Substance use disorders are often chronic problems better managed by ongoing monitoring and extended services than by an acute treatment approach (
1,
2). However, the addiction field has focused mainly on aftercare services involving 12-step participation or modalities conducted through specialty substance abuse treatment programs. Many of these increase the benefit of treatment (
3–
9), but in most cases the aftercare period is limited. At some point it ends, and patients become disconnected from the clinic, specialty care providers, and other resources and services (
10).
A growing literature suggests that primary care may play an important role in long-term recovery of substance use disorders. Primary care is an ideal setting for identifying relapse or risk of relapse and offering brief treatment or referring to specialty treatment when needed (
10,
11). Primary care can also address comorbid medical problems, which most substance users have (
10,
12,
13), and this too may facilitate positive long-term outcomes. Studies have found integrated primary care and substance abuse treatment to be effective, especially for patients with medical problems (
14–
18), and some have suggested that the benefit extends to five years (
13,
19). However, the field lacks guidelines for service use after substance abuse treatment, especially in primary care.
This observational study analyzed nine years of prospective data for 991 adults who entered substance abuse treatment in a private, nonprofit managed care health plan. We hypothesized that those who received regular primary care, and substance abuse treatment readmissions or psychiatric services when symptoms were present, would be more likely to achieve remission over time. We developed a measure of continuing care based on the findings, and we examined its relationship to remission over nine years.
Methods
Study participants
Study participants were drawn from two large randomized studies conducted at the Kaiser Permanente Sacramento Chemical Dependency Recovery Program. Kaiser Permanente Northern California is a large, private nonprofit, integrated managed care health plan covering 40% of the Sacramento catchment area population. It provides substance abuse treatment and psychiatric services internally. Most members are insured through their own employer or through a family member's employer.
The substance abuse treatment program provides group-based outpatient and day treatment modalities that include supportive group therapy, education, relapse prevention, family therapy, and individual counseling in a model similar to other abstinence-based, group-format private and public programs. Both modalities last eight weeks, and aftercare is available for ten months. The psychiatry department provides individual and group psychotherapy and medication management. All substance use patients are assigned to (or select) a primary care physician and are encouraged to use primary care for preventive and ongoing health care.
Procedures
The Day Hospital Study compared day hospital treatment with traditional outpatient treatment and recruited patients between 1994 and 1996 (N=1,204) (
20). The Integrated Care Study examined integrated delivery of medical and addiction services and recruited patients between 1997 and 1998 (N=749) (
14). Program components were consistent across both studies. After giving written informed consent, patients completed baseline interviews conducted by research staff at intake. For both studies, follow-up interviews were conducted at one, five, seven, and nine years, with average response rates of 86%, 81%, 84%, and 75%, respectively. In both studies, drug test results for a random subsample found good validity of the self-report data (
14,
20). Institutional review board approval was obtained from the Kaiser Foundation Research Institute and the University of California, San Francisco.
Measures
Demographic characteristics.
The baseline interview included questions about age, gender, ethnicity, education level, household income, and significant life events often related to outcomes, such as marital status and employment status (
21–
24). These questions were repeated at the follow-ups.
Alcohol and drug dependence.
At baseline, questions adapted from the Diagnostic Interview Schedule for Psychoactive Substance Dependence (
25) provided a diagnosis of alcohol and drug dependence and abuse for each of nine substances.
Alcohol, drug, and related problem severity.
Composite scores from the Addiction Severity Index (ASI) (
26) measured alcohol, drug, and related problem severity at all waves. For each follow-up, we created a set of dichotomous markers indicating whether the patient had alcohol, drug, medical, or psychiatric ASI composite scores greater than zero at the prior interview; these binary markers were proxy measures of need for the corresponding types of services in the subsequent period.
Length of health plan enrollment.
Months enrolled in Kaiser Permanente during each of the nine follow-up years were summarized from health plan databases.
Substance abuse treatment.
Duration of index substance abuse treatment episode was measured from health plan databases; completion was defined as remaining in treatment for eight or more weeks without a gap of seven or more continuous days, consistent with the program's definition of dropout for the rehabilitation phase of treatment. Treatment readmissions during the nine years after index treatment were also identified from the databases (
19,
27,
28). Dichotomous measures indicated having any readmission between interviews (that is, year 1 and years 2–5, 6–7, and 8–9).
Psychiatric services.
From the health plan databases, visits to the department of psychiatry were summarized for the periods between interviews. We created a dichotomous indicator of having at least two psychiatry visits for each period (a threshold based on prior research) (
27) and examined its association with long-term outcomes.
Primary care visits.
From the health plan databases, visits to the departments of adult medicine, family practice, or obstetrician-gynecologist were summarized for the periods between interviews. For each period, a dichotomous variable indicated receiving yearly primary care (
19).
Continuing care for substance use patients.
This was defined as receiving yearly primary care visits and substance abuse treatment readmissions or psychiatric services when symptoms were present (details are described in Results).
Remission of substance use disorders as the outcome.
Individuals classified as in remission were either abstaining or were nonproblematic users. Nonproblematic users were those who in the prior month drank four times or fewer and indicated no days of having five drinks or more, did not use marijuana more than once, did not use drugs other than alcohol or marijuana, and reported that they did not have suicidal ideations, violent behavior, or serious conflicts with family, friends, or coworkers (
13,
29,
30).
Data analyses
We conducted all analyses with SAS version 9.1 (Cary, NC). We selected those with at least one follow-up interview who were Kaiser Permanente members for at least 5.4 years during the nine years after intake (N=991). Prior work established that 60% of a given time period struck a good balance between retaining sample participants and accurately predicting utilization for the period (
27,
31). Decisions were informed by sensitivity analyses that compared results by applying different membership criteria (that is, no restriction, full membership, and having health plan membership for different proportions of time during the total follow-up period).
We examined associations between each type of service use (substance abuse treatment readmissions, psychiatric services, primary care, and continuing care) and remission over time by fitting nonlinear mixed-effects multivariate logistic regression models with a random intercept. This model examined the effects of the explanatory variables on the participants' probability of being remitted while allowing the initial status (intercept) to vary for every participant. We fitted an initial model that included demographic characteristics; baseline alcohol and drug dependence; completion of index substance abuse treatment; alcohol, drug, and related problem severity at prior follow-up; and time of follow-up (coded as 0, 4, 6, and 8 at one, five, seven, and nine years, respectively). We next fitted a model that included all three types of services and the interaction terms of each service type and the corresponding binary marker for service need; this analysis controlled for covariates significantly associated with remission at p<.10 in the initial model. Finally, we created a measure of continuing care and examined its association with remission over time while controlling for the same set of covariates. Odds ratios (ORs) and 95% confidence intervals (CIs) for the predictor variables were calculated on the basis of the parameter estimates.
Results
Final sample
Participants who were included in the final analytical sample (N=991) had more women (39% versus 34%; χ2=5.24, df=1, p<.05), more who were 50 or older (16% versus 8%; χ2=89.17, df=4, p<.001), more with college or higher education (41% versus 34%; χ2=25.57, df=2, p<.001), more with household incomes ≥$40,000 (46% versus 31%; χ2=45.65, df=1, p<.001), and more with higher mean±SD alcohol ASI (mean±SD=.43±.32 versus .40±.31; t=–2.27, df=1,947, p<.05) and lower average drug ASI (mean±SD=.11±.12 versus .14±.12; t=4.26, df=1,945, p<.001) composite scores at baseline than those who were not included.
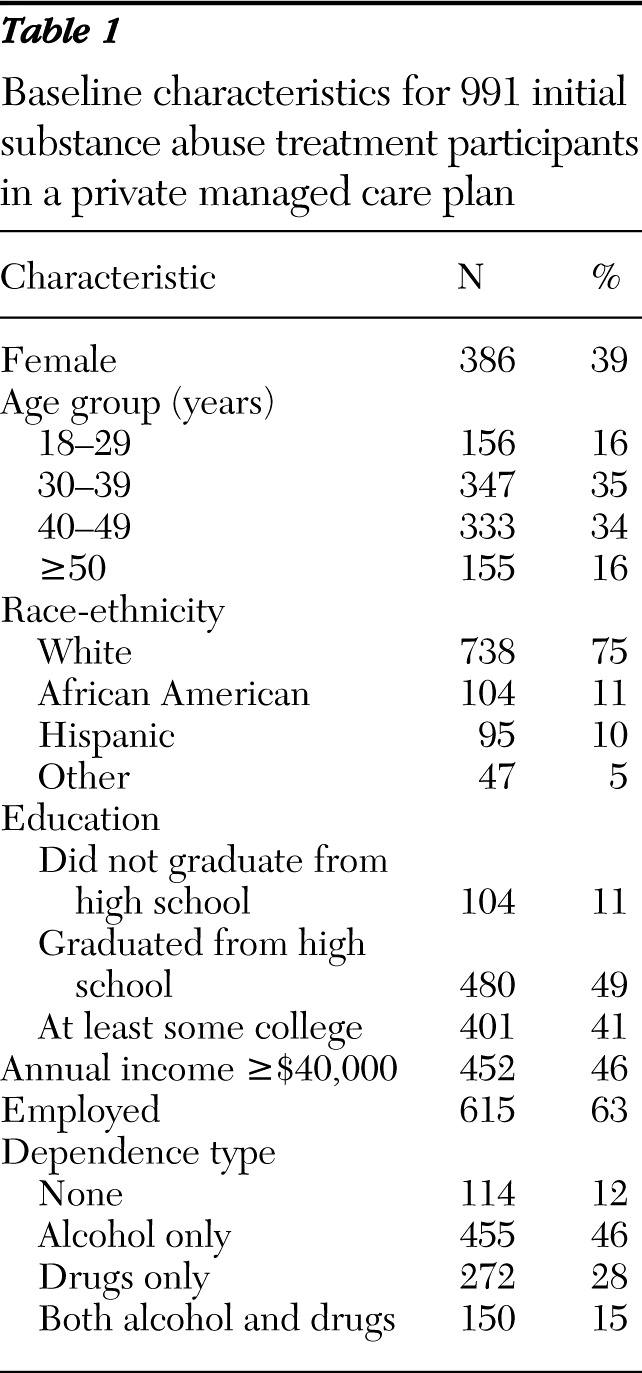
Table 1 presents individual characteristics at treatment entry for the final analytical sample. The mean±SD age was 39.7±10.6 years. More than half of the patients were dependent on alcohol: 455 (46%) were dependent on alcohol only, and 150 (15%) were dependent on alcohol and drugs. In addition, 272 (28%) were dependent on drugs only, and 114 (12%) were not dependent, with most meeting criteria for a diagnosis of substance abuse.
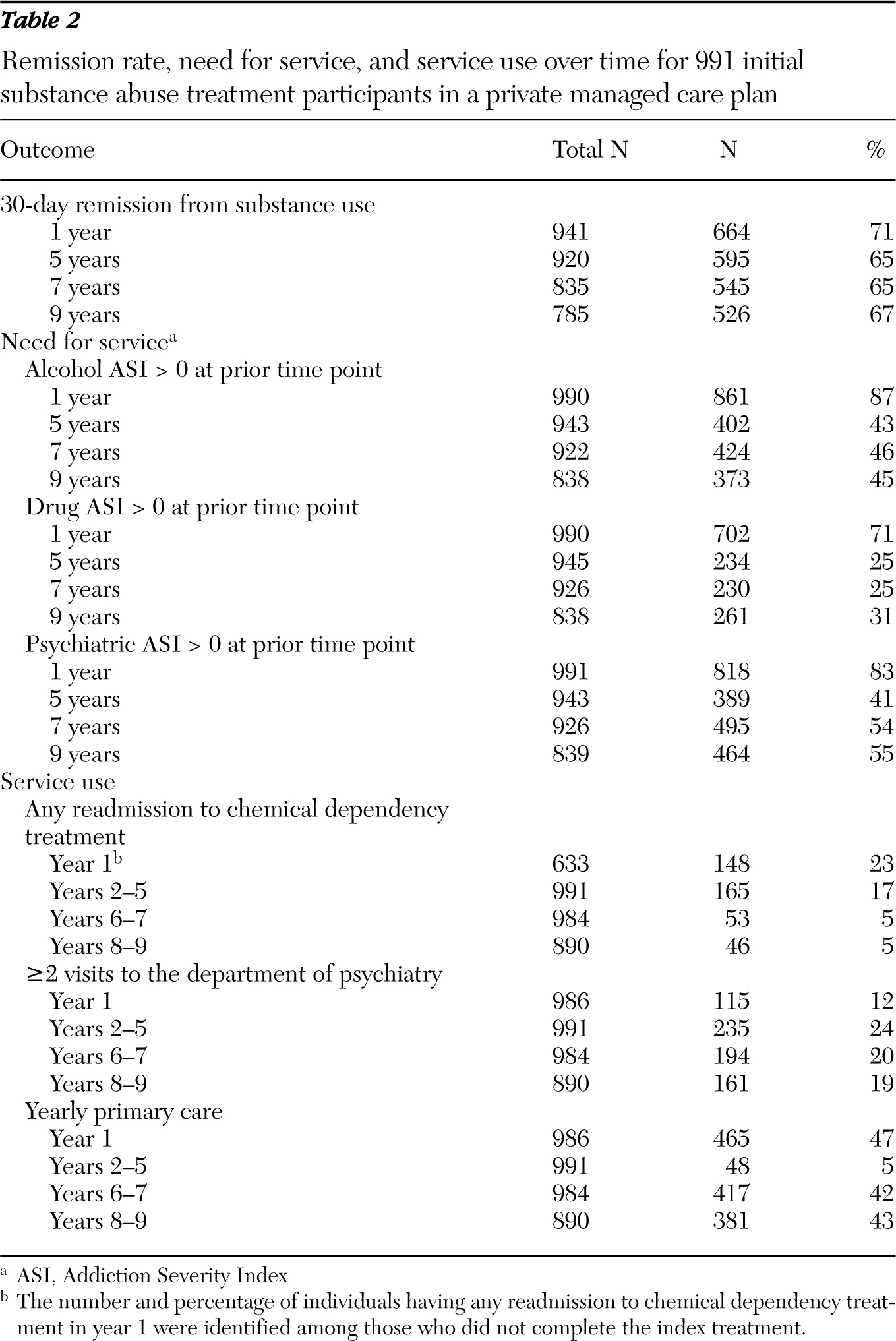
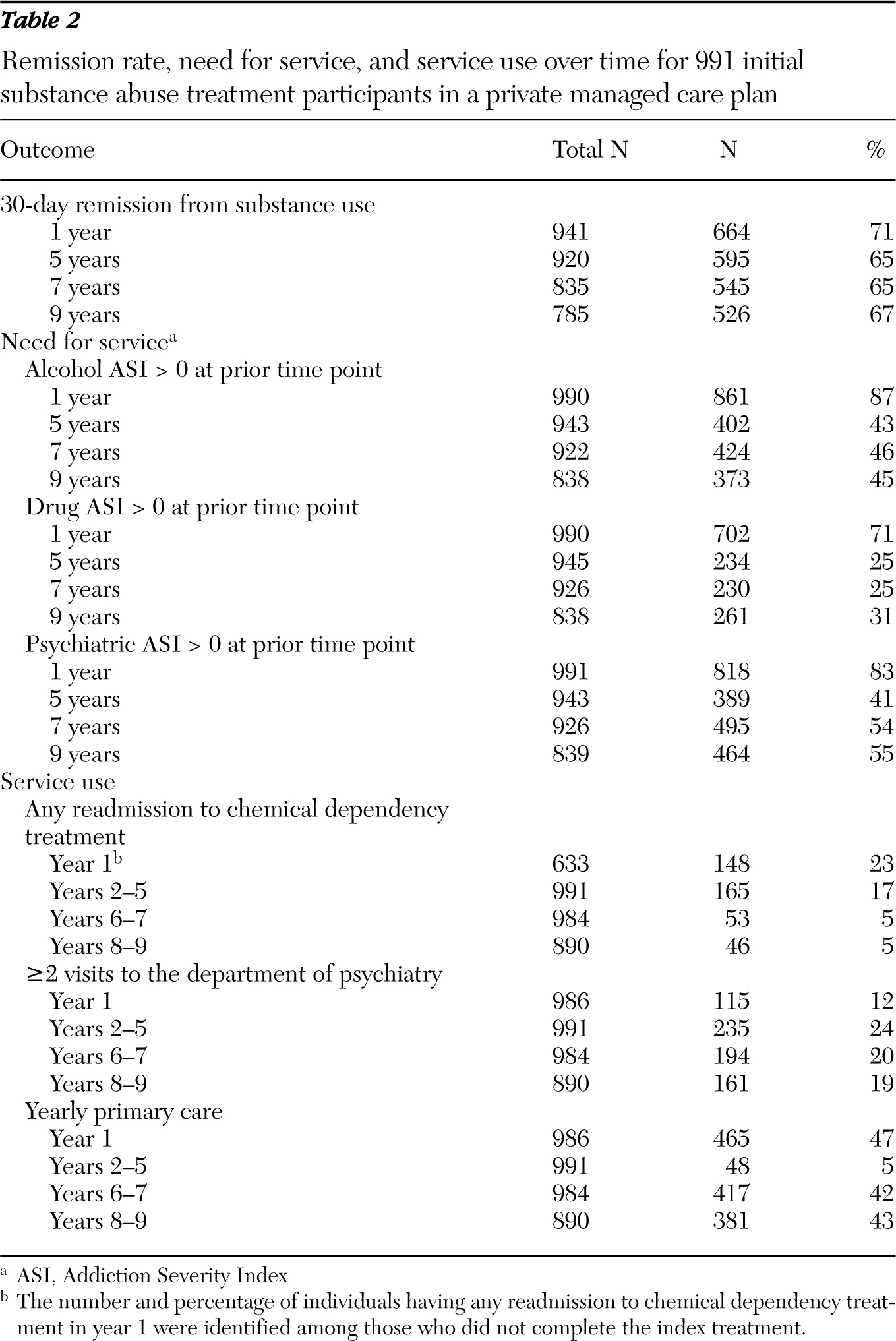
At the one-year follow-up, 71% of the sample met remission criteria; 65%, 65%, and 67% achieved remission at five, seven, and nine years, respectively. Over 40%, 20%, and 40% had alcohol, drug, and psychiatric ASI composite scores greater than zero over follow-ups after year 1, respectively, indicating need for the corresponding specialty care. A total of 354 (36%) patients completed eight or more weeks of index substance abuse treatment; among those who did not, 23% had a readmission to substance abuse treatment during the first year. Proportions of patients with readmissions after the first year were low. About one-fifth used psychiatric services during follow-up periods after year 1. Forty-seven percent of the sample had a primary care visit in year 1, but the percentages for yearly primary care visits dropped to 5% during years 2–5 and to 42% and 43% during years 6–7 and 8–9, respectively (
Table 2).
Individual characteristics and remission over time
A mixed-effects logistic regression model examining baseline patient characteristics, index substance abuse treatment completion, and time-varying covariates other than service use indicated that being female (OR=1.44, CI=1.08–1.92), being older (OR=1.02, CI=1.00–1.03), completing index substance abuse treatment (OR=2.72, CI=2.00–3.71), and being married or living as married (OR=1.38, CI=1.09–1.75) were positively associated with remission at follow-ups, whereas being employed at baseline (OR=.78, CI=.58–1.04) was marginally associated with nonremission at follow-ups (p<.10). Race-ethnicity, baseline household income, education, and dependence type were not associated with remission over time at the p<.10 level; thus they were not included in subsequent analyses. Having an alcohol ASI score above zero at the prior interview was negatively associated with remission over time (OR=.38, CI=.30–.49). We found no association between drug, medical, or psychiatric ASI composite scores at the prior interview and remission over time (data not shown).
Service use and remission over time
We next examined associations of substance abuse treatment readmission, psychiatric service use, and yearly primary care with remission over time by fitting a model that included covariates for each service use and its interaction with severity at prior time point, controlling for time and individual characteristics (
Table 3). Results suggest a significant interaction between lagged alcohol ASI score and substance abuse treatment readmission. Compared with participants with lagged alcohol ASI scores equal to zero and no substance abuse treatment readmission, participants with lagged alcohol ASI scores above zero but no readmission were 66% less likely to achieve remission, whereas those with lagged alcohol ASI scores above zero and who were readmitted to treatment were only 13% less likely to do so (OR=.34 and .87, respectively). Furthermore, having a yearly primary care visit was associated with remission over time: those with such visits had a 39% higher chance of achieving remission compared with those without such visits (OR=1.39, CI =1.11–1.75). Psychiatric problem severity at the prior interview seemed to moderate the associations between receiving psychiatric services and achieving remission from substance use problems at follow-ups: receiving psychiatric services was negatively associated with remission over time, whereas the interaction term of having lagged psychiatric ASI scores greater than zero and receiving psychiatric services was marginally positively associated with remission over time.
Continuing care and remission over time
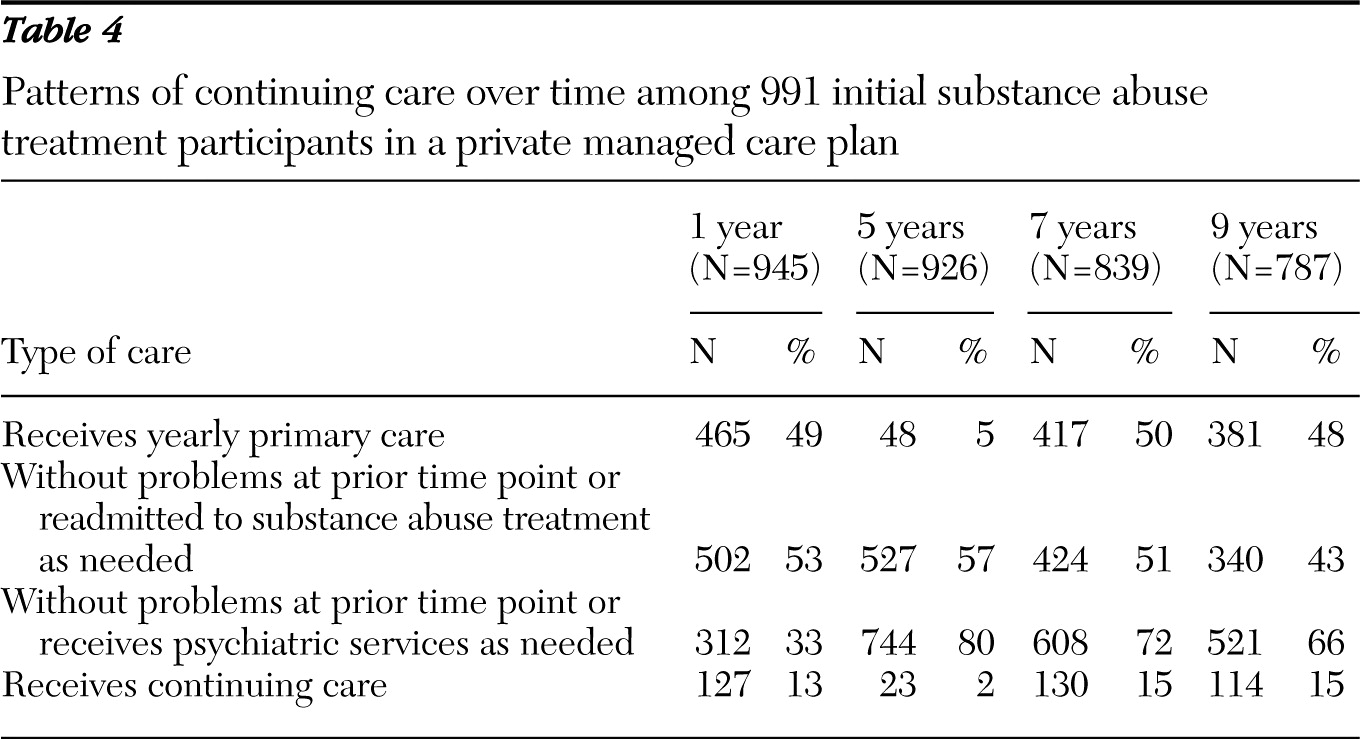
Our findings suggested a model of continuing care that included three components: regular primary care, substance abuse treatment as needed, and psychiatric services as needed. We next examined an operational definition of receiving continuing care at each follow-up, defined as having at least one yearly primary care visit; in year 1, completing index substance abuse treatment or not completing it but being readmitted, and after year 1, having both alcohol and drug ASI scores equal to zero at the prior interview or having alcohol or drug ASI scores above zero at the prior interview and having readmissions; and having psychiatric ASI scores equal to zero at the prior interview or having psychiatric ASI scores above zero at the prior interview and having psychiatric visits. On the basis of our definition, 15% or less had continuing care at one, five, seven, and nine years (
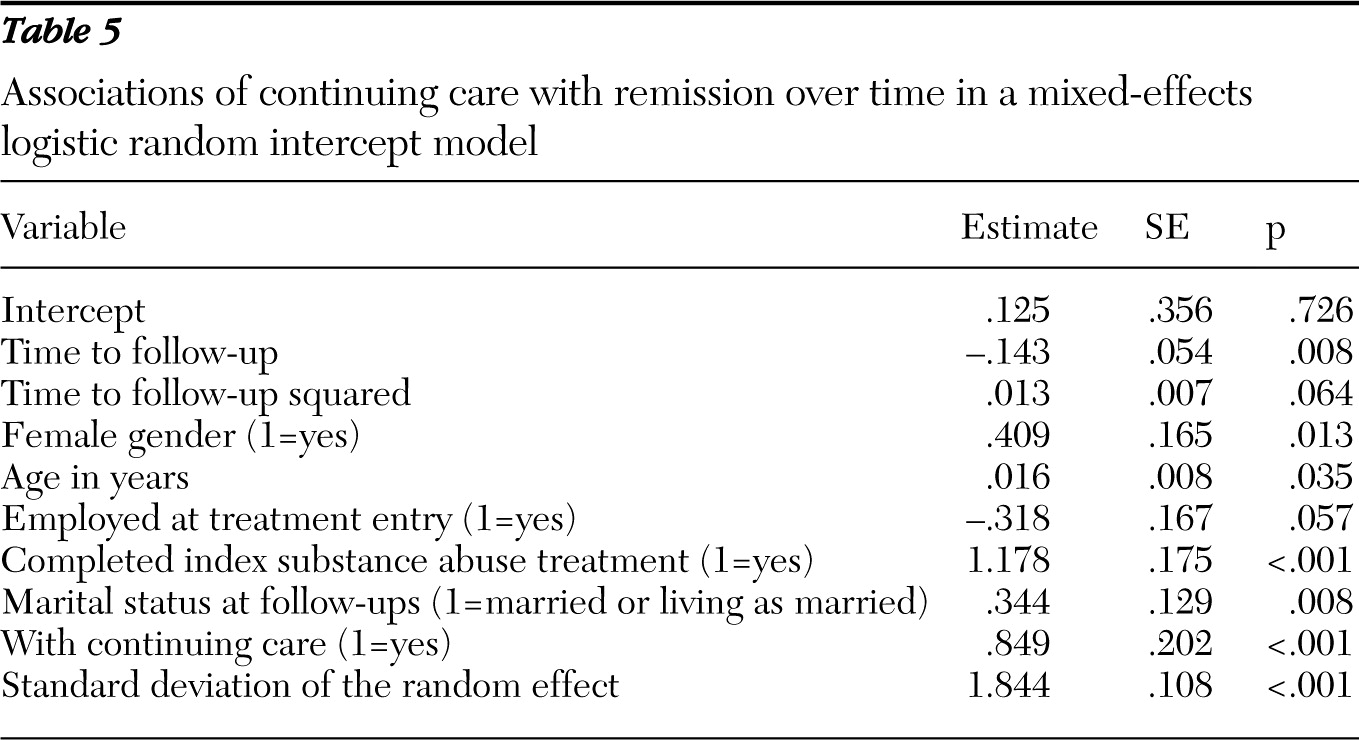
Table 4). A mixed-effects logistic regression model controlling for other covariates found that participants with continuing care were more than twice as likely to have achieved remission at follow-ups as those without continuing care (OR=2.34, CI=1.57–3.47) (
Table 5).
Discussion
This study found that having yearly primary care and specialty care (substance abuse treatment and psychiatric services) when needed was associated with remission over nine years for substance use patients in a private, nonprofit, integrated managed care health plan. Results reinforced primary care's key role in a continuing care approach to maintaining long-term outcomes for substance use patients, which is consistent with the model of primary care as an anchoring “health home” for the general population. Furthermore, our findings contribute empirically in showing that receiving yearly primary care is associated with better longitudinal outcomes. Post hoc analyses found that having at least one primary care visit every other year was only marginally associated with remission over nine years, indicating that frequency of visits is important. The mechanisms for the associations between yearly primary care and long-term remission remain to be examined. Those with yearly primary care may be more motivated or have better self-management skills; they may be healthier from being more likely to have medical needs addressed, which, in turn, helps their remission status; or yearly visits may provide opportunities to have a crisis or relapse identified and treated or referred. These questions are beyond the scope of this article but should be further examined.
One common confounder for longitudinal evaluation of intervention effectiveness on deviant behaviors is natural maturation. We conducted post hoc analyses to examine whether having “matured” into the next age category (defined by decade), compared with the prior time point, would confound the study results. Stratified cross-sectional bivariate analyses found that maturation was positively associated with past 30-day remission only for those aged 18–29 at one year (remission rate=95% versus 59%; χ2=9.03, df=1, p<.01), not for other age groups or at later waves. A mixed-effects logistic regression model of those under 30 at baseline found no significant maturation effects over time, whereas continuing care remained a significant predictor. Findings rule out the effect of natural maturation for this study.
Although few had substance abuse treatment readmissions after the first year, those who did when problems were present at the prior interview had better outcomes than their counterparts. A higher proportion of our sample had psychiatric services than had readmissions to substance abuse treatment during follow-ups. However, receiving psychiatric services was inversely related to remission, with a possible moderating effect of the lagged psychiatric severity. The relationship between psychiatric and substance use severity and the effects of psychiatric services use on this relationship have not been adequately studied. Prior research has found that receiving psychiatric services during or after substance abuse treatment (
27,
32,
33) is predictive of positive long-term outcomes. Furthermore, the high prevalence of psychiatric comorbidity among substance use patients suggests that receiving psychiatric services when needed should be considered a key component in a continuing care model.
Our definition of “in remission” is consistent with the literature (
13,
29,
30,
34–
36). We note that, across time points, most individuals who achieved remission were in total abstinence (91%, 87%, 85%, and 85% at one-, five-, seven-, and nine-year follow-ups, respectively). Therefore, the sample size for the nonabstinent, nonproblematic use group for each period was fairly small. Nevertheless, we conducted analyses that distinguished between remitted individuals who were abstinent and nonproblematic users and found that, at follow-ups, the nonproblematic users were not significantly different from total abstainers, whereas problem users were doing significantly worse than the other two groups. We also conducted nonlinear mixed-effects logistic regression analyses examining abstinence as the outcome and found that our measure of continuing care was significantly associated with alcohol, drug, and total abstinence at follow-ups over nine years, adjusting for the same set of covariates (abstinence from alcohol, OR=1.74, CI=1.20–2.52; abstinence from drugs, OR=1.83, CI=1.02–3.29; and total abstinence, OR=1.74, CI=1.21–2.49, respectively). These analyses support the validity of our measure of remission and the robustness of the findings on continuing care in maintaining long-term recovery.
Our continuing care model is consistent with the chronic care model, a frequently advocated chronic illness management framework (
37) that has been adapted to self-management office-based programs for several chronic illnesses and that has been shown to improve health outcomes, including for patients with mood disorders such as depression (
38). Findings of this study suggest long-term beneficial effects of adapting such a model for continuing care of individuals with substance use disorders. However, few substance use patients received continuing care, despite its benefits. This is of concern in a health system that provides primary care and specialty services internally. Other research in private and public systems has found that individuals with substance use disorders are more likely to use emergency and urgent care services than regular primary care (
39–
41; Parthasarathy S, Chi FW, Mertens JR, et al., unpublished manuscript, 2011). This calls for interventions that link patients to primary care and motivate them to appropriately use health care. Too often, substance use patients are seen as “belonging” to substance abuse treatment programs, and they themselves perhaps are insufficiently aware of their other health needs. The separation of behavioral health from medical practice may also contribute to a pattern of patients' being engaged in specialty treatment with no medical component (
42). This is an area for future research.
This study had several limitations. First, the sample was drawn from a private, integrated managed care health plan, and we selected those with health insurance over 60% of the observation period. Thus findings may not be generalizable to other health plans or public populations. However, this population may be more similar to the general population after health reform. Second, follow-up data were observational, and continuing care services were not randomized. Measures of some potential confounders, such as motivation, were not available across interview waves. However, a randomized comparison of a continuing care condition to a no-continuing care condition on long-term outcomes would be costly to conduct, and when continuing care is the normal standard of care, a randomized study would be unethical. Findings from our observational data may help stimulate future research and interventions. Third, although a key advantage of the mixed-effects modeling approach is that it can be applied when participants are not measured at the same number of time points, some fraction of participants might be missing because they were not remitted. We repeated the analyses presented in
Tables 3 and
5 with missing outcomes recoded as nonremission (
43) and found similar results, which suggests the robustness of the findings.
Acknowledgments and disclosures
This study was supported by grant RO1AA010359 from the National Institute on Alcohol Abuse and Alcoholism and grants R37DA10572 and R01DA08728 from the National Institute on Drug Abuse. The authors thank Donald Hedeker, Ph.D., and Kevin L. Delucchi, Ph.D., for statistical assistance, Joe Selby, M.D., M.P.H., for his review of the manuscript, and Agatha Hinman, B.A., for editorial assistance.
The authors report no competing interests.