Homelessness, defined as not having a fixed, regular, and adequate nighttime residence, is a common phenomenon in our contemporary societies. In Canada, an estimated 150,000–300,000 people (.5%–1.0% of the population) are homeless, living in shelters, or living on the streets; on any given night, 40,000 people stay in homeless shelters (
1). In Ottawa, 7,514 persons used emergency shelters in 2008, for a mean duration of 51 days (
2). The homeless population is particularly vulnerable, because homelessness is linked to social isolation, poor health, and increased mortality. The relationships between homelessness, foreign origin, and schizophrenia are complex.
Most studies observe that rates of schizophrenia are higher among homeless persons than in the general population, for which the point and lifetime prevalence estimates are lower than .5% (
3). Two reviews observed a large range for rates of schizophrenia in the homeless population (
4,
5). When considering only studies based on representative samples and using standardized diagnostic instruments, investigators have found that the prevalence ranged between 4% and 16%, with a weighted average of 11% (
4). The only Canadian study using a standardized instrument reported a rate of 11% for lifetime schizophrenia among 750 homeless persons in Montreal and Quebec City (
6). Two other studies using self-reports found lower rates of schizophrenia and other psychotic illness among shelter users: 6% for schizophrenia in Vancouver (
7) and 6% for psychotic disorders in Toronto (
8). The rates of homelessness are also elevated among persons with schizophrenia. In a large U.S. public mental health system, 20% of 4,307 patients with schizophrenia were homeless (
9). In Europe, the rate of patients with schizophrenia who have experienced homelessness was 33% in the United Kingdom, 9% in France, and 8% in Germany (
10). Homelessness has a very negative impact on individuals with schizophrenia (
11). For example, access to medical and psychiatric treatment becomes more difficult. Homeless people engage in behaviors that place their health at risk, are frequently alcohol and drug abusers, and also experience high levels of violence. Consequently, their life expectancy is shortened: persons with schizophrenia have a standardized mortality ratio twice as high as that of the general population, and those who are also homeless have a still higher ratio (
12).
The proportion of homeless people in the general population is not easily estimated. Moreover, in some countries, a nonnegligible proportion of immigrants do not have legal documentation. Consequently, it is difficult to obtain reliable estimates of the percentage of foreign-born individuals among homeless people. European studies have reported higher rates of foreign-born persons among the homeless than among the general population (
13,
14). But Canadian studies found that the proportion of foreign-born persons was lower among homeless people than in the general population: 18% in a shelter survey versus 38% of the population in greater Vancouver (
15), 32% versus 46% in Toronto (
16), and 11% versus 18% in Montreal (
6). The differences between Europe and Canada are possibly related to differences in the immigration process. In Canada the selection criteria favor immigrants in the economic class (between 55% and 60% of immigrants from 2000 to 2008) (
17); family reunion (between 24% and 29% during the same period) is also privileged. [Details on immigrant selection criteria are available in an online appendix to this article at
ps.psychiatryonline.org.]
A large body of research in Europe observes an increased risk of schizophrenia in foreign-born compared with native-born populations. In a landmark meta-analysis of 18 studies, 17 of which were from Europe, the relative risk of schizophrenia associated with immigration was estimated at 2.9 (
18). Immigrants were also at increased risk of having other psychoses (
19,
20). The risk of schizophrenia was increased among both first- and second-generation immigrants (
18,
21). A comparative study remarked that the risk was observed not only in countries of recent immigration, such as European countries where immigration on a large scale began after World War II, but also in countries of long-standing immigration, such as Australia, Canada, and the United States, which were populated by successive waves of immigrants (
22). In Canada, several studies observed better mental health among recent immigrants compared with the rest of both the general population (
23–
27) and the homeless population (
16,
28). However, these studies did not consider psychosis or schizophrenia.
Very few data are available on the relationship between homelessness and psychosis according to foreign birth. Two early studies of patients with schizophrenia found lower proportions of foreign-born among homeless than nonhomeless men (
29) and a similar trend for women, although the difference was nonsignificant (
30). Two later studies with larger samples found a positive association between homelessness and foreign birth, one among first admissions to psychiatric wards in the United States (
31) and the other among admissions to psychiatric emergency services in Spain (
13), but specific diagnoses were not mentioned. The aim of this study was to examine the relationship between foreign birth and symptoms of schizophrenia and psychosis in a sample of homeless persons.
Methods
Study design
In an evaluation of an ongoing research program to improve outreach psychiatric services for homeless persons (
32), sociodemographic and clinical data of homeless clients assessed by the psychiatric outreach team, Royal Ottawa Health Care Group (Ottawa, Canada), were systematically recorded beginning in 2002. The definition of homelessness in this study was that of the Canada Mortgage and Housing Corporation, which defines homelessness as living in a shelter or on the street or being vulnerably housed (having been homeless in the past year). After referral by partner agencies for potential psychiatric symptoms, individuals were encountered in shelters, drop-in centers, or rooming houses and were assessed by a member of the psychiatric outreach team. The charts of all clients seen between 2002 and 2007 were retrospectively reviewed and then were abstracted and anonymously coded by an experienced research assistant, who consulted the study's senior psychiatrist as needed. No external validation by an independent clinician was performed.
The study was approved by the Royal Ottawa Group Research Ethics Board. No individual informed consent was requested for this retrospective review.
Measures
Sociodemographic characteristics, such as gender, age, and level of education were self-reported, as was country of birth. Forty-six birth countries other than Canada were grouped into larger regions: Africa, Americas excluding the Caribbean, Asia, Caribbean, Europe, and the Middle East. Data regarding ethnic origin were not recorded.
All clients were evaluated by highly trained multicultural and multilingual team members from various clinical disciplines, mainly nursing and social work. They performed psychiatric assessments following DSM-IV criteria and using a semistructured interview format, and, when indicated, they referred individuals to a psychiatrist or a psychologist. Because a psychiatric diagnosis by a specialist was not available for all clients, we used two definitions based on the assessment performed by the clinical staff. First, symptoms of schizophrenia were defined as thought disorders (characterized as disorganized thinking with altered associations), alone or associated with delusions, hallucinations, or both; second, symptoms of psychosis other than schizophrenia were defined as delusions, hallucinations, or both, without thought disorders (the psychosis category contained those reaching a clinical diagnosis of a DSM-IV psychotic disorder other than schizophrenia).
Statistical analysis
Characteristics according to birth in Canada or in another country were compared by chi square test and analysis of variance. The primary dependent variables were symptoms of schizophrenia and symptoms of psychosis other than schizophrenia. For both variables the reference group was constituted by persons without symptoms of schizophrenia or psychosis. The relationships between foreign birth and the two dependent variables were first examined with univariate analyses. Because the associations were similar for men and women, both genders were combined for further examination.
Multivariate analyses were performed with logistic regression, taking into account gender plus possible confounding factors such as age, level of education, and substance abuse or dependence. Because of missing values for these independent variables, the multivariate analyses were performed using the level “unknown” for age, level of education, and substance abuse or dependence. Because living alone or being unemployed might be a consequence of schizophrenia or psychotic illness, marital status and employment status were not included as possible confounding factors. Subsequently, we examined the relationship between region of birth and symptoms of schizophrenia and psychosis in multivariate analyses that used the same independent variables. Only groups consisting of more than five individuals were included in this analysis. The statistical analyses were performed with PASW Statistics 18 (SPSS Inc).
Results
Sociodemographic characteristics of the sample
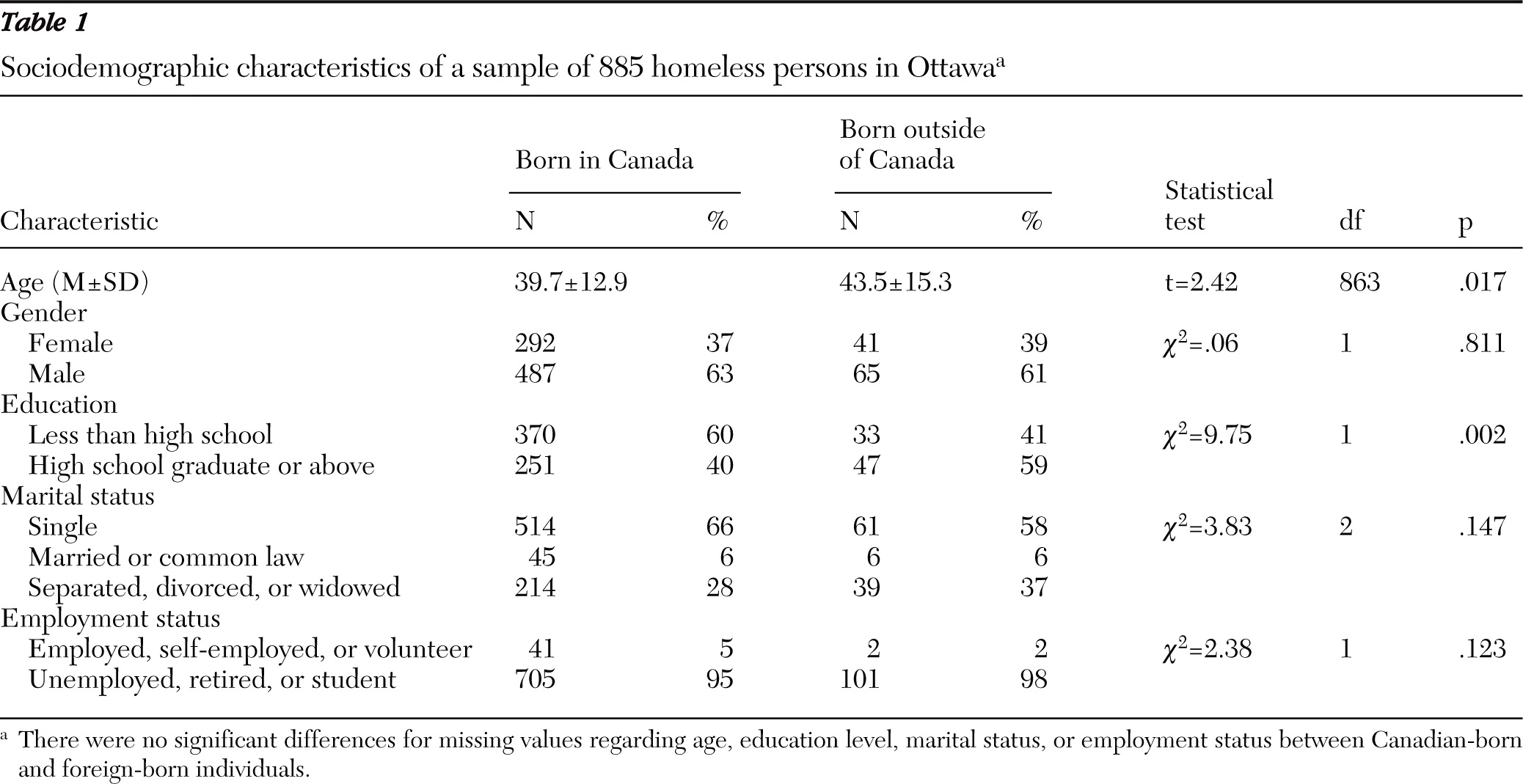
A total of 903 charts that included psychiatric symptoms were reviewed; of these, 885 (98%) included data on country of birth. These individuals constituted the study sample, and their sociodemographic characteristics are described in
Table 1. The sample consisted of 779 Canadian-born and 106 foreign-born persons (12%). The gender distribution was similar in both groups, with an underrepresentation of women (37% and 39%, respectively). Mean±SD age was 40.1±13.3 years (range 16–88). Foreign-born individuals were significantly older, by 3.8 years, than those born in Canada and had a higher level of education. Among the 106 persons born outside of Canada, 33 reported birth in Africa, 27 in Europe, 19 in Asia, 12 in the Americas, 11 in the Caribbean, and four in the Middle East.
Psychiatric symptoms
A total of 146 of 885 individuals (16%) presented symptoms of schizophrenia, and 129 (15%) had symptoms of psychosis other than schizophrenia. The proportions did not differ significantly between the 552 men and 333 women: 17% (N=94) and 16% (N=52) for schizophrenia and 16% (N=86) and 13% (N=43) for other psychotic illness, respectively (χ2=1.77, df=2, p=.41).
The other psychiatric disorders consisted of mood disorders (N=436, 49%), substance (alcohol and drug) abuse or dependence (N=423, 48%), anxiety and panic disorders (N=177, 20%), and developmental delay (N=47, 5%). The total is greater than 100% because some persons had multiple conditions. Substance abuse was reported more frequently by Canadian-born than foreign-born individuals (N=367, 57%, versus N=24, 30%; χ2=19.79, df=1, p<.001, data for persons with unknown use excluded).
Psychotic symptoms and foreign birth
For both genders, persons presenting symptoms of schizophrenia and other psychosis were more likely to be foreign-born than Canadian-born. The association with foreign birth was significant for both genders (women, χ2=24.52, df=2, p<.001; men, χ2=24.14, df=2, p<.001). For both genders combined, the odds ratio [OR] associated with foreign birth was 2.92 (95% confidence interval [CI]=1.74–4.90, p<.001) for symptoms of schizophrenia, and 4.79 (CI=2.92–7.86, p<.001) for symptoms of psychosis.
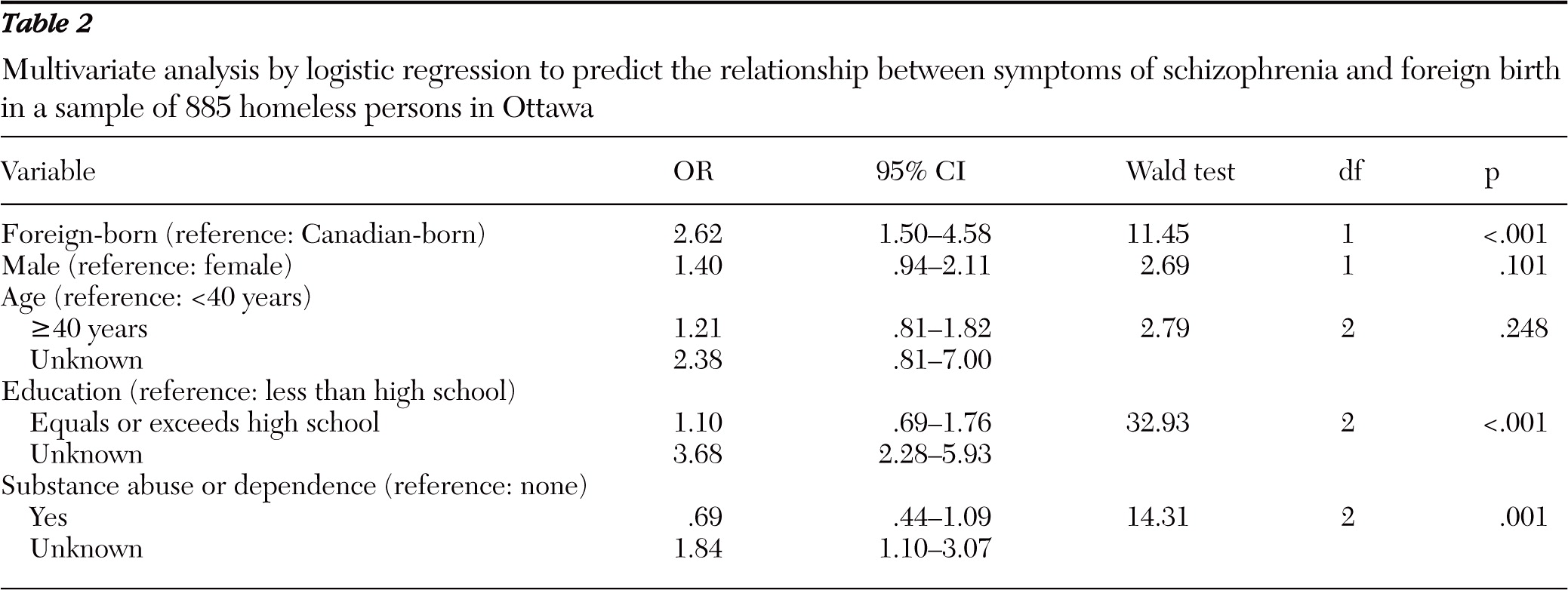
In multivariate analyses including age, gender, level of education, and substance abuse, the relationship between foreign birth and symptoms of schizophrenia remained significant, as shown in
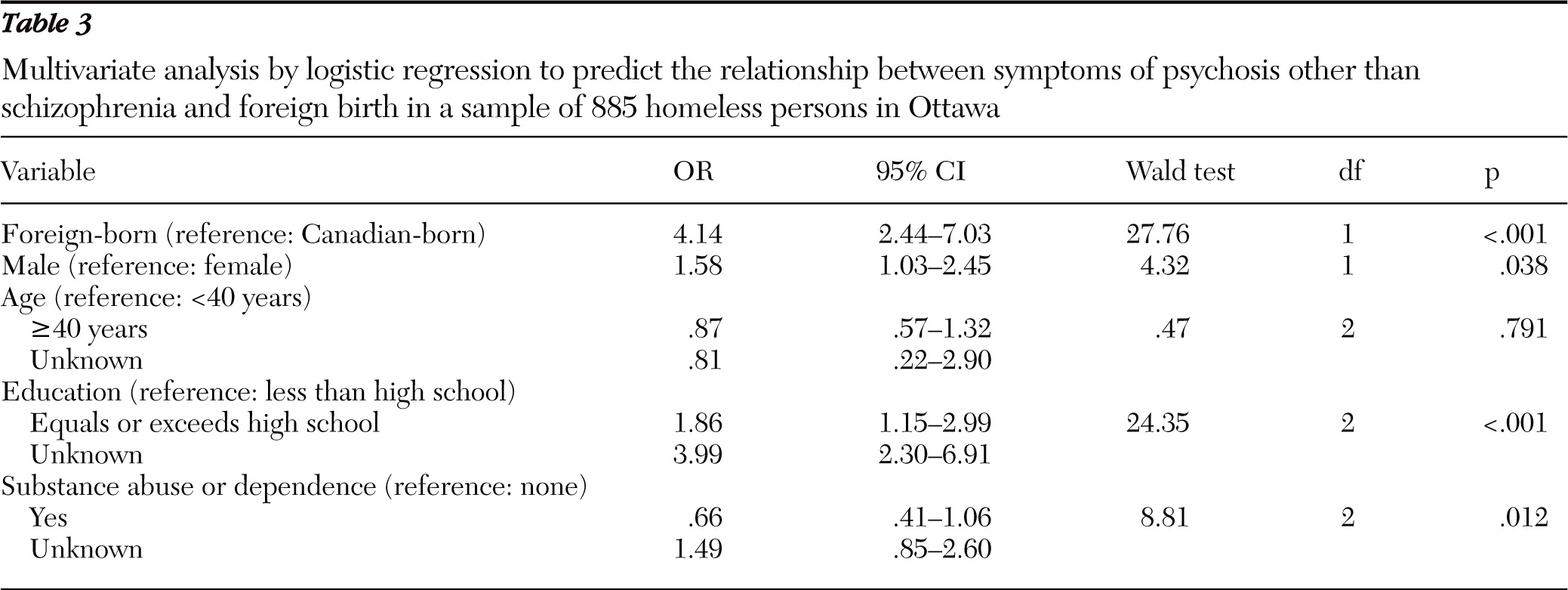
Table 2 (OR=2.62). Examination of region of birth in the multivariate model showed that only birth in Europe was associated with a significantly higher risk (OR=3.75, CI=1.42–9.90, p=.008). Birth in Asia (OR=2.86, CI=.84–9.73, p=.093) and in Africa (OR=2.64, CI=.97–7.19, p=.058) was associated with a marginally higher risk. The relationship with birth in the Caribbean (OR=1.53, CI=.28–8.35, p=.63) and in the Americas (OR=.58, CI=.07–4.95, p=.62) was not statistically significant. The relationship between foreign birth and symptoms of psychosis remained highly significant in multivariate analyses, as shown in
Table 3 (OR=4.14). Male gender and higher level of education were associated with a higher risk of psychosis. With regard to region of birth in the multivariate model, birth in Africa (OR=6.13, CI=2.56–14.66, p<.001), in Asia (OR=5.18, CI=1.66–16.22, p=.005), and in Europe (OR=3.62, CI=1.32–9.95, p=.012) was associated with a significantly higher risk of psychosis. Birth in the Caribbean was associated with a marginally higher risk (OR=3.59, CI=.88–14.59, p=.07). The relationship with birth in the Americas (OR=1.19, CI=.24–5.92, p=.84) was not statistically significant.
Discussion
Strengths of the study
The positive association between foreign birth and symptoms of schizophrenia and other psychotic illness in our sample of homeless persons is of importance because of the high proportion of homelessness in developed countries. It is also a serious burden for public health, given that immigrants represent a substantial percentage of the population in North America.
Limitations of the study
It is not possible to generalize the findings in this sample of homeless persons to the general population. A major methodological issue of our study is the selection of the sample in that all clients were referred for a psychiatric assessment. We cannot exclude that referral might have differed according to foreign birth or language competency. Another important issue is that although the psychiatric assessments were performed by clinical staff, psychiatric diagnoses validated by a psychiatrist were not available for all clients. The assessment used a semistructured interview format that followed DSM-IV criteria but was not validated; this represents another limitation of the study. It is also possible that our definitions led to misclassification: for example, a person with hallucinations and delusions might have been diagnosed as having schizophrenia but was characterized in the study as presenting symptoms of psychosis other than schizophrenia.
Sociodemographic data, including country of birth, were self-reported and not verified by the clinical staff. Country of birth is not always indicative of foreign origin: Canadian persons may be born abroad to Canadian parents; conversely, second-generation immigrants are born in the host country. Data on second-generation immigrants were unavailable in our study.
Validity of the data
The proportion of foreign-born persons was 12% in our sample of homeless persons, lower than the 18% in the general population in Ottawa and the 20% in Canada (
33). Our finding of a lower rate of homelessness in the foreign-born than Canadian-born populations is consistent with other Canadian studies (
6,
15,
16). These results do not exclude the possibility that foreign-born persons in Canada are not using shelters but live in precarious conditions (with friends, extended family, and compatriots). Consequently, it is possible that a less stringent definition of homelessness would provide different results.
Klodawsky and colleagues (
28) reported on a study of 412 homeless persons in Ottawa interviewed in 2002–2003. The study design overrepresented foreign-born women and families, and individuals were selected by their willingness to participate. It is therefore difficult to interpret the significantly higher proportion of foreign-born persons compared with the proportion in our study (24% versus 12%) and the differences regarding region of birth, with more persons born in Africa and fewer in Asia and in Europe in the Klodawsky study's sample. However, other sociodemographic characteristics were quite similar: in both samples, most persons were single and unemployed, and the level of education was higher for persons who were foreign-born than for their Canadian counterparts. This last result is consistent with the report of the 2006 Census (
33) in which a university degree was declared by 32% of immigrants to Canada but only 20% of the Canadian-born population.
We found that 16% of individuals presented symptoms of schizophrenia and 15% symptoms of psychosis other than schizophrenia. The total of 31% is significantly higher than the 13% prevalence reported in a homeless population for a validated diagnosis of schizophrenia and other psychotic disorders in Montreal and Quebec City (
6). The selection of our sample for psychiatric symptoms may explain our higher proportion of individuals with symptoms of psychosis and schizophrenia. Our use of symptoms rather than validated diagnoses of schizophrenia and psychosis may increase the estimates. Also the composition of the homeless population changes over time; for example, in Detroit, the percentage of homeless adults with a schizophrenia spectrum disorder was twice as high in 2002 as in 1992 (
34).
Interpretation of the results
We found an association between foreign birth and symptoms of schizophrenia and psychosis in this sample of homeless persons. The relationship between schizophrenia and foreign origin is in line with findings of international studies (
18,
21,
22). It has been argued that this association was due to differential diagnosis according to ethnic origin or immigrant status. But in our sample, the relationship was observed with symptoms of both schizophrenia and psychosis.
In Canada, studies reporting better mental health among immigrants (
23–
27) did not include symptoms of psychosis or diagnosis of schizophrenia. Early studies using hospital data found evidence of a moderately increased risk of schizophrenia among immigrants. The risk estimates were 1.5 with archival data collected in British Columbia between 1902 and 1913 (
35) and were 1.8 and 1.2 with administrative data collected in all Canadian provinces in 1950–1952 (
36) and in 1961 (
37), respectively. These estimates were in the same range as those reported for other countries of long-standing immigration (
22). The increased risks associated with foreign birth reported by our study—almost three times for schizophrenia and four times for psychosis—were high compared with the estimates reported in other Canadian studies. It is possible that, by chance, our sample included very few second-generation immigrants and consequently maximized the difference between the foreign-born and the native-born populations. We also cannot exclude the possibility that our findings reflect differential staff attitudes according to foreign birth or language of the client. But this is unlikely because the staff was multicultural and multilingual, with interpreters available in case of language barriers. Other plausible explanations are that despite universal health care, access to psychiatric services is hindered for foreign-born compared with Canadian-born persons if they develop schizophrenia or psychosis. Another possibility is that, according to the stress model, foreign-born persons who become homeless are more vulnerable to developing psychosis.
Interestingly, foreign birth, despite being associated in our sample with a lower risk of homelessness, a higher level of education, and less substance abuse, was associated with an increased risk of schizophrenia and psychosis. European researchers have stressed the lower socioeconomic status of immigrants and its possible role in explaining their increased risk of schizophrenia; however, two non-European studies reported a higher socioeconomic status among immigrants compared with native-born populations (
38,
39). A higher level of education does not imply a higher socioeconomic status; despite their educational attainments, immigrants to Canada do not reach a socioeconomic status equal to that of their native-born counterparts. Among persons with a university degree, those who are foreign-born are more likely than those who are Canadian-born to have a job with low educational requirements (
33). Our findings regarding substance abuse are comparable with those of Veen and colleagues (
40), who found similar rates of drug use among patients with a first episode of psychosis who were from ethnic minority groups and those who were born in the Netherlands to native-born parents.
We found that the risk of schizophrenia and psychosis differed according to the region of birth, with a trend for an increased risk in all regions other than the non-Caribbean Americas. These results should be interpreted with caution, because of the small cell sizes and the consequent large CIs.
Conclusions
Despite the methodological shortcomings of our study, its results warrant attention. Persons with schizophrenia or a psychotic illness represent an important segment of the homeless population. In order to address the general issue of homelessness, different strategies should be directed at each of the various segments of this population. A major problem for homeless persons with schizophrenia or other psychotic illness is the lack of access to psychiatric treatment, including a consistent psychiatric team and support for medication purchase, intake, and compliance. Without adequate intervention, homelessness might aggravate psychosis, and psychosis might perpetuate homelessness. Specially designed studies are warranted to obtain more detailed information regarding homeless persons with schizophrenia and psychosis, in order for researchers and clinicians to devise appropriate interventions.
Our finding that a higher proportion of individuals presented symptoms of schizophrenia and psychosis in foreign-born than Canadian-born persons stresses the need for current North American data on this important issue. Because of the low incidence of psychotic disorders, epidemiological studies should include immigrant groups large enough to provide sufficient statistical power. Because of the increased risk of psychotic illness in the second generation, these studies should consider generation of immigration in order to provide reliable estimates of the risk of schizophrenia and psychosis associated with immigration. If our results are confirmed in large and representative samples, mental health services for immigrants should focus on providing earlier and better assistance to foreign-born persons.
Acknowledgments and disclosures
This work was supported by grant HDD 77945 from the Canadian Institutes of Health Research.
The authors report no competing interests.