According to a recent report (
1), almost 80,000 American military personnel (7.7%) sent to Iraq or Afghanistan since January 2002 had a psychiatric diagnosis before their first combat deployment. Because prior mental disorders are a known risk factor for maladaptive responses to stress and for posttraumatic stress disorder (PTSD) (
2–
4), the wartime vulnerability of personnel with a previous diagnosis is of great interest and potential concern.
Recognizing the importance of this issue, the U.S. Department of Defense established a policy in 2006 regarding deployment-limiting psychiatric conditions (
5). On the basis of this guidance, some conditions, such as psychotic and bipolar disorders, automatically disqualify personnel for deployment. Disqualification for other psychiatric conditions is subject to clinical judgment, with the caveat that the service member must be able to perform assigned duties, be medically stable, not present a danger to self or others, and demonstrate minimal potential for symptom recurrence during deployment. Parallel guidelines exist for physical disorders. The ability to perform assigned duties is of paramount concern.
The impact of military deployment policy for personnel with prior psychiatric diagnoses is unknown because, normally, information is not systematically maintained on mental disorders in war zones. As a consequence, researchers have been unable to quantify psychiatric relapse during combat.
This study used an unprecedented set of mental health data on U.S. military personnel seen by mental health care providers in a war zone. Its purpose was to describe the sociodemographic characteristics of personnel who received an in-theater psychiatric diagnosis, identify the psychiatric conditions most commonly seen during the combat tour, calculate the percentage of these personnel who were given a diagnosis of a psychiatric disorder before receiving an in-theater diagnosis, determine whether branch of service was associated with having a preexisting psychiatric diagnosis, examine the overlap of preexisting and in-theater diagnoses, determine the time interval between predeployment and in-theater psychiatric diagnoses, determine the proportion of personnel for whom providers recommended full return to duty, and examine whether Marines who had two or more deployments were more likely to have a predeployment diagnosis than Marines on their first deployment.
Methods
Data sources
In-theater psychiatric documentation for this study was collected for 1,114 patients between January 2006 and February 2007, when the 1st Marine Division deployed to Al Anbar Province in Iraq. Mental health services were provided by the division psychiatrist and a team of 15 providers, who documented each mental health encounter from their catchment area in the Theater Mental Health Encounters Database (TMHED). The population served by these providers consisted of approximately 30,000 military personnel, primarily Marines but also personnel from other U.S. military services.
TMHED data included demographic characteristics, psychiatric diagnoses, and providers' recommendations about whether the patient should return to full duty. Providers recorded this information on paper forms, and the raw data were entered into an electronic database by mental health staff. In the final version of the electronic file, encounters for each patient were chronologically ordered to allow examination of first mental health encounters in Iraq and subsequent encounters. If a patient received more than one diagnosis during the first encounter, the primary mental health diagnosis was used for analysis.
Data on predeployment psychiatric diagnoses were from the military health care system's electronic database, which includes information on inpatient and outpatient medical visits to military treatment facilities and government-reimbursed private providers. These records are generated for military personnel on every medical encounter, except for those that occur in a war zone or that involve civilian providers not reimbursed through the military health care system, TRICARE. Individuals were deemed to have a psychiatric diagnosis if their medical records included an ICD-9-CM diagnosis code in the range of 290–316, with the exception of 305.1 (tobacco use disorders). Of primary interest was the most recent psychiatric diagnosis before each individual's deployment date. As with the TMHED data, if a patient had more than one diagnosis during the most recent predeployment encounter, the primary psychiatric diagnosis was used for analysis.
Broad categories for psychiatric conditions were used for analyses, with the exception of acute stress disorder and PTSD. Specifically, acute stress disorder and PTSD were included as components of the anxiety disorder category in the analyses, but they were also examined separately because of current interest in these topics (
6).
Data on number of combat deployments for Navy and Marine Corps personnel were provided by the Defense Management Data Center. Information on number of deployments for Army and Air Force personnel was not available to researchers at the time of the analyses, and therefore they were excluded from a subset of the analyses.
Final sample and exclusion criteria
Of the 1,114 patients with verified Social Security Number matches, 36 were reservists. Data for these individuals were excluded from the analysis; documented medical histories for reservists are often incomplete because reservists are ineligible for military health care during some periods. This resulted in a final sample of 1,078 Marine Corps, Army, Navy, and Air Force personnel seen by mental health staff in Iraq.
Statistical analyses
Descriptive statistics (percentages and means) were used to describe the demographic characteristics of the sample, identify the most common in-theater psychiatric diagnoses, determine the overlap between predeployment diagnoses and diagnoses assigned in the war zone, and ascertain which in-theater conditions were associated with a history of receiving mental health care predeployment. Chi square tests were used to identify which services were more likely to have deployed personnel with a predeployment diagnosis, examine whether patients with a predeployment diagnosis were more likely to be recommended for restricted duty, and determine whether the proportion of patients with predeployment diagnoses varied as a function of single versus multiple deployments.
To determine the distribution of time between the date of the most recent predeployment diagnosis and the date of the first in-theater mental health visit, the distribution of intervals between diagnosis dates was plotted and the properties of the distribution were examined. SPSS-PC, version 16.0, was used to conduct all statistical analyses (
7).
Results
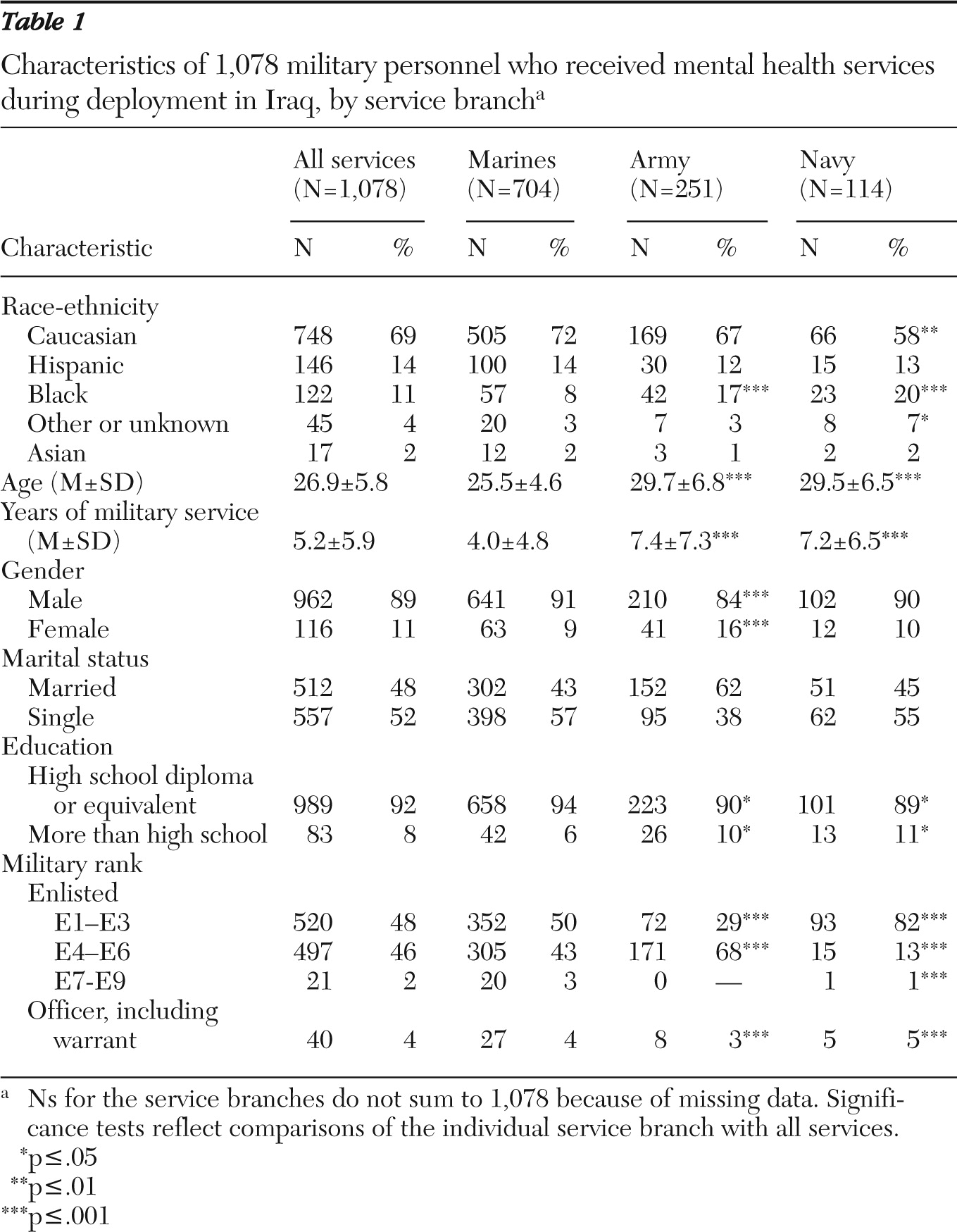
As shown in
Table 1, most patients were men (89%) and Caucasian (69%). The mean age of the sample was 27. Nearly all (92%) entered the military with a high school diploma or equivalent as their highest degree. Although Marines made up the largest proportion of patients (65%), Army (23%) and Navy (11%) personnel were represented, along with a small number of Air Force personnel (N=9, <1%). Army and Navy personnel were older than Marines (Army, t=9.2, df=951, p<.001; Navy, t=6.4, df=816, p<.001) and more likely to have more than a high school education
(χ2=5.4, df=1, p<.05;
χ2=4.5, df=1, p<.05).
Ad hoc comparison of the patient sample with all Navy and Army personnel deployed to Iraq circa 2006–2007 showed that Navy personnel in the TMHED sample did not differ in gender from the Iraq-deployed Navy population but were significantly younger, less educated, and lower ranking. Army personnel in the TMHED sample were more likely than the Iraq-deployed Army population to be female, older, and less educated. Also, there were significantly fewer officers in the TMHED sample than in the population cohorts.
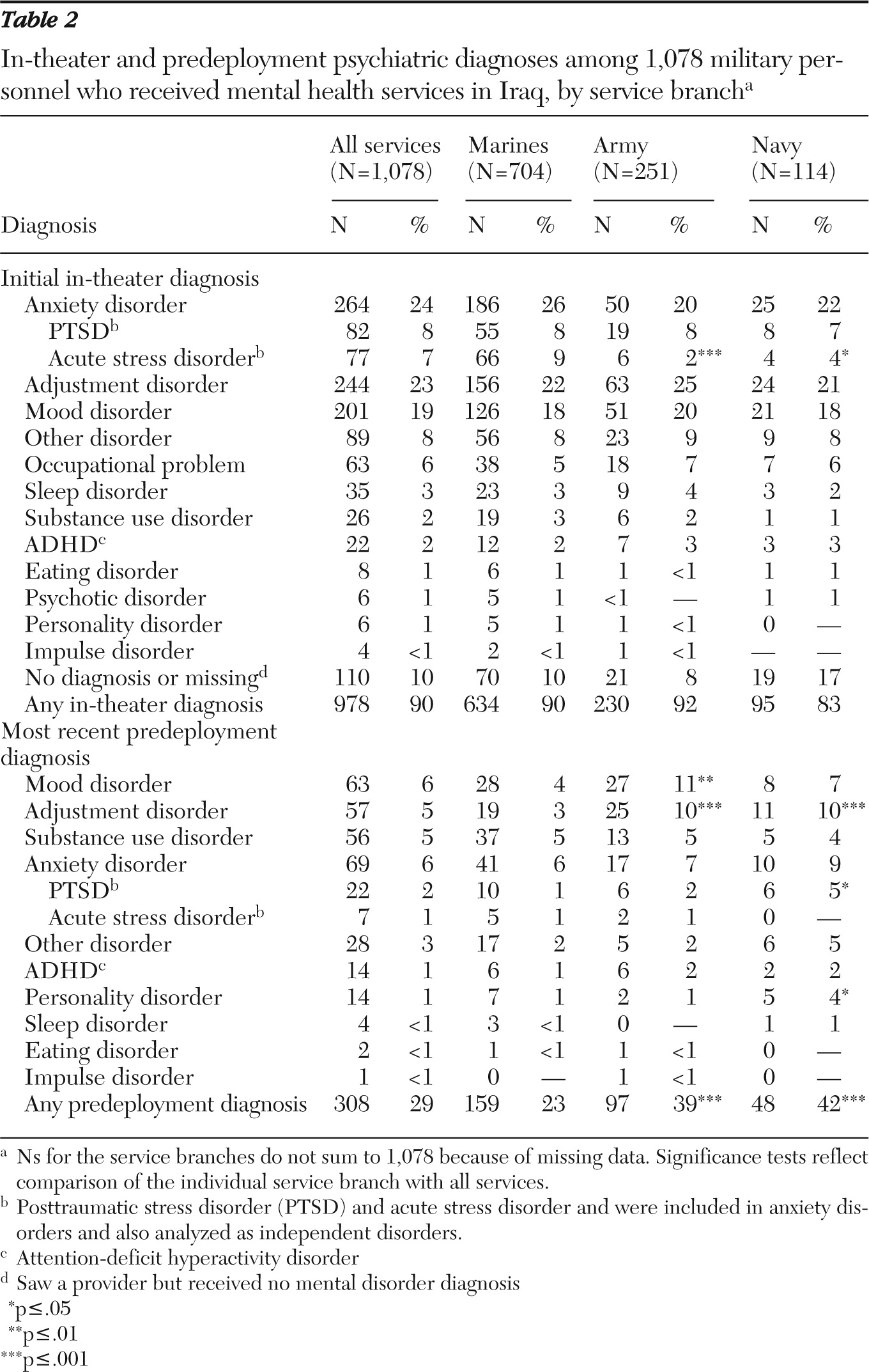
The top half of
Table 2 shows the distribution of diagnoses received in theater by the 1,078 active-duty service members seen by 1st Marine Division mental health providers during their deployment to Iraq between January 2006 and February 2007. The diagnoses shown are the first received during each service member's deployment. The most frequent diagnoses, by far, were anxiety disorders, adjustment disorders, and mood disorders. Ten percent of patients in the sample did not receive a diagnosis from the mental health staff. Nearly every diagnosis was equally distributed across service branches.
The lower half of
Table 2 shows predeployment diagnoses. Of the 1,078 patients, 29% had a psychiatric diagnosis in their medical records before their first in-theater encounter with mental health services. The percentage of patients with a prior mental disorder varied substantially by service branch (Air Force personnel were omitted from this comparison because of the insufficient sample size). Compared with Marines, Army and Navy personnel who received in-theater mental health services were significantly more likely to have prior diagnoses (Army,
χ2=29.3, df=1, p<.001; Navy,
χ2=20.1, df=1, p<.001). In particular, a prior diagnosis of an adjustment disorder was more common among Army and Navy personnel. Twenty-three percent of Marine Corps patients, 39% of Army patients, and 42% of Navy patients seen by mental health providers in Iraq had previous psychiatric diagnoses in their medical records.
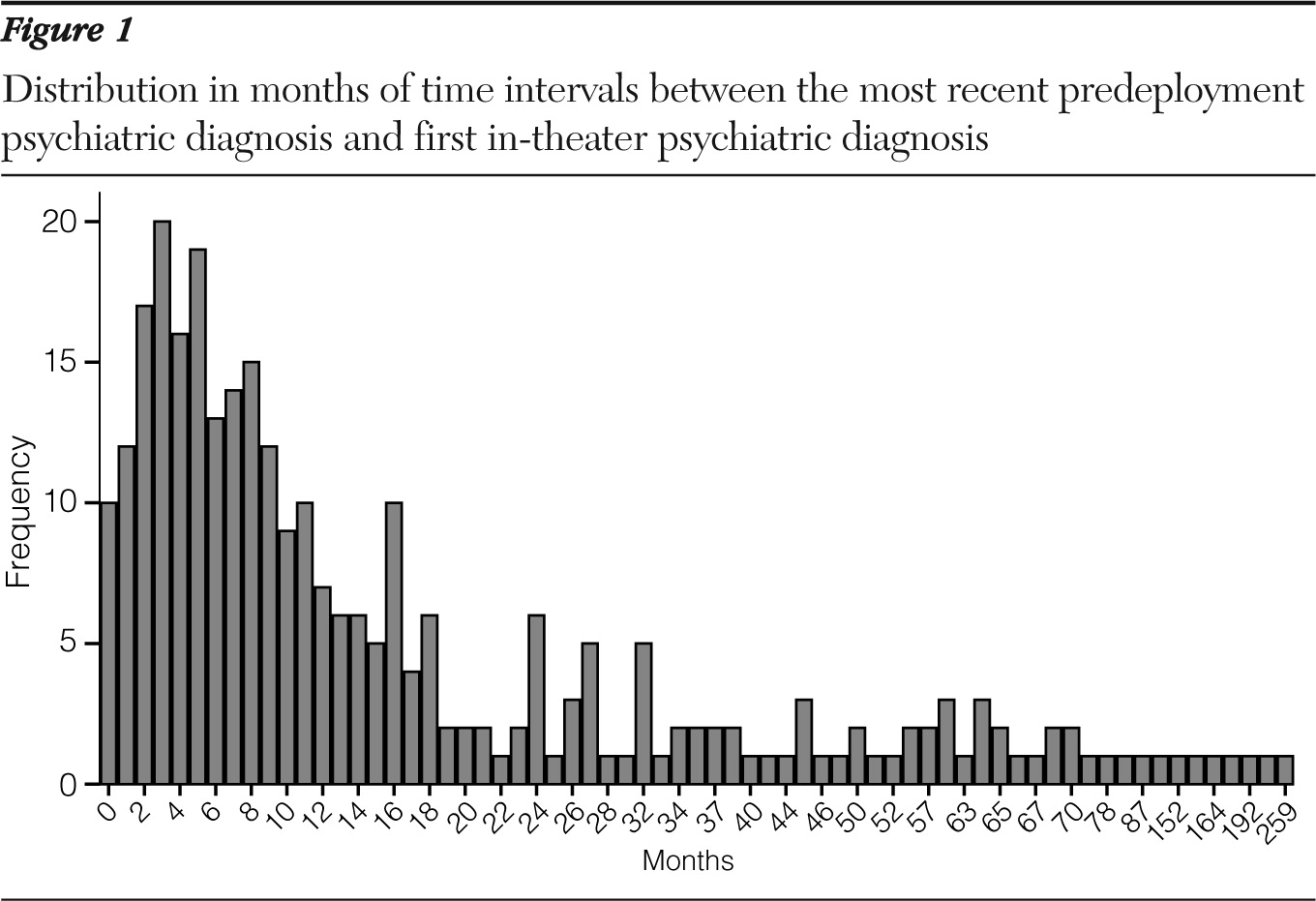
The mean±SD time interval between the most recent predeployment psychiatric diagnosis and the first in-theater mental health encounter was 21±34 months. As shown in
Figure 1, the distribution of time intervals between diagnoses has a pronounced positive skew, indicating that predeployment diagnoses tended to be relatively close in time to in-theater diagnoses. Of the 308 patients in the sample with predeployment diagnoses, 155 (50%) received the diagnosis in the nine months before the mental health encounter in Iraq.
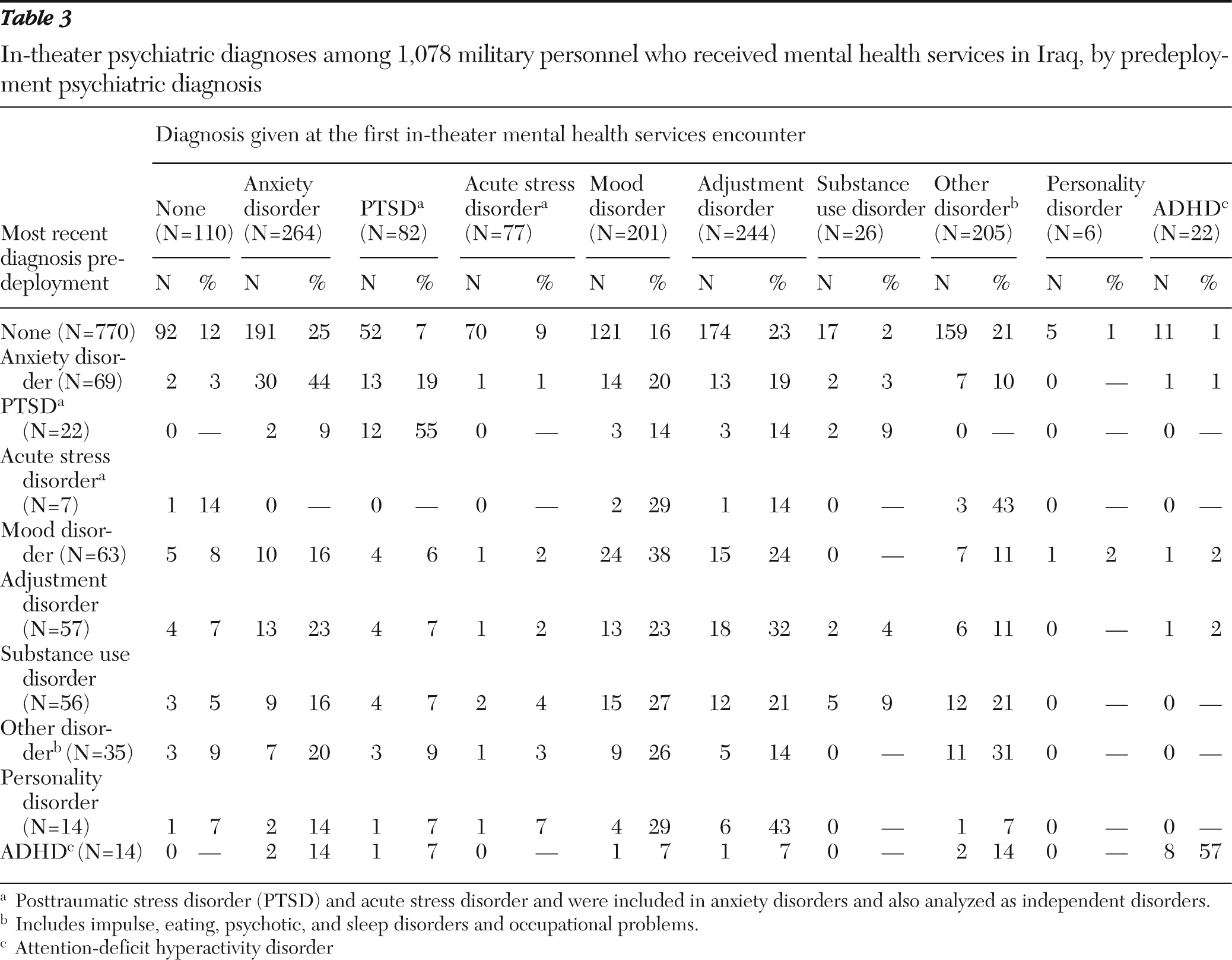
Table 3 shows the overlap between the first diagnosis received in Iraq and the most recent predeployment diagnosis. Patients who had no prior psychiatric diagnosis (N=770) most often received in-theater diagnoses of anxiety (25%) and adjustment (23%) disorders, followed by “other” (21%) and mood disorder (16%) diagnoses. Among patients with a prior psychiatric diagnosis, the highest rate of relapse (receipt of the same diagnosis in theater) was for attention deficit hyperactivity disorder (ADHD) (57%), followed by anxiety disorders (44%) (especially PTSD [55%]), mood disorders (38%), and adjustment disorders (32%). Few patients had a diagnosis of ADHD or PTSD; however, more than half of those with an in-theater diagnosis of these disorders had a previous diagnosis of the same condition. Approximately one-third of patients diagnosed as having mood or adjustment disorders in theater had previous diagnoses of the same conditions.
Substance use disorder was the most noteworthy counterexample. Predeployment substance use disorder diagnoses rarely preceded in-theater substance use disorder diagnoses. Instead, more than 20% of patients with a predeployment substance use disorder diagnosis received either mood or adjustment disorder diagnoses during their combat deployment.
We determined the proportion of personnel who were recommended for return to full duty after being seen by a mental health provider. Overall, providers recommended no restriction of duties for 82% of the sample (N=886). The likelihood of return to full duty was not significantly different between individuals with or without predeployment psychiatric diagnoses.
Additional Marine Corps analyses
As explained above, single and multiple deployments could be compared only for Marine Corps and Navy personnel. Because Marines constituted 65% of the sample, our analysis of multiple deployments was based on Marines only. Fifty-two percent of Marines in the patient sample were on their first combat deployment, and 48% had experienced at least one previous combat deployment. Marines with more than one deployment were no more likely to have had a documented psychiatric disorder before their current deployment than Marines on their first deployment. In addition, there was no significant difference in in-theater diagnoses between Marines with multiple prior deployments and Marines without multiple deployments.
Discussion and conclusions
This study represents the first documented attempt to link preexisting psychiatric conditions with mental health problems observed in a war zone among American forces. The results provide valuable information regarding the characteristics of military personnel seeking treatment in theater and the types of diagnoses most commonly received before and during deployment. Specifically, a substantial proportion of personnel who received an in-theater diagnosis had a preexisting mental disorder noted in their medical records, and relapse—or receipt of the predeployment diagnosis in theater—was relatively common.
By far the most frequent diagnoses in Iraq were a constellation of anxiety disorders (including acute stress disorder and PTSD), followed by adjustment disorders and mood disorders. These findings are similar to diagnostic trends documented in a combat-deployed British military cohort (
11). Among military personnel, the prevalence rates of anxiety and mood disorders appear to be higher among those in combat deployments compared with those who have never deployed (
1). This is consistent with findings that anxiety disorders are elevated among combatants (
8–
11).
Twenty-nine percent of active-duty personnel who were seen by a team of mental health providers in Iraq had prior psychiatric diagnoses. This may indicate that individuals with preexisting psychiatric conditions constitute a disproportionate share of personnel receiving mental health services in a combat zone. Our data for Marines are the most robust for the purpose of examining this possibility. Twenty-three percent of Marine Corps patients seen in theater had a previous psychiatric diagnosis (
Table 2). Taubman (
1) reported that among the Marines who deployed to Iraq or Afghanistan between January 2002 and December 2008, 5% had a psychiatric diagnosis before their first deployment and approximately 15% had a psychiatric diagnosis in the years after their first deployment (
1). Therefore, Taubman's data suggest that the likely range of psychiatric diagnoses among Marines with one or more deployments should fall between 5% and 15%. Thus the proportion of Marine Corps personnel with a prior psychiatric diagnosis (23%) who were seen in the mental health clinic in Iraq falls outside Taubman's 5% to 15% range. This indicates that Marines seen for mental health concerns in the war zone had relatively high rates of prior psychiatric diagnoses. If the midpoint of Taubman's range, 10%, is used as the expected incidence of psychiatric disorders among all deploying Marines, then the rate of 23% is approximately double that for the entire Marine Corps.
In our study Army and Navy personnel who were seen for in-theater mental health issues were significantly more likely than their Marine Corps counterparts to have a prior diagnosis. This is consistent with Taubman's (
1) finding that at a population level, Marines have lower rates of predeployment psychiatric diagnoses than any other service. Army and Navy personnel in the sample were also older, however, which might increase the likelihood of having a prior diagnosis simply because the observation time for these individuals was greater. Our data do not allow us to identify with certainty the reason for differences across services.
Although patients with previous psychiatric problems may have been overrepresented in the in-theater sample, we found no evidence that having a prior psychiatric diagnosis was associated with diminished functional competence. Specifically, having a documented preexisting disorder did not decrease the likelihood of being recommended for return to full duty. However, return to duty might be influenced by factors other than symptom severity.
Receipt of the same diagnosis in theater was particularly common for personnel who had predeployment PTSD and ADHD diagnoses and rare for those with substance use disorder diagnoses. More than half of the patients with an in-theater diagnosis of ADHD or PTSD had a previous diagnosis of the same condition. The discontinuity of substance use problems is not surprising given that consumption of both alcohol and drugs is prohibited in combat zones. Nevertheless, it is interesting that substance use disorder diagnoses accounted for over 20% of the predeployment diagnoses of patients who were given in-theater mood and adjustment disorder diagnoses. This most likely reflects the high rate of comorbidity of substance abuse and other mental health problems. Finally, Marines with more than one combat deployment were no more likely than Marines on their first deployment to have had prior psychiatric disorders.
The findings complement the work of Taubman (
1), who examined the association between predeployment mental disorders and mental disorders diagnosed after return from deployment. Although Taubman had no intermediate data from war zones, he found that service personnel who had received a psychiatric diagnosis before deploying were more likely than their counterparts with no predeployment diagnosis to receive a psychiatric diagnosis after returning from a deployment. Moreover, Taubman found that recurrence of previously diagnosed disorders was common. Our data suggest that recurrence of mental disorders extends into the war zone as well.
As noted above, Department of Defense policy guidance on deployment-limiting psychiatric conditions states that in order to be deployable, the service member should demonstrate minimal potential for recurrence of symptoms in a deployed environment (
5). Our results offer a mixed perspective on the success of this policy. Clearly, a significant proportion (29%) of patients experiencing mental health problems in a combat zone had preexisting conditions. However, if recommendation for restricted duty can serve as a proxy for overall fitness, then personnel with preexisting and new-onset mental health conditions did not differ in the ability to perform their jobs. In addition, because most of the in-theater patients did not have known preexisting disorders, factors other than prior mental health concerns clearly influence resilience during combat (
12).
Any attempt to further restrict deployability of service members with psychiatric diagnoses might lead to greater avoidance of care. Therefore, tightening current deployment policy might have severe and unintended negative consequences. One caveat, however, is that over 50% of the personnel with a predeployment psychiatric diagnosis had received the diagnosis in the nine months before their encounter with mental health services in Iraq. Further study may be advisable to determine whether a time-based algorithm for deployability is needed. This is particularly true for PTSD, a condition for which a very high rate of repeat diagnosis in theater (55%) was found. We believe that our current data need to be augmented with additional cases to determine whether a minimum time should be established between receipt of a diagnosis and eligibility for deployment and whether it should vary by diagnosis
Our research has several limitations. First, our methods introduced several sources of potential bias. Selection bias is a possibility because only service members who sought treatment from mental health professionals were eligible for inclusion. Predeployment care received from other sources, such as providers outside of the TRICARE system, is unknown. Also, because participants were evaluated by multiple providers, there is a possibility of inconsistent symptom interpretations. Furthermore, we cannot report on the well-being of all service members who were sent into combat after receiving a psychiatric diagnosis. Rather, our data reflect a specific patient population at a given place and time.
In addition, military personnel who had prior experience working with mental health clinicians may have been more likely to seek treatment in Iraq because of a diminished sense of stigma. We cannot test this hypothesis with our data. However, no other data exist that would allow broader examination of mental health conditions during combat. The information reported here is unprecedented and provides a unique glimpse into mental health concerns in a war zone.