Introduction by the column editors: Psychosocial treatment and rehabilitation can be categorized as a primarily remedial or a primarily compensatory means of targeting the functional deficits of persons with schizophrenia and other disabling mental disorders. Remedial strategies attempt to overcome functional deficits by improving the individual's skills through training interventions. Social skills training and the token economy are examples of this approach (
1,
2). Compensatory approaches aim to create environmental supports that reduce cognitive burdens, stress, and requirements for functioning while providing for the individual's needs and quality of life. Assertive case management and supported employment are examples of compensatory programs (
3,
4).
Remedial interventions focus on changing the individual, while compensatory programs aim to improve support and accommodations in the person's environment. Most psychiatric rehabilitation programs, in reality, use both remedial and compensatory interventions. This month's Rehab Rounds column describes a compensatory approach called cognitive adaptation training that uses neurocognitive assessment to direct treatment planning.
Cognitive adaptation training is a series of intervention strategies designed to compensate for the cognitive impairments associated with schizophrenia and improve adaptive functioning (
5). The determination of which strategies are required for a particular client is based on the results of a battery of neuropsychological tests (
6), an assessment of functioning, and a structured evaluation of observed behavior.
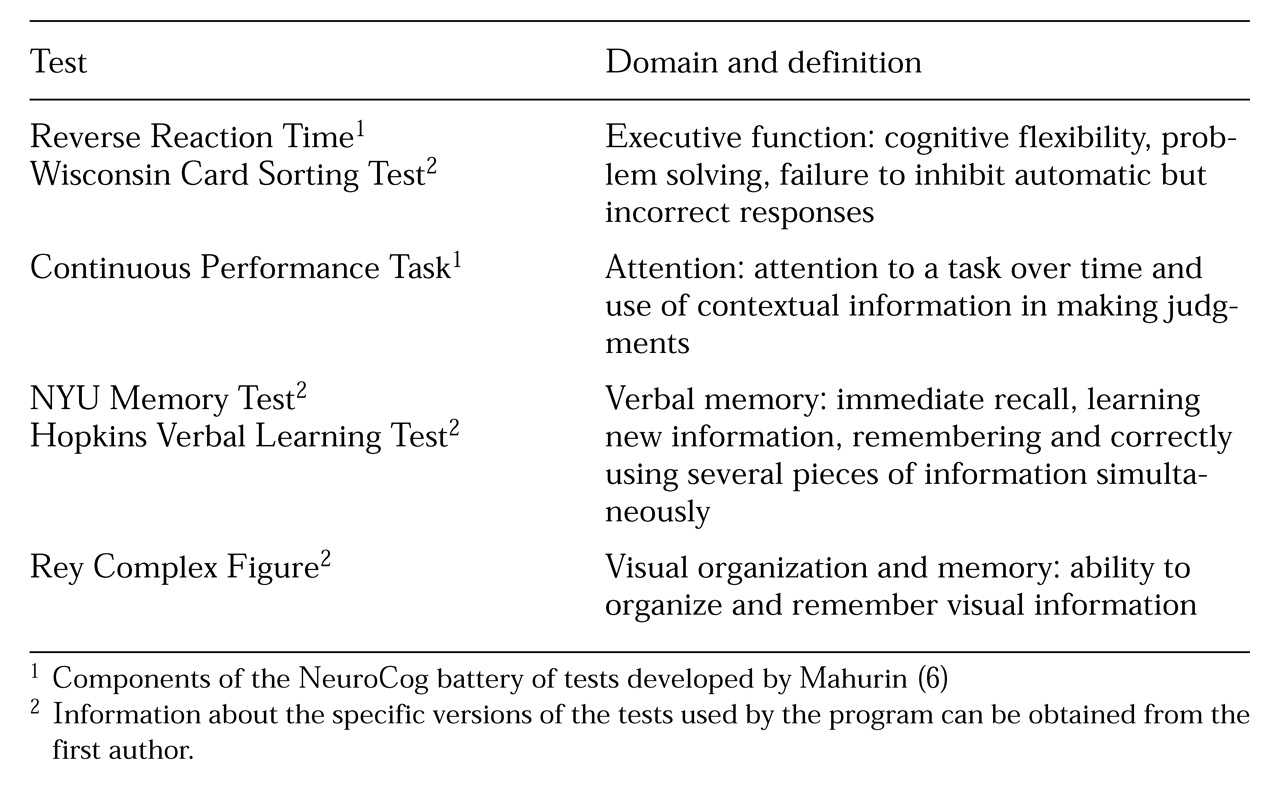
The neuropsychological tests used in the approach are described in
Table 1. They are usually administered by master's-level psychologists, and the results are given to therapists in the cognitive adaptation training program for treatment planning. Program therapists can be from any mental health discipline, including psychology, social work, occupational therapy, and nursing, and may have an educational background ranging from high school through doctoral-level professional training.
The assessment of functioning, completed by the program therapist, is based on use of the Functional Needs Assessment, a 26-item performance-based measure of the client's ability to initiate and perform basic activities of daily living (
7). This instrument covers multiple areas of adaptive functioning such as grooming, avoiding hazards, shopping, and care of belongings. Scores obtained during a structured, clinic-based assessment are supplemented with results of assessments done during home visits. Thus scores on the Functional Needs Assessment reflect actual performance in the home. For example, if a home visit reveals that a client's clothes are not clean, the scores for structured performance on items of the Functional Needs Assessment that reflect dressing and laundry skills may be amended.
During home visits, the therapist from the cognitive adaptation training program also thoroughly assesses the client's living environment to identify safety hazards such as improper storage of foods—for example, flour kept next to rat poison and inappropriate use of electrical appliances, such as using a space heater to boil water or using appliances with frayed electrical cords. In addition, the therapist checks the availability of necessary supplies, such as a toothbrush and laundry soap, and determines if they are properly placed. The therapist also characterizes the natural support systems that are available to the person, including the level of structure provided in the home, the tasks that are done for the client, and the degree to which parents or residential staff are knowledgeable about mental illness.
Finally, the therapist completes the Frontal Lobe Personality Scale (Grace J, Malloy P, unpublished manuscript, 1992) based on behavior observed before the client's discharge from the hospital and during home visits. This scale was designed to quantify behavioral syndromes that have been associated in theory with abnormalities in various frontal circuits. For example, abnormalities in the anterior cingulate cortex and lateral orbital prefrontal cortex have been associated with apathy and disinhibition, respectively.
The scale contains 46 items focused on the frequency with which clients show interest in tasks, neglect tasks, behave inappropriately or impulsively, become stuck on certain ideas, and become cognitively derailed while performing a task. Scores are converted into T-score form. Based on an algorithm of scores, individuals are classified as apathetic, disinhibited, or mixed. Roughly one-third of all outpatients we have tested fit into each of these categories.
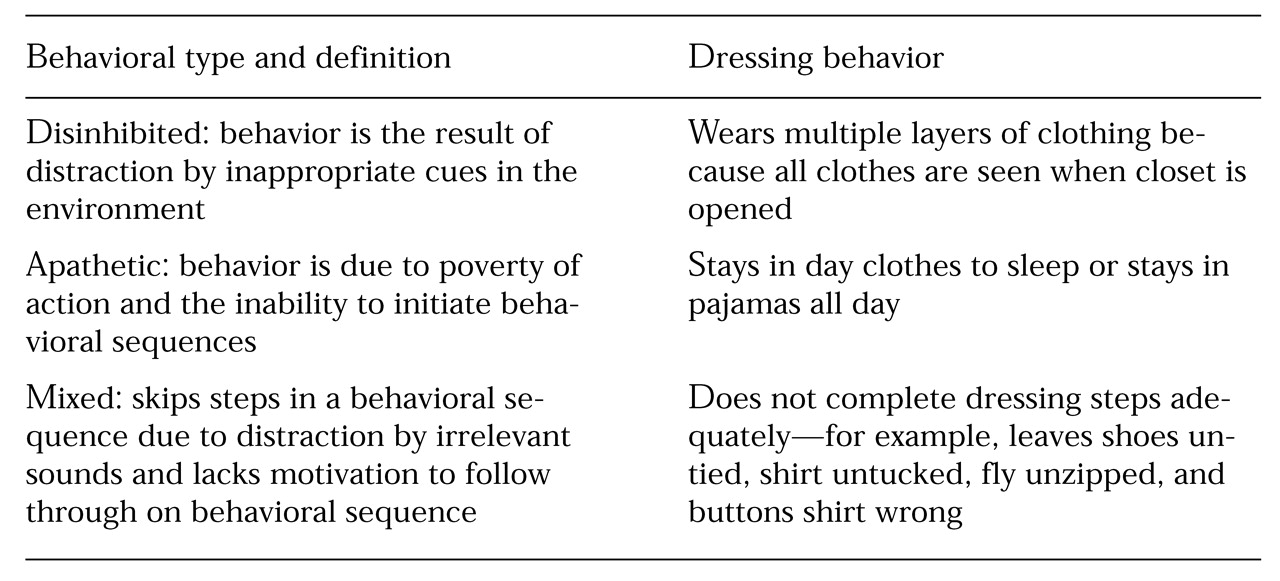
Individuals with primarily apathetic behavior tend to have poverty of speech and action and to be unable to initiate and follow through on behavioral sequences. Individuals scoring higher on disinhibition tend to be distractible, too easily driven by cues in the environment, and lacking in judgment (
8). Those with a mixed profile have a combination of these behavioral tendencies, which can be observed in many areas of instrumental behavior.
Table 2 provides an example of each these profiles related to dressing.
Although the same overt behavior, such as skipping steps in dressing, may occur due to apathy (not being able to initiate behavioral sequences) or to disinhibition (being distracted during the task), scores on the Frontal Lobe Personality Scale allow clinicians to identify the underlying styles that lead to similar overt behaviors. Moreover, the overt behaviors and symptoms of schizophrenia only partly overlap. Among participants in our program, correlations between apathy and negative symptoms range from .30 to .59 (Pearson correlation coefficient), and those between disorganization symptoms and disinhibition range from .33 to .43.
In the same way that assessments such as the Brief Psychiatric Rating Scale characterize symptoms with well-defined anchor points, the Frontal Lobe Personality Scale characterizes an individual's approach to goal-directed activity. Classifications of clients' behaviors tend to remain stable over a three- to six-month period and correlate more highly with multiple measures of community outcome than do ratings of symptoms.
Both level of impairment on measures of executive functioning and overt behavior guide the types of compensatory strategies applied in cognitive adaptation training. In general, clients with greater degrees of executive impairment need a greater level of structure and assistance and also need larger, brighter, and more proximally placed visual cues to remind them of appropriate behavior. Individuals with less impairment in executive function can perform instrumental skills adequately with less structure and more subtle cues. Often clients who show apathy need prompting and cueing to complete each step in a sequenced task. Clients with disinhibited behavior respond well to the removal of distracting stimuli and to redirection. Those with mixed profiles benefit from a combination of these approaches.
Interventions may be adapted for significant memory, attention, and fine motor impairments or strengths. For example, changing the color or placement of signs may help capture the client's attention. Similarly, substituting Velcro fasteners for buttons may compensate for a client's impairment in the fine motor coordination needed for dressing.
The following two cases differ in the client's level of executive impairment, in the types of overt behavior shown, and in the range of compensatory strategies used in the client's cognitive adaptation training. The cases were drawn from among subjects participating in research on the use of compensatory strategies at the clinical research unit of San Antonio State Hospital during 1995 to 1997. Since 1993, as part of ongoing studies, about 100 clients have participated in the cognitive adaptation training program.
Case 1
Mr. C, a 30-year-old man with an 11-year history of schizophrenia, showed evidence of apathy and moderate executive impairment. Although he was compliant with his medication regimen, he had been hospitalized three times in the preceding year. He was living independently in an apartment during the time of our evaluation. Mr. C identified his major problems as occasionally believing his thoughts were being broadcast to others, particularly when he was around strangers or on the public bus, and not knowing what to do when he was alone in his apartment.
His neuropsychological testing revealed moderate impairment in executive functions (his scores ranged from one and a half to two standard deviations from the mean of control subjects), severe attentional impairment (scores of more than two standard deviations from the mean of control subjects), and mild verbal and visual memory impairment (scores ranging from one to one and a half standard deviations from the mean of control subjects). His scores on the Frontal Lobe Personality Scale indicated apathetic behavioral tendencies.
The results of the Functional Needs Assessment suggested that Mr. C had the ability to perform many tasks independently. However, home visits indicated that he had trouble completing all the steps in a task and in initiating behaviors on his own. For example, Mr. C was brushing his teeth less than once a week; his clothing was soiled, wrinkled, and unkempt; his fly was not always zipped; and his hair was typically uncombed.
He also scored low in the areas of planning and the use of leisure time. Mr. C had not interacted socially with others outside his family, worked at a job, or attended school for 11 years. The environmental assessment also revealed that Mr. C's belongings, including medication, clothing, and important papers, were strewn haphazardly in drawers and on countertops. Although the apartment was generally dusty and dirty, no glaring safety hazards were observed.
After the test results were explained to Mr. C, his participation was elicited in developing and using environmental supports. Mr. C made an audiotape of his own voice reminding him that "no one can hear my thoughts." He listened to the tape through earphones while he was riding the bus. Mr. C made up a list of things to do when he was bored in his apartment, including washing dishes, listening to music, and going for a walk. The list was written in large and colorful letters and placed on the refrigerator door.
Adaptations set up in the apartment during brief weekly visits over the next month included providing a medication container and alarm reminder, organizing the closet and cupboards, making sure that Mr. C's clothing was easily accessible either hung in the closet or folded, placing his toothbrush and toothpaste in a basket attached to the bathroom mirror along with a sign that read "Did I Brush My Teeth Today?" placing a full-length mirror on the back of the bathroom door with a sign listing the criteria for Mr. C's appearance checks before leaving the bathroom, and providing a file box for important papers. The color of the lettering and the backgrounds of signs used for cognitive adaptation training were changed every other visit to capture and sustain Mr. C's attention.
After three months in the cognitive adaptation training program, Mr. C reported that he was able to select an activity when he was bored by visually "scanning" the list "in his head," enabling him to remove the list from the refrigerator. Mr. C was brushing his teeth daily, and family members reported that his appearance was much better—for example, on five of seven days his hair was combed and his clothing was neat. He reported more favorable experiences when meeting others and attributed this change to his improved appearance. He was able to locate important documents for appointments. The audiotape enabled Mr. C to increase the amount of time he spent outside of his apartment from three to 12 hours weekly.
Later in Mr. C's cognitive adaptation training program, we worked with him to develop a schedule for cleaning his apartment. A calendar with prompts for cleaning tasks was placed on the refrigerator, and step-by-step instructions were attached to cleaning supplies—for example, "1. Get a bucket. 2. Add water" and so on.
We worked on his use of leisure time by providing a bicycle and movie tickets and helping him to enroll in a cooking class. Mr. C learned to create his own compensatory strategies, such as placing his book on a ledge by his door to remember it for class. He was not hospitalized during the nine months that he was followed by therapists from the cognitive adaptation training program.
Case 2
Mr. V was 43 years old and was living in a board-and-care home when he was contacted by the cognitive adaptation training team. He had shown signs of disinhibition and severe executive impairment.
Mr. V had been hospitalized more than 20 times in his life, most recently for four consecutive years. He had a GAF score of 22 and could not correctly state the day, date, or time consistently. He had somatic delusions, auditory hallucinations, and tangential speech. The results of the Functional Needs Assessment indicated that Mr. V was refusing to brush his teeth because they were sore. He was wearing clothing that was too small for his size and inappropriate, such as heavy jackets in summertime and several shirts at the same time.
Observation indicated that he wore the inappropriate clothes because they were hanging in the closet. He had very poor kitchen and safety skills and used objects in inappropriate ways; for example, he cleaned his ears with paper clips. He had difficulty keeping track of his belongings; he would leave his soap and shampoo in the shower he shared with other residents and would leave his spare change and keys at the corner store. He was not engaging in leisure activities.
Mr. V's neuropsychological tests revealed severe impairments (scores more than three standard deviations from the mean of control subjects) in all areas of cognitive function with the exception of visual memory, for which his score was in the 50th percentile of a normative sample. The Frontal Lobe Personality Scale indicated disinhibited behavior—Mr. V was capable of initiating behavior, but he was often distracted and driven by environmental cues. The environmental assessment found that although Mr. V had no structured activities, the staff of the board-and-care home where he lived were well informed, warm, and supportive. His medication regimen was supervised by staff, and his laundry was done by staff.
Cognitive adaptation training interventions for Mr. V included placing a large calendar by his bed with a marker attached to check off days, providing him with a watch, obtaining special toothpaste and an extra-soft brush for his sensitive teeth, hanging on the wall a simple daily activity checklist with pictures rather than words to capitalize on Mr. V's relative strength in visual memory, placing a large brightly colored basket on a peg at eye level for his showering supplies, removing all paper clips from his room, and providing washcloths for ear cleaning.
Clothing that did not fit or was inappropriate for the weather was removed from Mr. V's closet. It was replaced with complete outfits, each consisting of a pair of pants and one shirt stored in a separate plastic container labeled with the day of the week. For trips outside the home, Mr. V was given a pack to attach to his waist for important belongings.
After three months, Mr. V regularly checked off the days of the week before going to bed and was aware of the date and time on 80 percent of occasions. Every day he brushed his teeth, used a washcloth to clean his ears, and dressed appropriately. Moreover, he no longer left his belongings behind when he was out of the home.
Over the next six months, Mr. V worked on social and leisure skills. The cognitive adaptation training therapist arranged for Mr. V to participate in a psychosocial group. Comic books and a radio were also provided, which Mr. V used daily. The therapist helped Mr. V obtain a bus pass and taught him to look for specific landmarks to avoid distraction by novel stimuli en route to his destination. Last, Mr. V was enrolled in a work program, which included compensatory strategies focused on removing distracting stimuli and setting up obvious cues for appropriate work behaviors.
At the end of nine months of cognitive adaptation training, Mr. V was working regularly and had not been rehospitalized since the start of the program. This nine-month period constituted his longest continuous tenure in the community in more than 20 years.
Conclusions
Preliminary results of a randomized controlled trial of cognitive adaptation training have indicated that rehospitalization rates are significantly reduced for participants compared with those in control conditions (23 percent compared with 50 percent) (
5). In addition, participants in cognitive adaptation training do significantly better in reducing positive symptoms and improving motivation and community functioning (
9).
Cognitive adaptation training has many characteristics in common with intensive case management techniques, including small caseloads, home visits, and in vivo supports. However, cognitive adaptation training differs from these techniques by implementing more systematic and specific supports in the client's environment. In cognitive adaptation training, the cues and compensating measures are left in place for lengthy periods of time, even in the absence of the trainer or therapist. Additional research is planned to determine whether compensatory strategies significantly increase benefits to clients who are already participating in programs of assertive community treatment.
Afterword by the column editors: Cognitive adaptation training is similar to the wraparound services that have been provided effectively for decades to persons with head injury (
10) and mental retardation (
11). In pointing out that the antecedents, or supports, as well as the consequences, or reinforcers, of behavior can have a profound impact on rehabilitation, Dr. Velligan and Dr. Bow-Thomas have reminded us of the importance of behavior analysis in functional assessment.
Innovative approaches to antecedent control of behavior have been reported to be highly effective in addressing a wide range of developmental disabilities and in special education contexts (
12). In addition, the efficacy of contingent use of consequences to shape and reinforce adaptive behavior has been described for persons with schizophrenia and other mental disabilities (
1,
2). Through careful, thorough, specific, and observable measurement of behavior and its environmental antecedents and consequences—as well as through the use of selected neuropsychological tests—we should be able to improve rehabilitation outcomes for many more individuals.
Acknowledgments
This work was funded partly by a grant from the National Alliance for Research on Schizophrenia and Depression, the Hogg Foundation for Mental Health, and the Friends for Psychiatric Research.