Measures
The analyses presented here are based on the following sections of the interview schedule.
Diagnostic assessment. The diagnostic instrument used in the WHO-WMH was the Composite International Diagnostic Interview (CIDI) (
18 ), a fully structured diagnostic instrument that assesses lifetime and recent prevalence of selected psychiatric disorders according to both
ICD-10 and
DSM-IV diagnoses. The Israel survey assessed for anxiety disorders (panic disorder, generalized anxiety disorder, agoraphobia without panic disorder, and posttraumatic stress disorder), mood disorders (major depressive disorder, dysthymia, and bipolar I and II disorders), and substance use disorders. The presence of a disorder was determined by whether respondents' past or current symptoms met 12-month or lifetime diagnostic criteria for a
DSM-IV disorder. For each disorder, a screening section was administered to the respondent. When a respondent endorsed a specific screening item, he or she was asked all the questions in the CIDI diagnostic section for that disorder to establish the presence of a current disorder. Persons who reported the presence of an organic disorder that accounted for their symptoms were not included in the sample.
The validity of the WHO-WMH CIDI as a diagnostic tool was assessed in France, Italy, Spain, and the United States by a clinical reappraisal study (
20 ). That study sought to determine whether CIDI diagnoses were consistent with those obtained independently by trained clinicians who administered the Structured Clinical Interview for DSM-IV (SCID) to a subsample of survey respondents who had previously completed the CIDI. The individual-level concordance between the SCID and CIDI for 12-month prevalence of any mood disorder, any anxiety disorder, and any disorder overall was substantial (area under the curve in the range of .8 to .9) (
20 ).
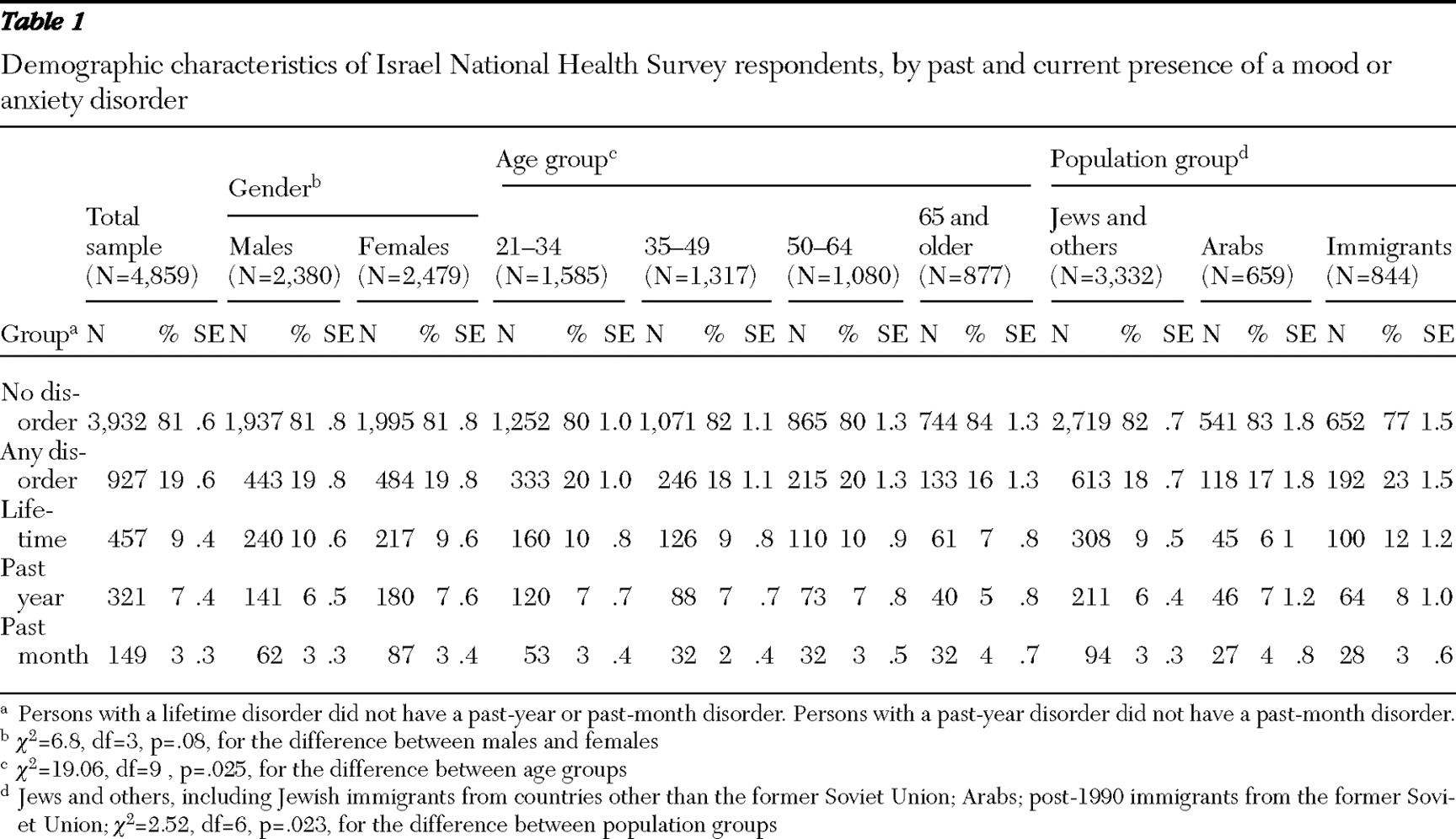
For the analyses reported here, respondents were grouped into those with or without any mood or anxiety disorder, because one-third of those with any anxiety disorder also had a mood disorder. All respondents with a 12-month alcohol or drug use disorder had a comorbid anxiety or mood disorder and were therefore included in the anxiety or mood disorder group. The analysis distinguished between four groups of respondents in terms of a mood or anxiety disorder: those with no disorder, those with a lifetime disorder but no disorder in the past 12 months, those with a 12-month disorder but no disorder in the past 30 days, and those with a disorder in the past 30 days.
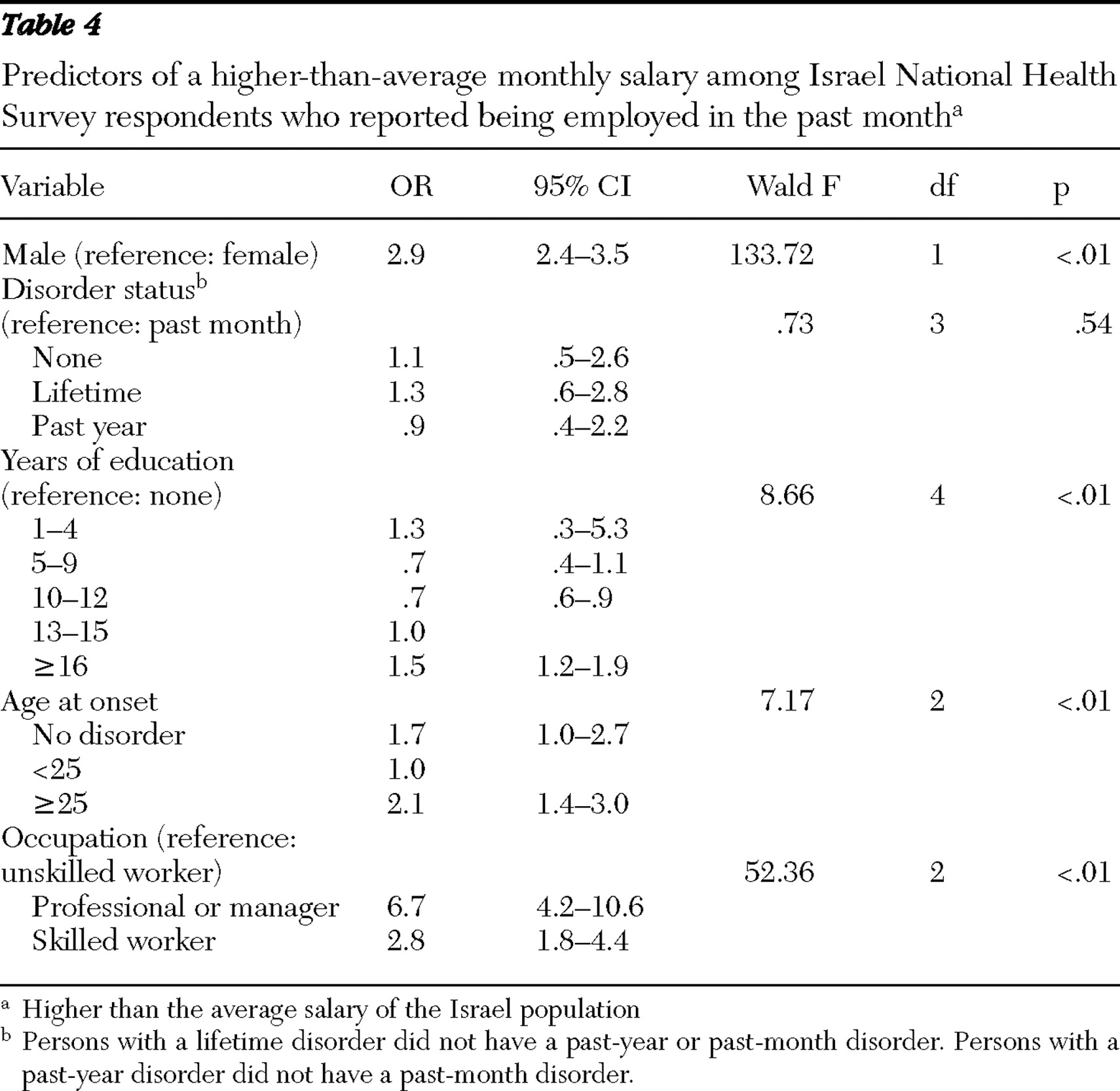
Age at onset. The survey included an item on age at onset: "How old were you the first time you had the symptoms?" Respondents who could not remember were asked whether onset was before they started school, before their teens, or later. Age at onset, a continuous variable, was divided into two categories of equal size: aged 24 and younger and aged 25 and older. The multivariate analysis used three categories: no age at onset (no disorder), onset at 24 or younger, and onset at 25 or older.
Chronic general medical conditions. The survey included a checklist of chronic general medical disorders and chronic pain. The conditions listed were heart attack, heart disease, stroke, high blood pressure, asthma, chronic obstructive pulmonary disorder, emphysema or other lung disease, tuberculosis, diabetes, kidney disease, neurological conditions, thyroid disease, cancer, chronic back or neck pain, arthritis or rheumatism, headaches, or any other chronic pain. Respondents were asked whether they ever experienced any of the symptoms of these conditions and, if so, whether they experienced them at any time in the past 12 months. For conditions that are typically identified by medical diagnosis, such as heart disease, respondents were asked whether a doctor or other health professional had ever told them that they had the condition, and if so, whether they had the condition in the past 12 months. The question about the past 12 months was omitted for conditions that persist throughout the life course. In this analysis, respondents with chronic general medical conditions were grouped into a two categories: those reporting any one of the conditions and those reporting none.
Methodological research has shown that such checklists provide useful information about treated or currently untreated chronic conditions (
21 ) and that they predict use of outpatient health care, hospitalization, and mortality (
22 ). Such research has also shown that self-report of chronic general medical conditions is in moderate to high agreement with medical records data (
23 ).
Service use for emotional or mental problems. Respondents were asked whether they had ever visited any of a list of professionals to talk about problems related to their mental or emotional health. The professionals listed were specialist mental health service providers (such as psychologists, psychiatrists, and social workers), general medical professionals (such as general practitioners), religious counselors (such as rabbis and sheikhs), and healers (such as naturopaths).
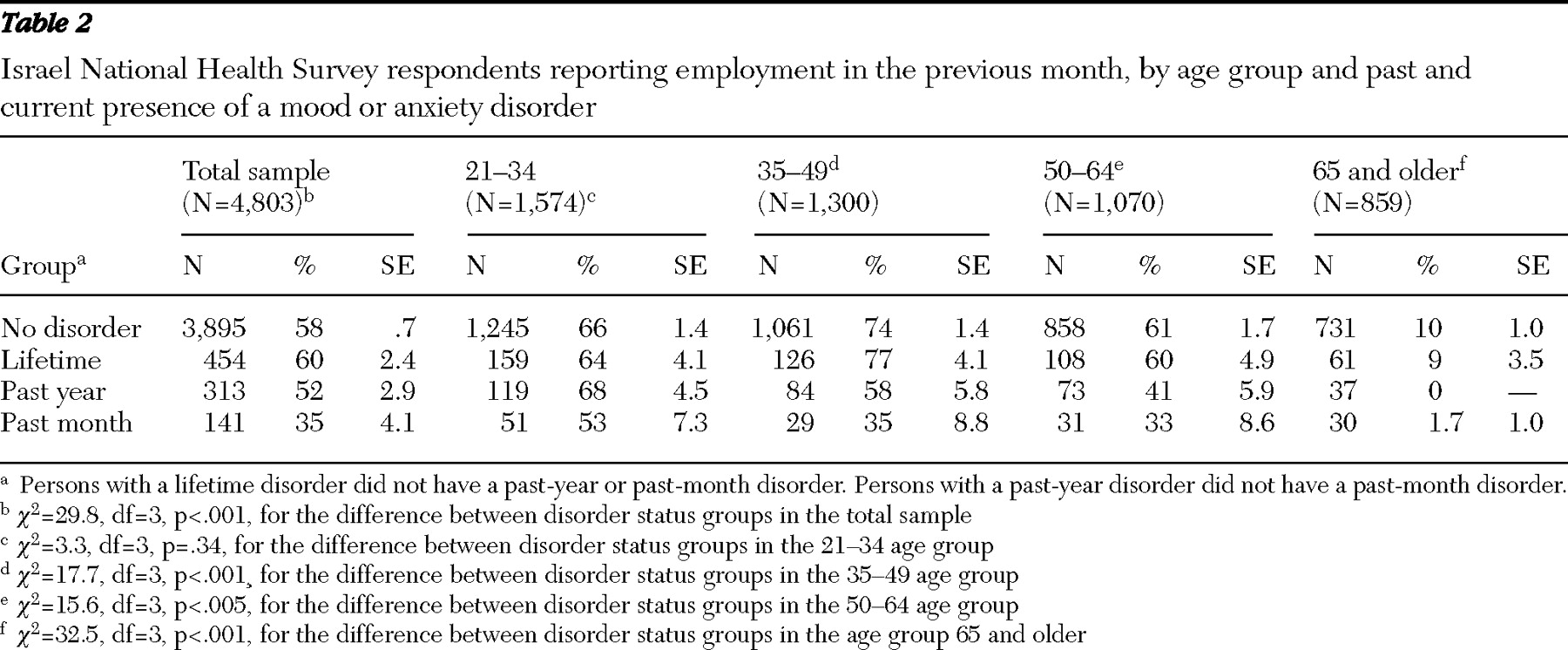
Employment, monthly salary, and occupation. All survey respondents were asked to report their salary in the previous month. For the study reported here, respondents' reports of employment and income for the previous month were used. Income was then categorized into two groups: above and below the average monthly salary in Israel (about $1,500 U.S. dollars at the time of the study).
All respondents were asked to describe the type of work they did in their place of work. The answers were classified by Central Bureau of Statistics staff into ten occupational groups on the basis of the International Labour Organization's Classification of Occupations (
24 ). For this study the ten classes of occupations were categorized into three groups: professionals and managers, skilled workers, and unskilled workers.
Employment restrictions. All respondents were asked about whether they had physical or emotional problems that placed limits on employment and whether they were out of the workforce, temporarily unemployed, or employed full-time. The following three questions were used in this study: "Are you limited in the kind or amount of work you can do because of problems with your physical or emotional health?" "What is the main reason you are not working and also not looking for a job?" "Do you have any problems with your physical or emotional health that would prevent you from working for pay if you wanted to?" Four mutually exclusive categories were used for restriction: due to general medical problems, due to mental health problems, due to both general medical and mental health problems, and no health restrictions on employment. Respondents who stated that they did not work or were not looking for work because they had retired or were homemakers or who stated a reason other than health were classified as having no health restrictions on employment.
Statistical analysis
The data were weighted to adjust for the differential probabilities of respondents' selection and nonresponse and for differences between the sample and the adult population in Israel. Prevalence rates in the four disorder status groups (none, lifetime, past year, and past month) were calculated by gender, age, and the three population groups on the basis of weighted data, along with estimates of standard errors.
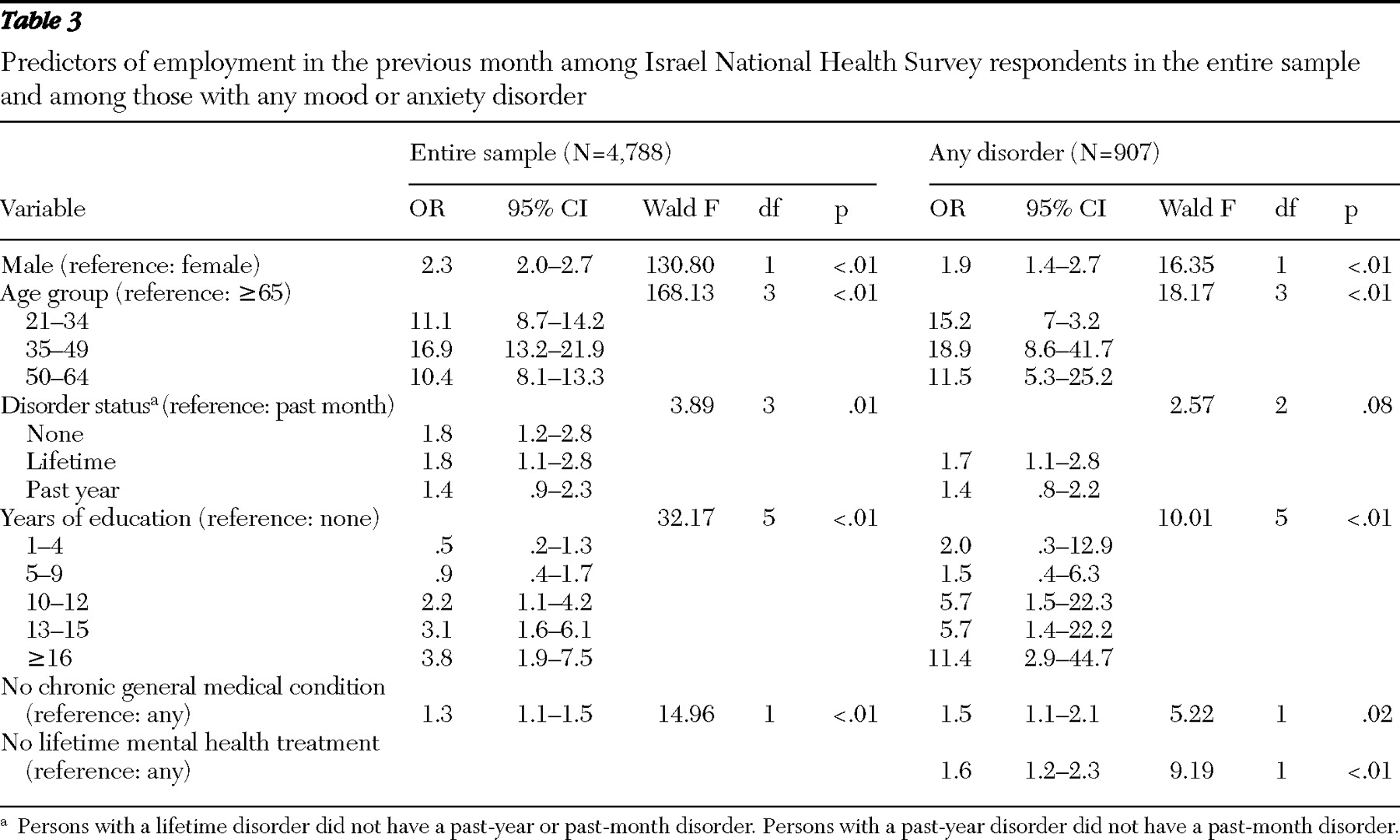
Logistic regression analyses were conducted with SUDAAN (
25 ) to estimate the association between being employed and mental disorder status in the entire sample adjusted for age, gender, and any chronic general medical condition; the association between being employed and disorder status among respondents with any mental disorder adjusted for age, gender, education, any chronic general medical condition, and any past treatment for mental problems; and the association between being in the higher-than-average salary group and disorder status among those who were working in the previous month adjusted for age, gender, education, and age at onset of mental problems.
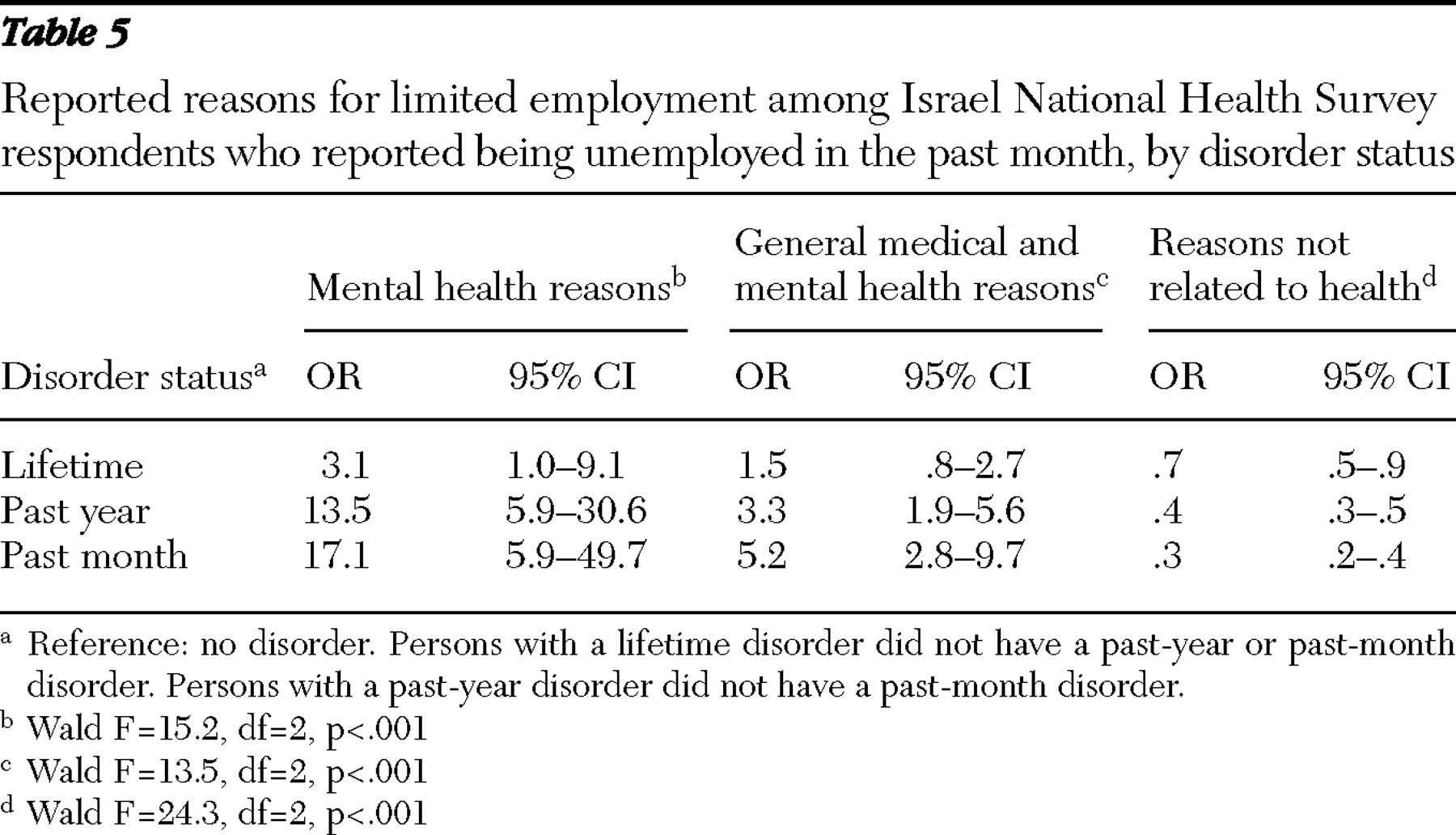
Another set of regression analyses was conducted for respondents who were unemployed or who had employment limitations in order to estimate the association between the reported reason for lack of employment and mental disorder status adjusted for age, gender, education, and any chronic general medical condition. The logistic regression coefficients were transformed to odds ratios (ORs) and 95% confidence intervals (CIs).