For most patients with schizophrenia, a combination of pharmacological and psychosocial interventions is necessary for optimal outcomes (
1 ). Cognitive-behavioral therapy has been found to be an effective adjunct to the use of antipsychotic medications (
2 ), especially for decreasing the positive symptoms of schizophrenia (
3 ). In fact, cognitive-behavioral therapy's effectiveness has led to clinical guidelines recommending it for the routine treatment of schizophrenia (
4 ). However, most of the studies about the adjunctive use of cognitive-behavioral therapy for schizophrenia have been with patients who were treated with first-generation antipsychotic medications and not with second-generation antipsychotics, which are now recommended as the first choice for the treatment of schizophrenia (
5 ). Pinto and colleagues (
6 ) treated patients with clozapine and cognitive-behavioral therapy and found that cognitive-behavioral therapy was superior to supportive therapy for the control of general psychopathology and positive symptoms. In reviewing that study, Rector and Beck (
7 ) concluded that there might be a possible synergistic interaction between clozapine and cognitive-behavioral therapy. However, clozapine is reserved for patients with treatment-resistant symptoms because of the risk of agranulocytosis (
5 ). Hence, it is important to evaluate whether adding cognitive-behavioral therapy to the treatment of patients with schizophrenia who are prescribed other second-generation antipsychotics is more effective than treating patients with only second-generation antipsychotics.
The purpose of this pilot study was to determine whether adding individual cognitive-behavioral therapy to the treatment of patients with schizophrenia who were prescribed second-generation antipsychotics other than clozapine would be more effective than treating patients with schizophrenia with only second-generation antipsychotics. Clozapine was excluded because the combination of clozapine and cognitive-behavioral therapy has been previously studied (
6 ).
Methods
Detailed descriptions about how the patients were recruited, screened with respect to exclusionary and inclusionary criteria, treated with individual cognitive-behavioral therapy, prescribed second-generation antipsychotics, and rated with or administered various instruments, as well as the a priori power analysis and the reasons for the selection of the statistical procedures that were employed, are available in an online supplement at
ps.psychiatryonline.org .
Thirty-six patients were screened after giving informed consent. Thirty-three were eligible for the study: 18 (55%) were randomly assigned to receive second-generation antipsychotics and cognitive-behavioral therapy, and 15 (45%) were randomly assigned to receive only second-generation antipsychotics. The third author (RAS) prepared a list of computer-generated random numbers for patient assignment and did not have any contact with the patients. The first author and principal investigator (NRP) reviewed all of the available medical records, administered the clinical version of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (
8 ) to derive all of the psychiatric diagnoses; all of the SCID modules were administered if necessary. The ratings for the clinical outcome scales were made at baseline (pretest), after completion of therapy at 12 weeks (posttest), and at 24 weeks (follow-up) by the second author (DJR), a psychiatrist who is also an expert in the pharmacology of schizophrenia and was blind to whether a patient was receiving cognitive-behavioral therapy. The self-report measures were also administered by the study's project coordinator or research assistant before the same visits when the clinical ratings were made. The patients received $25 at the end of completing each one of the three assessment visits. The study was conducted from September 2005 through October 2008 and was approved of by the institutional review board of the School of Osteopathic Medicine in Stratford, New Jersey.
Of the 33 patients who were randomly assigned to treatment, 25 (76%) completed baseline and posttest 12-week evaluations, and 17 (52%) completed follow-up evaluations at 24 weeks. For the 25 outpatients who completed pre- and posttest evaluations, 14 (56%) were women and 11 (44%) were men. Twenty (80%) were European Americans, one (4%) was African American, one (4%) was Hispanic American, and three (12%) persons described themselves as of "other" race or ethnicity. Thirteen (52%) had never married, and 22 (88%) were unemployed. The mean±SD age was 40±11 years. The mean number of years of hospitalization was 3±3. Twenty-two (88%) were diagnosed as having schizoaffective disorder, and three (12%) were diagnosed as having paranoid schizophrenia. The sample's initial, mean level of global functioning was 44±9. (Global functioning was measured with DSM-IV-TR Global Assessment of Functioning scale. Possible scores range from 0 to 100, with higher scores indicating better functioning.) Sixteen (64%) patients were also diagnosed as having comorbid anxiety disorder.
All of the patients received pharmacotherapy during monthly visits with the second author (DJR). Frequency of pharmacotherapy was standardized: patients were seen every four weeks or more frequently if necessary. Visits lasted 30 minutes or longer if necessary. The focus of the medication visits was on medication adherence, which was determined through means such as verbal questioning, checking prescriptions filled, and collaborating with family or case managers wherever possible. The dosages of the second-generation antipsychotics and adjunctive medications, such as anxiolytics and antidepressants, were prescribed and adjusted according to the estimation of the patient's clinical needs.
The patients in the group with cognitive-behavioral therapy received 12 weekly individual sessions of cognitive-behavioral therapy from the first author (NRP), who is certified in cognitive-behavioral therapy. The cognitive-behavioral therapy approach was not manualized, but it stressed engaging the patients in treatment; developing a cognitive formulation of the symptoms; and utilizing a normalizing rationale to reduce stigma associated with psychosis, with specific cognitive techniques to reduce distress and dysfunction associated with positive psychotic symptoms and relapse prevention techniques. Homework tasks included the completion of dysfunctional thought records, modified dysfunctional thought records for voices and delusions, activity schedules, and a range of behavioral experiments (
7 ).
The clinical rating scales that were administered were the Psychotic Symptom Rating Scales (PSYRATS) (
9 ) to evaluate the severity of delusions and hallucinations, the Hamilton Psychiatric Rating Scales for Anxiety (HARS) (
10 ) and Depression (
11 ) to assess, respectively, the severities of clinically rated anxiety and depression. In addition, the Beck Anxiety Inventory (
12 ), the Beck Depression Inventory-II (
13 ), and the Beck Cognitive Insight Scale (
14 ) were administered to measure, respectively, the severities of self-reported anxiety and depression and cognitive insight about patient's mental health problems.
Results
The 14 (56%) patients in the second-generation antipsychotics plus cognitive-behavioral therapy group and who completed posttest evaluations at 12 weeks received a mean of 11.93±.83 cognitive-behavioral therapy sessions (median=12, range=ten to 13) and a mean of 4.07±1.59 medication visits. The 11 (44%) patients in the group that received only second-generation antipsychotics and who completed posttest evaluations had a mean of 5.00±1.84 medication visits. The mean difference in medication visits between the two groups was not significant. An analysis of covariance (ANCOVA) also found that at 12 weeks the adjusted posttest, mean chlorpromazine-equivalent dosages for the second-generation antipsychotics for both groups were comparable; the posttest adjusted mean dosage for the second-generation antipsychotics plus cognitive-behavioral therapy group was 597.84 mg, and the adjusted mean dosage for the other group was 612.02 mg. The antipsychotic dosage equivalency to chlorpromazine-equivalent units was based on expert consensus guidelines for the treatment of psychotic disorders (
5 ).
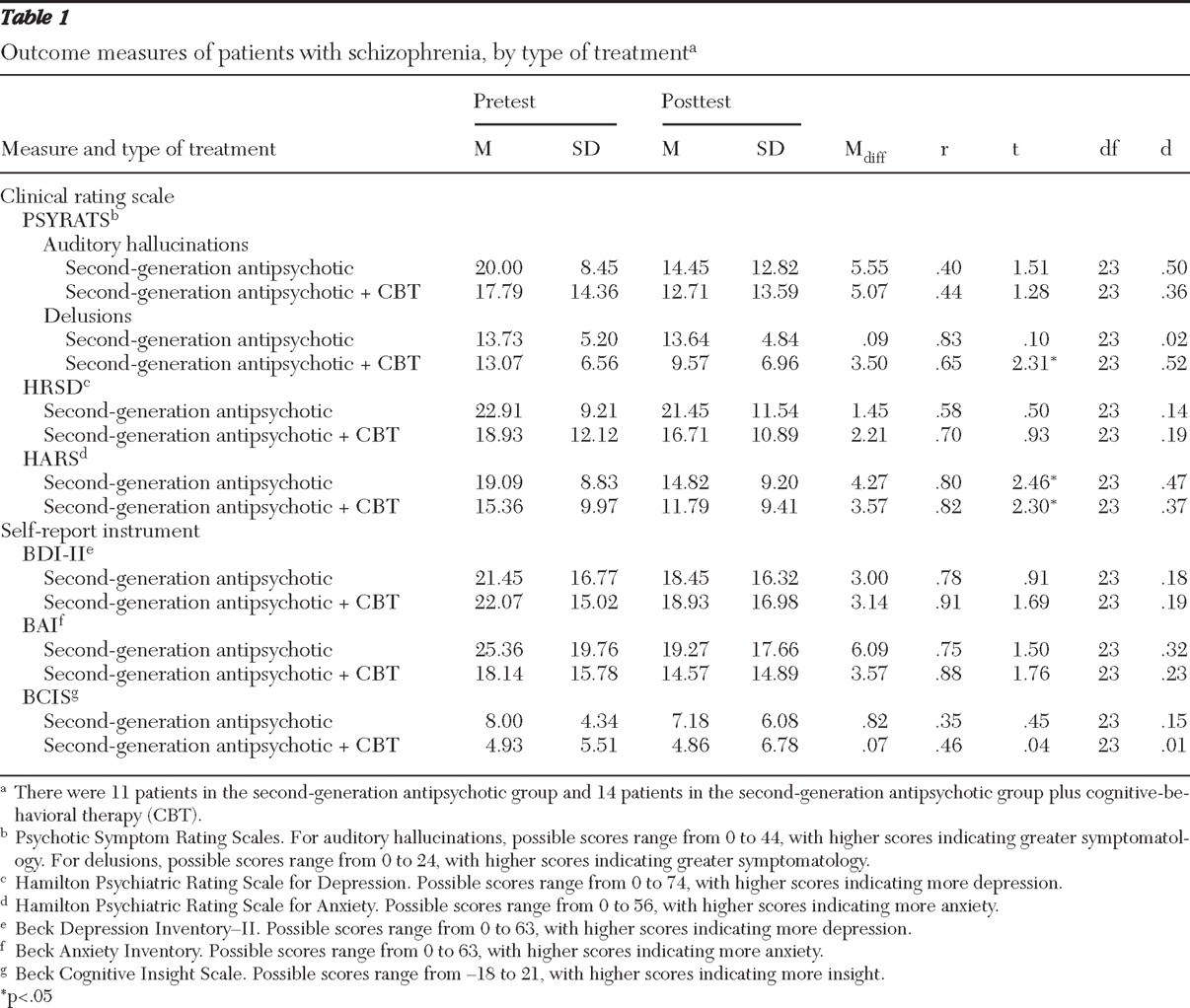
Table 1 presents the pre- and posttest means, standard deviations, correlations between the pre- and posttest scores, paired (correlated) t tests, and effect sizes (d statistics) for the mean differences between the pre- and posttest means for the outcome measures for each treatment group. Because this was a pilot study, no Bonferroni adjustment was made to control for the familywise error rate. As
Table 1 indicates, there were three significant (p<.05) pre- and posttest mean differences: the patients who were treated with second-generation antipsychotics plus cognitive-behavioral therapy were rated as having less severe delusions on the PSYRATS, and patients in both groups were rated as having less anxiety on the HARS. These three significant mean differences represented medium effect sizes according to Cohen's interpretive guidelines (
15 ). However, none of the ANCOVAs that were calculated for the seven outcome measures to compare both groups' adjusted mean differences at posttest were significant, even though the mean difference between the adjusted mean PSYRATS delusion scores represents a large effect size (d=.81).
Follow-up data at three months after treatment ended (24 weeks) were available for only 17 (68%) of the 25 patients who completed treatment (11 patients in the second-generation antipsychotics plus cognitive-behavioral therapy group and six in the second-generation antipsychotics-only group). Wilcoxon matched-pairs signed-ranks tests were used to compare the posttest scores of the seven outcome measures with the 24-week follow-up scores for each group, and there were no significant differences from the posttest scores. Of importance, the decrease in clinically rated severity of delusions was maintained at 24 weeks for the second-generation antipsychotics plus cognitive-behavioral therapy group.
Discussion
The results show that cognitive-behavioral therapy as an adjunct to pharmacotherapy with second-generation antipsychotics afforded a significant reduction in the severity of clinician-rated delusions among patients with schizophrenia, and the improvement was maintained three months after treatment ended. The improvement in delusions is consistent with results from multiple prior studies that showed improvement in positive psychotic symptoms with cognitive-behavioral therapy (
6 ). Unlike previous studies, in our study pharmacotherapy was more standardized—one psychiatrist was responsible for prescribing all of the psychotropic medications, and the duration and frequency of pharmacotherapy visits was controlled for—thereby eliminating variations in prescription practices across different psychiatrists. The improvement in delusions might be attributable to increased time in treatment as opposed to specific effects of cognitive-behavioral therapy. However, the persistence of improvement three months later makes this explanation less likely.
The study presented here did not find significant improvement in the auditory hallucinations component of the PSYRATS scale in the group that received cognitive-behavioral therapy, as has been reported in other studies (
6 ). The lack of response of auditory hallucinations could be due to the small sample size, use of only 12 sessions of cognitive-behavioral therapy, or nonstipulation in the inclusion criteria of the period of active psychotic symptoms required, unlike prior studies.
The methodological strengths of this study are use of a standardized diagnostic assessment, randomized treatment assignment, blind clinical assessments, and control for the way in which pharmacotherapy was provided. With respect to limitations, the sample was small, members of the second-generation antipsychotic-only group did not receive equivalent amounts of therapy time, and the dropout rate in the second-generation antipsychotic-only group was high. The cognitive-behavioral therapy sessions were not monitored to ensure that cognitive-behavioral therapy was being used, and the prescribing of the psychotropic medications was based on only one psychiatrist's preferences. Future studies should have larger samples, control for the total time in treatment, include fidelity measures for cognitive-behavioral therapy, and compare the second-generation antipsychotic prescribing practices of more than one psychiatrist. Inability to conduct an intent-to-treat analysis and requiring patients to change their psychiatrist reduced the generalizability of this study.
Conclusions
Cognitive-behavioral therapy was effective in reducing the severity of delusions among patients taking second-generation antipsychotics, and the improvement persisted three months after completion of therapy.
Acknowledgments and disclosures
This project was funded by a NARSAD grant to the first author (supported by Stephen and Constance Lieber). The authors thank Louis Pantuck, R.N., C.C.R.C., for help in scheduling and taking calls from patients and organizing and maintaining the records.
The authors report no competing interests.