Localized delivery of mental health services, a process we term "regionalization," has been the linchpin of public mental health policy and service delivery for more than four decades (
1 ). A catchment area or regional model arguably enhances sensitivity to local population needs and encourages autonomy and flexibility in addressing them (
2,
3,
4 ). In this brief report we present a case study of the effects of a state mental health agency's regionalization of a previously centralized mental health service that manages the community reentry of persons with severe mental illness exiting correctional settings.
A recent study by the Urban Institute documented the daunting task of reentering one's community after incarceration (
5 ), a challenge made all the more difficult for persons with serious mental illnesses who must be connected (or in some cases reconnected) with mental health services and helped in regaining entitlements, including Medicaid (
6,
7,
8 ). In 1998 the Massachusetts' Department of Mental Health acknowledged and addressed these challenges through the development of a reentry program, the forensic transition team, whose mission is to address the needs of offenders with major mental illness leaving correctional settings (
9 ). The forensic transition team's only criterion for receiving transition services is that individuals meet criteria for major mental illness. An inmate's criminal history does not disqualify him or her from participating in the program. The forensic transition team provides comprehensive transition planning services to individuals while they are incarcerated by identifying service needs and starting the process of reinstating benefits three months before release. The team continues to support and monitor individuals three months postrelease, paying particular attention to living arrangements, medication compliance, case management and psychiatric appointments, and making referrals to appropriate treatment and services when warranted, such as outpatient, vocational therapy, substance abuse, and sex offender treatment and services. From 1998 to 2002 policies and practices related to transitional services were overseen by the Department of Mental Health's Central Office. As such, forensic transition team personnel and resources were mobilized from the Central Office to correctional settings statewide and made arrangements for community placement and management in concert with local personnel in the region where the client was to reside.
In December 2002 the forensic transition team was regionalized. Forensic transition team staff who had worked as a team overseen by the Central Office were reassigned to the six Department of Mental Health service regions across the state. The goal of this reorganization was to improve coordination of forensic transition team services within regional mental health systems. Specific objectives included increasing each region's capacity to serve forensic clients, reducing duplication of effort, and improving communication among community providers and the criminal justice system. Essentially, regionalization shifted supervision and control of the reentry program's functions to the six regional forensic directors who report to area directors overseeing their regions' services. Thus, under the newly regionalized system, forensic transition team members worked alongside other area personnel who had responsibility for their areas' nonforensic mental health services, including case management, residential programming, and employment services.
To assess the effects of regionalization on reentry services we compared system-level outcomes observed before and after regionalization to address questions and expectations regarding the systemic outcomes of the regionalization process. Our basic question was, How did regionalization affect the distribution of key outcomes? Our expectations were that regionalization's effects on these outcomes would be positive, because forensic transition team personnel would likely develop better linkages with area and regional personnel and have greater familiarity with local services and resources.
Methods
Correctional inmates are eligible for Massachusetts Department of Mental Health's forensic transition team services if the acuity of their axis I major mental illness has resulted in significant functional impairment lasting a year or more. During the study period (1998–2006) there were 799 unduplicated clientele. Of these 799 persons, nearly three-quarters (N=591, 74%) received previous community mental health services, primarily for thought disorders (N=413, 53%); in addition, 40% (N=312) received previous treatment for mood disorders. A small proportion (N=47, 6%) were diagnosed as having personality disorders. The vast majority (N=623, 78%) were male and aged 25 years or older (N=701, 88%). More than half (N=405, 51%) self-described as Caucasian, 20% (N=156) as black, and 15% (N=117) as Hispanic. Nearly two-thirds (N=506, 63%) had a history of co-occurring substance abuse, and 27% (N=216) had a history of homelessness. These individuals were released after serving sentences on charges that included assault and battery (N=288, 36%), public order offenses (N=224, 28%), property offenses or arson (N=136, 17%), drug offenses (N=79, 10%), sexual assaults (N=64, 8%), and murder (N=8, 1%). Eighteen percent (N=144) violated conditions of parole or probation.
Massachusetts' forensic transition team measures specific outcomes to assess performance. These are measured at follow-ups conducted with all forensic transition team clients at three months postrelease from a correctional setting. For this analysis we used four outcome categories: "engaged," meaning that the client's whereabouts are known, that he or she has not been reincarcerated or rehospitalized, and that he or she continues to receive services in the community; "hospitalized" refers to persons admitted to a psychiatric facility within three months of release; "criminal justice system" refers to persons coming back into contact with the criminal justice system either through rearrest or reincarceration; and "lost to follow-up" is recorded for persons having no contact with the mental health system—they are not known to have been hospitalized or rearrested during the period or to have been included in any state criminal justice or Department of Mental Health services roll.
Of these, engaged might be considered the optimal outcome for clients. At a minimum, this status indicates that clients attended their intake appointment in the community at time of release and stayed in contact with community case management three months after release. More than two-thirds of engaged clients had their entitlements in place and were engaged in services including, but not limited to, outpatient or day treatment, psychiatric services, and substance abuse treatment.
In Massachusetts, county houses of correction hold those with adjudicated misdemeanors and serving sentences of 2.5 years or less. County houses are distinct from jails, which are described by the U.S. Department of Justice as locally administered facilities that hold pretrial persons awaiting trial as well as persons serving sentences of one year or less. The analysis in this study focused on adjudicated individuals who had been convicted, found guilty, sentenced, and incarcerated; these persons are somewhat different from individuals emerging from the jail milieu who are held for a shorter period for a variety of reasons (
10 ).
Forensic transition team administrative data were used to assess the impact of regionalization on reentry outcomes. Data were obtained on 957 client episodes. In more than half of these episodes (N=528, 55%) individuals had served county house of correction sentences of 2.5 years or less for misdemeanor offenses. The remaining 429 episodes (45%) involved persons released from state prisons, who served an average of seven years for felony charges.
A number of individuals in the data set had more than one forensic transition team exposure (N=178) and were represented in our outcome data each time. Thus the outcome data presented here pertain to episodes of forensic transition team service, not to individuals. From July 1998 to November 2002 (the preregionalization period) the reentry program managed 525 episodes; during postregionalization (December 2002 to December 2006), the program managed 432.
This study was approved by the University of Massachusetts Boston Institutional Review Board and by the Massachusetts Department of Mental Health's Central Office Research Review Committee.
Results
During the entire period of the forensic transition team's operation, cases from county houses of correction showed higher rates of engagement than those from state prisons (54% versus 37%) but also higher rates of loss to follow-up (19% versus 8%). The overall rates of rearrest or reincarceration in the criminal justice system were roughly equal (17% from houses of correction and 15% from prisons). Former prison (but not house of correction) inmates had higher rates of hospitalization within three months of release (41% versus 10%), perhaps reflecting the seriousness of their offenses or a heightened concern about their returning to the community.
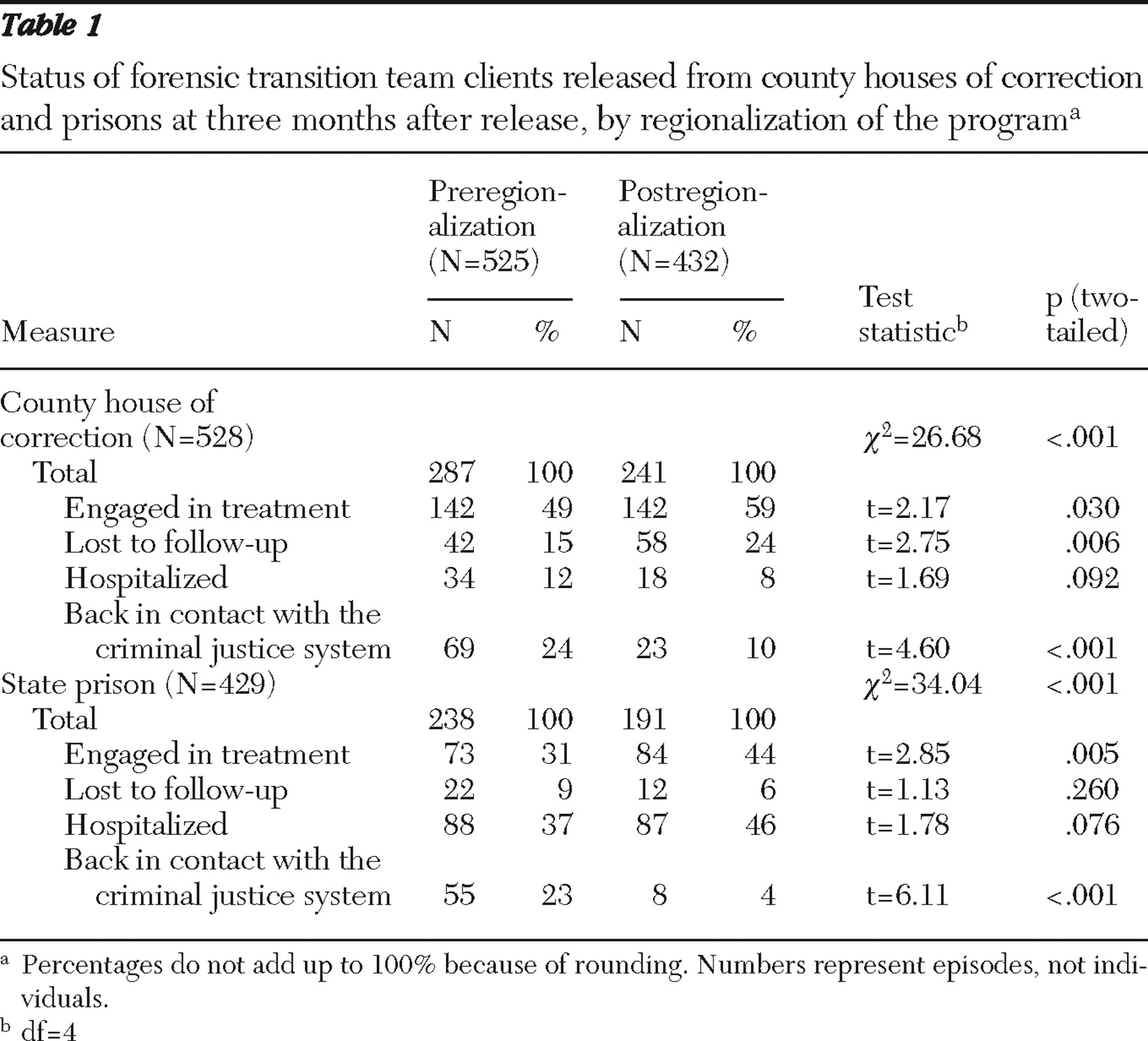
Table 1 shows differences in outcomes pre- and postregionalization. We conducted a pairwise t test of percentages in each category of the outcome variable pre- and postregionalization.
Table 1 shows significant differences before and after regionalization across outcome categories by correctional setting (that is, county house of correction or prison).
After regionalization, forensic transition team episodes involving persons exiting county houses of correction showed a significant increase in engagement, from 49% (N=142) to 59% (N=142). The teams also had a strong positive effect on episodes involving individuals released from prison, whose three-month engagement rates increased by almost 15% (31% to 44%). Another important finding is that regionalization significantly reduced the percentages of individuals returning to the criminal justice system from county houses of correction (24% to 10%) and prison (23% to 4%). The rate of loss to follow-up significantly increased among former house of correction inmates (15% to 24%), but it declined among former state prisoners (9% to 6%), although this finding was not significant. The t test results in
Table 1 confirm the trend that individuals released from county houses of corrections and prisons had consistently different outcomes both pre- and postregionalization at a high level of significance. However, this trend cannot account for the changes in outcomes in the various categories described above because this analysis does not include comparison groups or statistical controls. The individual-level and systemic factors underlying these findings also require much additional scrutiny.
We also used the same outcome variables as the dependent variable while controlling for offenders' demographic background, offense, and type of correctional institution in a logistic regression analysis. The results from the logistic regression indicate that regionalization had a significant impact on different outcomes when the above-mentioned variables were controlled for. Our multivariate analysis is consistent with these findings. However, because of the limited space, we did not include the multivariate analysis in the brief report.
Discussion
The notion that service delivery is made more effective and efficient when regionalized appears partially supported with respect to this relatively new and highly critical service. In a regionalized strategy, more attention can be given to service connections and the population being served at the local level, and there is a greater level of regional familiarity, local access, and clear lines of professional accountability and authority for service providers within each area. Regionalizing services also appears to have increased the forensic transition team's capability and expertise in serving both persons exiting local houses of correction and, importantly, those being released from state prisons. The latter have served much longer sentences, enabling better prerelease planning and potentially improving engagement at least in the short term. In addition, identification of individuals who reach a threshold level of acuity in illness that makes them appropriate candidates for step-down from the criminal justice system to scarce hospital beds immediately at release can more easily be identified. At the same time, their criminal histories are typically more serious, and their long stint away from community life may result in reentry challenges greater than those experienced by persons completing short sentences in county houses of correction.
Regionalization thus appears to have been at least somewhat beneficial. However, the increase in episodes of loss to follow-up at three months for the county house of corrections population suggests that, despite regionalization, many individuals remain difficult to keep track of, even in local environments familiar to service providers. A possible explanation is that, in contrast to the prison population, persons being released from houses of correction are typically completing much shorter sentences (on average approximately nine months), which in some cases can be terminated abruptly to reduce the inmate census or for other reasons. When these abrupt releases occur, prerelease planning can be truncated, making postrelease engagement more challenging. Additionally, individuals being released from houses of correction generally have a "lower profile" and are less of a concern to their communities than the sometimes higher-profile felons being released from state prisons, who may be described as dangerous and demand a greater share of resources and follow-up postrelease.
The data we report here must be viewed as preliminary and have several important limitations. First, although the team's staffing levels remained comparable pre- and postregionalization, factors external to the program, including changes in availability of services and even community receptivity to ex-offenders with mental illness, may have progressed independent of the administrative change. In addition, general secular trends in reentry outcomes, although not apparent in our data, could be partly responsible for the results we observed. A much broader analysis focusing on prerelease activities in prisons and county houses of correction, year-by-year data trend analysis, and assessment of each region's operating context and practices could help in determining whether there are alternative explanations for the outcome changes observed.
This analysis suggests that, as has been the case with other mental health service modalities, planning and delivering services in the area where persons will actually receive them may improve efficiency and outcomes, even for the challenging population of individuals with mental illness exiting correctional settings.
Conclusions
Although regionalization is a positive step toward improved transition planning, our findings reveal that gains in some areas also result in losses in others. For example, overall increases in engagement and decreases in contact with the criminal justice system for individuals released from houses of correction and prisons are offset by increased rates of losses to follow-up for individuals exiting houses of correction. Thus, although transition and reentry planning may improve in a regional model, the practice is distinct based on correctional setting, prerelease planning time, and severity of offender profiles. Reentry planning for ex-inmates released from houses of corrections poses special challenges, particularly given their comparatively elevated rates of return to the criminal justice system postrelease.
Acknowledgments and disclosures
The authors report no competing interests.