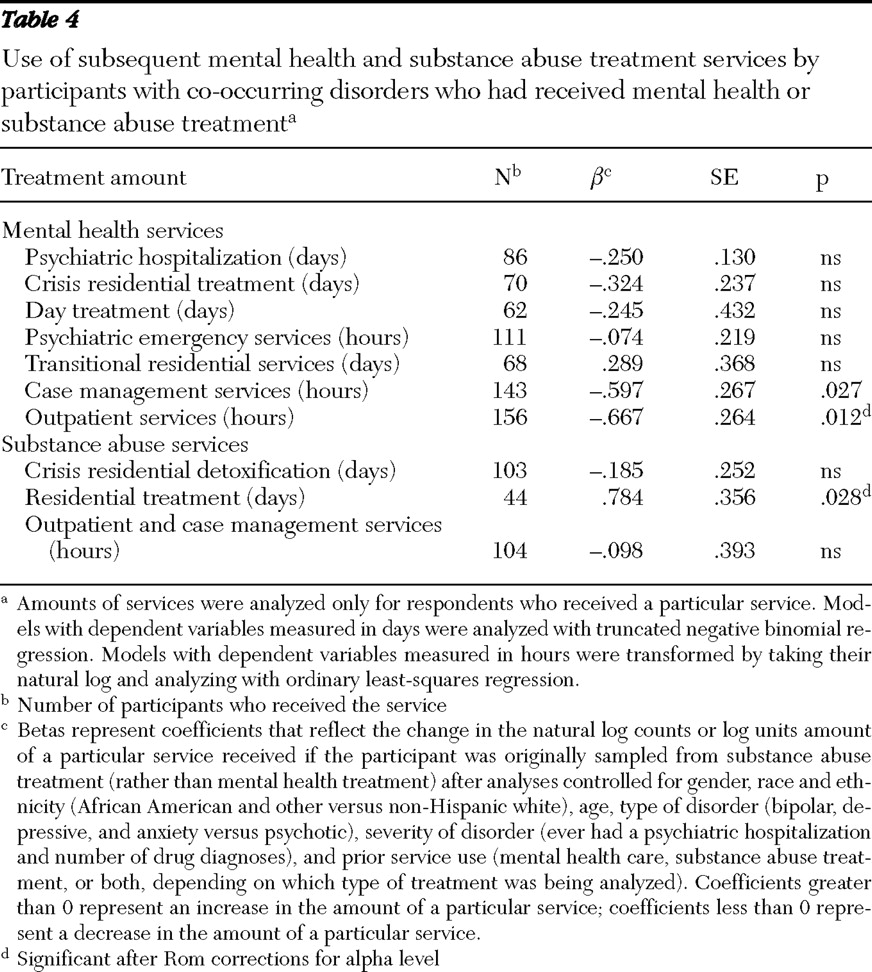
Continuous and count variables were created to reflect amount of services received over the 24 months. Amount of services was recorded as days or hours, depending on the units reported to the billing-information system.
Data analyses
Covariates. Variables included as covariates for the logistic and linear regressions were ones that either had significantly differentiated between the two treatment groups or that were supported in the literature. Covariates included gender (
17,
18 ), age (
3,
17 ), race-ethnicity (
19 ), homelessness (
20,
21 ), a diagnosis of schizophrenia spectrum disorders versus all other disorders (
22 ), severity of disorders, and prior service use (mental health treatment, substance abuse treatment, or both) (
12 ). In analyses predicting mental health service use, any use of mental health services in the 24 months before study entry was included in the model; in analyses predicting substance abuse treatment use, any substance abuse treatment in the 24 months before study entry was included in the model.
Analyses. We implemented a two-part model (
23,
24,
25 ), first using simultaneous logistic regressions to determine whether treatment system (mental health or substance abuse treatment) was a significant predictor of utilization. We then conducted zero-truncated negative binomial regressions (
26 ) to determine whether treatment system was a significant predictor of amounts of services received that were measured in number of days (counts). For amounts of services measured in hours, we used ordinary least-squares regression, but because the distribution of these variables was highly skewed, we transformed the variables into their natural log. All tests of statistical significance were two-tailed. When appropriate, we applied Rom (
27 ) corrections (a modified Bonferroni adjustment found in the literature) to all tests of significance to preserve the alpha level in multiple tests. The Rom adjustment controls the familywise error rate at the alpha designated as the significance level.