The limited research on use of mental health services by bereaved individuals suggests that they often do not access available services despite sometimes experiencing intense psychological suffering (
1,
2). Systematic reviews and meta-analyses of grief intervention studies have shown that treatments targeting high-risk or symptomatic individuals demonstrate stronger effects (
3).
To help identify individuals exhibiting persistent grief reactions, researchers have validated diagnostic criteria for a proposed clinical syndrome called prolonged grief disorder. Although it has not been recognized as a distinct disorder in published editions of the
DSM, there is growing evidence that prolonged grief disorder is a unique condition characterized by separation distress and other symptoms, such as intense, unremitting yearning for the deceased, difficulty accepting the loss, and sense of meaninglessness, that remain elevated at six or more months after the loss (
4). Although prolonged grief disorder may be comorbid with other psychiatric disorders, its symptoms have been associated with negative physical and mental health outcomes (
4), including poorer quality of life (
5) and suicidality, independent of depression (
6).
Despite the potential benefits of mental health services for bereaved individuals, including those with prolonged grief disorder, few studies have examined their use by this population. Use of such services by bereaved individuals has ranged from as little as 2% to 30% (
1,
2,
7), depending on the samples, the type of service used, and the relationship of individuals to the deceased. Mental health service use after bereavement may have enduring and broad positive effects, including the potential to counter adverse health consequences, such as premature mortality, that have been associated with the loss of a loved one (
8).
Given the limited research on mental health service use among the bereaved, and particularly among caregivers who meet criteria for prolonged grief disorder, this longitudinal study had four aims. They were to determine the incidence of prolonged grief disorder and its associations with morbidity (suicidality and poorer heath-related quality of life) among bereaved caregivers of advanced cancer patients, to characterize patterns of mental health service use among the bereaved with and without prolonged grief disorder, to identify reasons why bereaved individuals might choose not to use mental health services, and to identify and compare predictors of mental health service use among caregivers with prolonged grief disorder and those with other psychiatric disorders.
Methods
Participants were bereaved caregivers of patients with advanced cancer who were recruited as part of the Coping with Cancer Study, a multi-institutional, longitudinal evaluation of mental health of advanced cancer patients and their primary informal caregivers that was funded by the National Institutes of Health. This study focused on ad hoc analyses of data obtained from caregivers at baseline, which was conducted a median of 3.1 months before the patient's death, and at follow-up, a median of 6.6 months after the patient had died (
9).
Participating patient-caregiver dyads were selected on the basis of patient eligibility. Patients were eligible if they had a diagnosis of advanced cancer, had adequate stamina to complete an interview, were age 20 years or older, and could identify an unpaid, informal caregiver of at least 20 years of age who provided most of the patient's unpaid, informal care, regardless of living arrangement or number of hours per week care in which was provided. All study protocol documents were approved by the human subjects committee at each participating site. After receiving a complete description of the study, participants' written informed consent was obtained. [An online appendix with supplementary recruitment information is available at
ps.psychiatryonline.org.]
Caregivers provided detailed demographic information at baseline. The Structured Clinical Interview for the DSM-IV Axis I Disorders (SCID-I) (
10) was used by highly trained interviewers (
κ>.90 with expert rater) to determine the presence of major depressive disorder, generalized anxiety disorder, panic disorder, and posttraumatic stress disorder at baseline and six-month follow-up. We assessed caregivers' grief at baseline using a modified version of the PG-13, a rater-administered measure of prolonged grief disorder symptoms (
4). The predeath version has been used in prior studies of caregivers and assesses severity of grief as it relates to aspects of the patient's illness, such as loss of health and normal functioning, but does not assess symptom duration (
11).
Prolonged grief disorder was assessed at follow-up with the rater-administered PG-13 on the basis of diagnostic criteria outlined by Prigerson and others (
4), which have demonstrated internal consistency (Cronbach's
α=.82) and incremental validity. The Yale Evaluation of Suicidality (YES), a 16-item valid and reliable self-report measure, was used to assess suicidality (for example, the wish to live or die and the presence of suicidal ideation, plan, and intention) at follow-up (
6). Possible scores range from 0 to 16. Because scores in this sample were highly skewed toward no suicidality (score of 0) a dichotomous variable was created by using a median split (median=0) (
6). A score of 1 was assigned to caregivers with YES scores >1 (median 3, range 1–10) to indicate the presence of suicidal thoughts or gestures.
The well-validated Medical Outcomes Study 36-Item Short Form (SF-36) has eight subscales to measure physical functioning, physical health-related role limitations, bodily pain, general health perceptions, vitality or energy level, social functioning, emotional health-related role limitations, and mental health and was used to assess health-related quality of life (
12). We also examined health changes in the past year and four different summary scores—a physical component summary, a mental component summary, a summary in which each of the eight scales was weighted equally (summary score 8), and another in which each item was weighted equally (summary score 36). Scores are standardized and range from 0 to 100, with lower scores reflecting poorer outcomes (
12).
Mental health service use was assessed at baseline and follow-up (
9). Discussions about mental health concerns with the patient's oncologist or other health care professionals were differentiated from use of mental health services, which was defined as accessing any type of mental health intervention, such as psychotherapy, psychotropic medications, hospitalization, support groups, and counseling with a member of the clergy.
Characteristics of participants were determined with descriptive statistics. Differences in rates of suicidality and mental health service use among caregivers with different psychiatric disorders were examined with chi square or Fisher's exact test statistics. We evaluated differences in health-related quality of life using t tests. Logistic regression models were conducted to determine associations between access to mental health services following the patient's death and other background variables. Variables that were significantly associated with mental health service access at the p<.05 level and that were of conceptual interest, such as the presence of prolonged grief disorder, were included in the adjusted analyses. Data were analyzed with the SAS System for Windows, version 9.2, with two-tailed statistical tests.
Results
A total of 927 patients met initial screening criteria, and 287 (31%) declined participation. Only bereaved caregivers with prolonged grief disorder were included in this ad hoc study. After exclusion of 99 bereaved caregivers for whom prolonged grief disorder data were unavailable and 11 caregivers whose loved one had died fewer than six months earlier, the final sample included 86 participants. Differences between bereaved caregivers with and without data about prolonged grief disorder data can be found in the online appendix.
Participating caregivers were primarily spouses or partners (N=38, 46%) or offspring (N=21, 25%). A majority were female (N=72, 84%), white (N=47, 55%), and married (N=49, 57%). SCID-I results for 76 participants found 11 met criteria for major depressive disorder (13%), six for posttraumatic stress disorder (7%), and three for panic disorder (4%); two of 75 participants assessed met criteria for generalized anxiety disorder (2%). Overall, 19% of the 76 participants assessed met criteria for at least one diagnosis on the basis of the SCID-I. The online appendix describes other participant characteristics.
Sixteen percent (N=14) of the sample met criteria for prolonged grief disorder a median of 6.6 months after the death of the patient. An identical percentage registered the most severe grief symptoms at baseline on the modified PG-13. Caregiver grief before the patient's death was significantly associated with the presence of prolonged grief disorder (odds ratio [OR]=6.00; 95% confidence interval [CI]=1.65–21.77, p=.006). Bereaved caregivers with prolonged grief disorder were also more likely to also meet criteria for major depressive disorder or generalized anxiety disorder (p<.002). Interestingly, they were not more likely to meet criteria for posttraumatic stress disorder or panic disorder.
The presence of prolonged grief disorder was associated with several negative outcomes, including suicidality (χ2=5.03, df=1, p=.025). Ten of the 14 (71%) bereaved caregivers with prolonged grief disorder reported suicidal thoughts or gestures. Caregivers with prolonged grief disorder also had significantly poorer overall health-related quality of life (t=2.52, df=81, p=.014) compared with other caregivers. Specifically, they reported poorer mental health (t=5.21, df=83, p<.001), lower levels of social functioning (t=2.95, df=84, p=.004), more limitations because of emotional problems (t=2.31, df=84, p=.024), and lower energy (t=2.02, df=83, p=.046). Additional health-related quality-of-life data are reported in the online appendix.
Of the 86 caregivers in this study, 19 (22%) discussed emotional concerns with a professional prior to the patient's cancer diagnosis, 29 (34%) discussed them after the patient's diagnosis, and 38 (44%) discussed them after the patient's death. Twenty-three caregivers (27%) reported use of mental health services during the patient's illness, and 34 (40%) reported mental health service use after the patients' death.
Of the bereaved caregivers with prolonged grief disorder, seven (50%) discussed emotional concerns with a professional following their loss, and six (43%) reported mental health service use. Five of the ten (50%) caregivers with prolonged grief disorder and suicidality accessed services. The presence of prolonged grief disorder was not associated with either discussions with a professional about emotional concerns or mental health service use after the patients' death.
Whereas less than half of bereaved caregivers with prolonged grief disorder reported mental health service use, ten caregivers (63%) who met criteria for major depressive disorder, generalized anxiety disorder, panic disorder, or posttraumatic stress disorder used services. (The online appendix summarizes use of services by diagnosis.) The presence of a comorbid mental disorder and prolonged grief disorder was not significantly associated with use of mental health services.
Not having mental health concerns was the most common reason provided for not using mental health services, reported by 25 of the 49 (51%) bereaved caregivers whose responses were available. Other reasons included having family, friends, or church support (N=7, 14%); financial constraints (N=4, 8%); and not having time (N=2, 4%). Eleven caregivers (22%) provided other reasons, including not being aware of specialized bereavement services, not believing mental health treatment is effective, not knowing whom to contact, not feeling ready, not feeling that it was needed, and feeling too embarrassed.
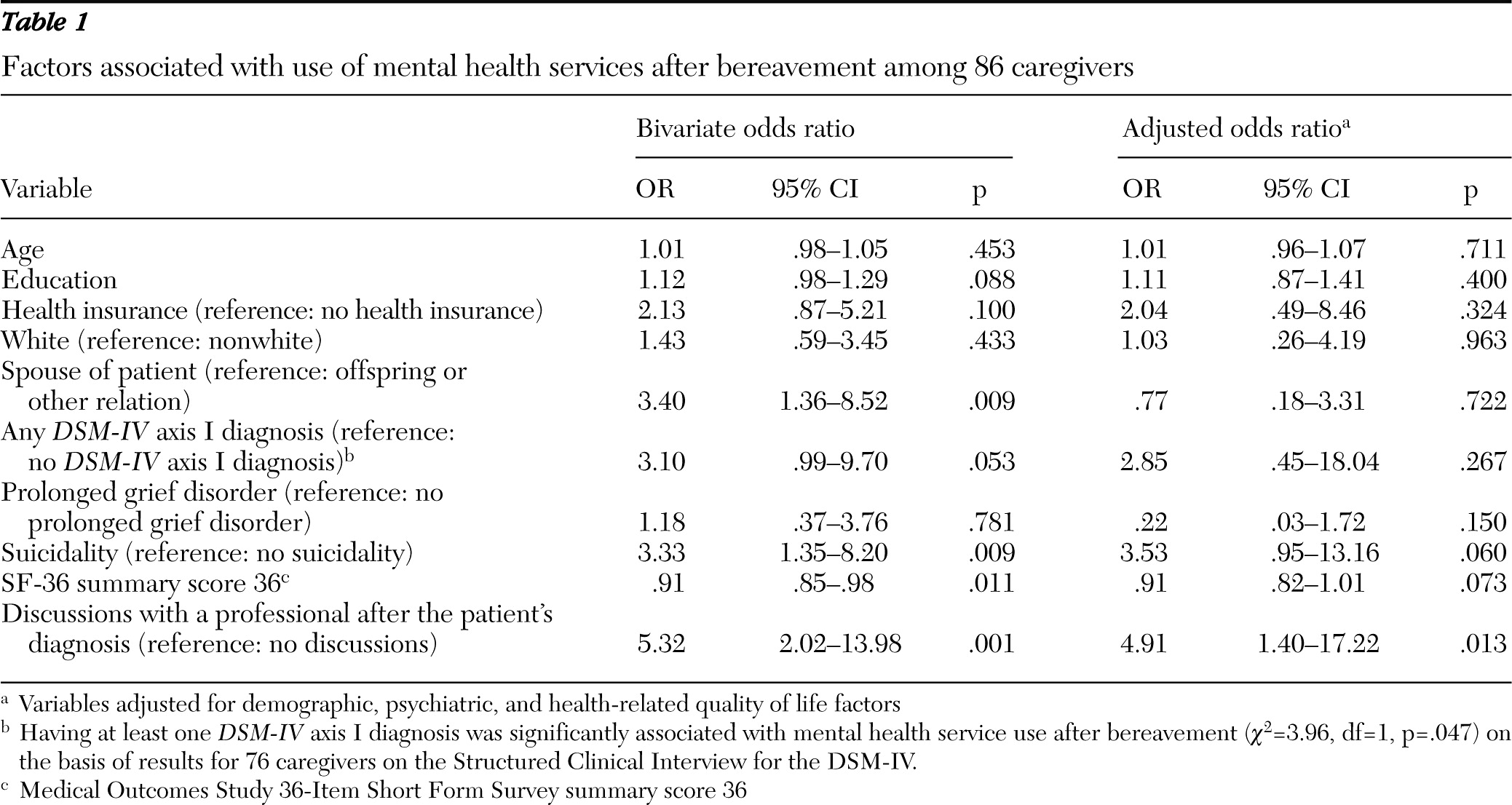
Table 1 shows factors associated with use of mental health services among bereaved caregivers in both unadjusted and adjusted analyses. Several variables were significantly associated with service use in unadjusted analyses, but only one—discussing psychological concerns with a professional after the patients' cancer diagnosis but before their death—remained a significant predictor upon adjusted analysis (OR=4.91, CI=1.40–17.22).
Discussion
Although a few previous studies have examined mental health service use by the bereaved (
1,
2,
7,
8), research on individuals with prolonged grief disorder is limited. We observed that only 43% of caregivers who met criteria for prolonged grief disorder accessed mental health services, compared with 63% of those who met criteria for major depressive disorder, generalized anxiety disorder, posttraumatic stress disorder, or panic disorder.
Despite experiencing symptoms of prolonged grief disorder and the negative correlates associated with them, such as suicidality and poorer health-related quality of life, these caregivers were no more likely to access services than caregivers without prolonged grief disorder. This pattern is troubling in light of our finding confirming a relationship between prolonged grief disorder and suicidality, which was consistent with other studies that have found that prolonged grief disorder is associated with suicidality independent of depression (
6).
Several explanations exist for the underutilization of mental health services by caregivers with prolonged grief disorder. Perhaps individuals who met criteria for an established diagnosable disorder were more likely to recognize their own symptoms and seek professional assistance. It may also be that personal or professional sources of support recognized the symptoms of established mental disorders and encouraged survivors to seek help but discounted or dismissed grief-specific distress. Also, members of bereaved caregivers' support systems may have considered grief symptoms part of a normal reaction to loss and may not have understood that mental health interventions were warranted.
Yet when participants in the Yale Bereavement Study were asked their feelings about a prolonged grief disorder diagnosis, more than 90% of those with the disorder reported that they would be relieved to know that it was a recognizable psychiatric condition, and all reported an interest in receiving treatment for symptoms of severe grief (
13).
We observed that caregivers who discussed mental health concerns after a patient's cancer diagnosis were nearly five times more likely to access mental health services after bereavement. The period after diagnosis presents an opportunity to integrate vulnerable patients and caregivers into the mental health care system to facilitate continuity of care. As disease progresses, interventions can be particularly important for caregivers struggling with death acceptance, given that a lack of preparedness for death has been associated with the development of prolonged grief disorder (
4).
Interventions that begin while the patient is still alive and facilitate preparedness for the patient's death can have a prophylactic effect and prevent negative bereavement outcomes (
14). Our finding that intense grief experienced before the patient dies predicts prolonged grief disorder suggests that connection with mental health providers during the caregiving phase may be especially important for caregivers exhibiting severe grief symptoms before the patient's death.
The reason reported most commonly by bereaved caregivers for not accessing mental health services was a belief that they did not need help, a finding similar to those of Cherlin and others (
3). For the subset of bereaved caregivers at increased risk of suicide, their prolonged, intense grief may contribute to their view that professional providers cannot help. These individuals may not recognize when reactions are abnormal nor know whom to contact for assistance. Outreach and treatment by providers may be affected by their beliefs about whether pathological grief reactions can develop; clinicians with concerns about overpathologizing grief may be hesitant to recommend mental health interventions for bereaved individuals because they consider grief normal.
Implementation of a standardized risk assessment as part of palliative care programs could help identify those individuals who might gain from psychological assistance but who may not be aware of their maladaptive symptoms or may be avoiding available professional support because of fear about confronting the pain of their loss or stigma (
1,
13). Bereaved individuals and members of their support systems may not realize that prolonged grief can be pathological and that specialized treatments that target prolonged grief disorder have benefits (
4,
15).
Although this study did not directly examine the benefits of bereavement mental health services, caregivers were asked to rate the helpfulness of the interventions they accessed. Of the 37 caregivers who responded, 36 (97%) rated the bereavement interventions as moderately or very helpful. Despite the potential efficacy of available interventions, this study highlighted that they are not commonly utilized by persons who are suffering from persistent, dysfunctional grief.
This study was limited by the relatively small sample size, which influenced the incidence of the mental disorders assessed and increased the risk of a type 2 error in the associations examined. The incidence rate of prolonged grief disorder we observed, however, was consistent with rates found in prior studies (
4). Patients who declined to participate in the study were more distressed than those who participated, raising the possibility of underrecognition of prolonged grief disorder among their caregivers. Because bereaved caregivers who were not included in the analysis were less likely to use mental health services, as indicated in the online appendix, underutilization of these services among bereaved caregivers may be greater than our findings suggest.
Conclusions
Bereaved caregivers with prolonged grief disorder appear to underutilize mental health services despite their protracted and distressing symptoms. These results should not imply that mental health services are needed in every case; to the contrary, research suggests that grief interventions are most efficacious among high-risk or psychiatrically symptomatic individuals (
3,
14,
15). Most bereaved are not in need of mental health services, but as these data show, those who meet criteria for prolonged grief disorder are in need of services and may find them helpful.
Recognizing that grief can be pathological will require an important paradigm shift in how bereaved individuals are clinically perceived and treated. However, we caution against interpreting these findings as evidence supporting the removal of the bereavement exclusion criterion for major depressive disorder in the fifth edition of the DSM. The bereavement exclusion criterion targets individuals who have been bereaved in the past two months. Participants in this study had been bereaved for at least six months; thus the data did not address the costs or benefits of removing the current exclusion criterion for bereavement.
Future studies should assess a larger cohort of bereaved caregivers at time points later in the bereavement trajectory to determine why some patients with diagnosable prolonged grief disorder or a DSM-IV axis I diagnosis do not seek treatment. Researchers could also focus on ways to promote discussions with clinicians before the patient's death. Studies to assess psychosocial and clinical barriers to use of mental health services after bereavement, the clinical utility of a prolonged grief disorder diagnosis for effective detection and treatment of distressed bereaved individuals, and ways to improve outreach and increase uptake of services for those in greatest need are also important. Finally, researchers should conduct longitudinal intervention studies to determine whether various grief treatments can reduce the prevalence of bereavement-related psychiatric disorders, including prolonged grief disorder, and can specifically address suicidality.
Acknowledgments and disclosures
This research was supported in part by National Institute of Mental Health grant MH63892; National Cancer Institute grants CA106370, CA139944, and CA156732; and the Center for Psycho-Oncology and Palliative Care Research, Dana-Farber Cancer Institute, Boston.
The authors report no competing interests.