Although institutional measures of control, such as seclusion and restraint, may seem justified at times, there is growing consensus that such practices are potentially countertherapeutic and may be unnecessary (
1–
6). Such concerns are heightened by data indicating that people with serious mental illness experience higher rates of sexual and physical assault and posttraumatic stress disorder, compared with the general population (
4,
7–
14). Furthermore, exposure to traumatic events among patients with serious mental illness is strongly correlated with severity of psychiatric difficulties (
10,
15). Together, these data suggest that patients with serious mental illness may be susceptible to adverse consequences of institutional measures of control (
16).
To improve the therapeutic climate of inpatient psychiatric settings, the Substance Abuse and Mental Health Services Administration (
17,
18), National Association of State Mental Health Program Directors (NASMHPD) (
16,
19), several state mental health departments (
20), and others (
1,
21,
22) have called for the elimination or reduction of seclusion and restraint via legislative efforts and reconsideration of administrative policies. It is encouraging that data gathered by the NASMHPD Research Institute from more than 200 psychiatric facilities between January 2000 and December 2004 showed a 16% reduction in the use of restraint (400 fewer patients per month) and a 45% reduction in the use of seclusion (1,000 fewer patients per month) over that period (
19). These data also demonstrated a 50% reduction in the total number of hours patients were held in restraint (26,000 fewer hours per month) and an 18% decrease in the number of hours patients were held in seclusion (3,000 fewer hours per month).
The effect of specific behavioral interventions on subsequent rates of seclusion and restraint has been examined in other studies (
23–
27) and in a review (
28). Common features of these behavioral efforts include changes in leadership, close monitoring of use of seclusion, staff education, and changes to the therapeutic setting. The findings suggest that it is possible to reduce the use of both seclusion and restraint (
23–
28) and that there are economic benefits to doing so (
29). However, none of the studies cited here included an experimental design, and the lack of experimental studies limits the ability to make conclusions about causality.
To our knowledge, there has not been a rigorous assessment of programmatic efforts to reduce use of seclusion and restraint in psychiatric hospitals. Specifically missing are effectiveness studies that incorporate the use of control groups or cluster-randomized, case-control, and time-series designs. As noted elsewhere (
28,
30,
31), efforts thus far have failed to incorporate methodological designs that will allow for meaningful inferences regarding the effects of specific behavioral interventions on outcomes. In addition, previous studies have often used a combination of behavioral strategies, making it unclear which component or components of the intervention affected subsequent rates of seclusion and restraint.
Previously, we proposed a strategy for measuring change related to the implementation of a multiphase intervention by using a multiple-baseline time-series design (
32,
33). We chose this approach for the study reported here because it represents a cost-efficient method that allows inferences about the program's effectiveness over and above nonspecific effects (such as time, seasonal variation, or effects associated with observation of patient and staff behaviors) and permits systematic evaluation of the effectiveness of various components of the intervention. To our knowledge, this study is the first to incorporate an experimental research design that allows for preliminary inferences about causality and identification of the intervention components that had the most impact on use of seclusion and restraint. These data are timely given recent national initiatives to reduce use of seclusion and restraint and to improve the climate of care for individuals with serious mental illness.
Methods
Design
Using a variant of the multiple-baseline design, we implemented the engagement model (an adaptation from the work of Bloom [
1]) in a psychiatric inpatient setting over a 3.5-year period (a total of 89,783 patient-days) in a manner that would be conducive to replication in other hospitals. A variant of the multiple-baseline design was chosen because it allowed for randomized assignment of interventions across inpatient units and the ability to control for the effects of time, implementation order, and institutional “placebo” effects, such as observation effects, and other nonspecific effects, such as the unit administration's commitment to change. The 3.5-year study period consisted of a baseline phase from January 2005 through February 2006, an implementation phase from March 2006 through March 2008, and a follow-up period from April 2008 through June 2008.
The engagement model includes four separate components: trauma-informed care training, changes in rules and language, patient involvement in treatment planning, and changes to the physical characteristics of the therapeutic environment. Included in the study were five inpatient units at one psychiatric hospital: a high-acuity adult unit, a geriatric unit, a general adult unit, a substance abuse unit, and a child and adolescent unit. The implementation schedule for the components of the model was established such that each unit was assigned to implement the components in a different order (randomly determined).
In addition, during the study period, the hospital implemented an ongoing, larger organizational initiative to improve patient satisfaction and patient-staff communication. This initiative was termed AIDET, which consisted of a policy that instructed all clinical staff to engage in the following communication behaviors with inpatients: “Acknowledge” patients, “Introduce” themselves, articulate the anticipated “Duration” of the clinical contact, “Explain” the reason for the contact, and “Thank” patients for their cooperation. The AIDET initiative was integrated into the engagement model implementation schedule such that its impact on the seclusion and restraint rate could be evaluated.
Last, each unit was assigned two separate implementation periods dedicated to making changes to the physical characteristics of the therapeutic environment. Each unit served as its own control from intervention to intervention. Because each unit implemented the same interventions over time but in a different order, unique effects for each intervention could be examined between units over time, with control for primary competing explanations for effects. For example, the rules and language intervention could be implemented at different times on different units during the two-year implementation period. If this intervention was found to be uniquely associated with significant reductions in the rate of seclusion and restraint over and above other interventions each time and place it was implemented (that is, independent of when it was implemented and independent of where it was implemented), one could reasonably conclude that this intervention was uniquely associated with changes in use of seclusion and restraint over and above effects of time, intervention order, and location. To the extent that time effects, order effects, and location effects are the primary competing explanations for any observed effects, this research design allowed us to begin to make inferences of causality.
Institutional review board approval was obtained to collect and publish patient and staff ratings regarding the quality of care. Institutional review board approval was also obtained to publish all findings regarding seclusion and restraint rates, inpatient unit acuity measures, and length-of-stay data.
Dependent measure
The rate of seclusion and restraint was calculated as the number of seclusion or restraint incidents per patient day for each unit and each period of the implementation schedule. This information is routinely collected and tracked in accordance with The Joint Commission's quality and safety standards and is maintained in internal databases at the study site.
Interventions
The activities associated with the engagement model components (trauma-informed care, rules and language, therapeutic environment, and patient involvement in treatment planning) were organized and operationalized to be as uniform as possible between the diverse inpatient units. Each phase of the implementation schedule was three months in duration.
For trauma-informed care, all unit staff attended a half-day standardized training seminar on the nature of trauma and its effects on patients' experiences, physiology, and psychological processes, along with instructions on how to minimize engaging in behaviors that could exacerbate trauma-related reactions from patients.
For rules and language, all unit staff attended a standardized training seminar on the effect of rules and language on patients' perceptions. The rules and language intervention included the establishment of a team for each unit that was tasked with reviewing and modifying unit rules and policies to be less restrictive to patients or eliminating unit rules that were too restrictive. All unit staff attended a follow-up half-day seminar during which the rule changes were articulated and the effect of coercive language on patients' experiences was discussed. All signs on the units were reviewed and revised as necessary to ensure that they reflected the new, less restrictive rules and used noncoercive language.
The therapeutic environment intervention involved making inexpensive physical changes, including repainting walls with warm colors, placement of decorative throw rugs and plants, and rearrangement of furniture to facilitate increased patient-patient and patient-staff interaction, as well as holding staff-patient group meetings regularly on the unit. Two separate therapeutic environment interventions were allotted to each unit. The second intervention included replacing worn-out furniture and continuing with environmental changes initiated during the first intervention.
For patient involvement in treatment planning, all unit staff attended a half-day standardized training seminar on the rationale for and clinical benefits of involving patients in the treatment planning process.
Measures of intervention effectiveness
The patient form and staff form of the Quality of Care (QOC) measure (see Danielson and associates [
33] for details and psychometric information) were used to measure three factors of quality of care: perceptions of the physical environment, trauma sensitivity of the staff, and involvement of the patient in treatment planning. The patient and staff forms of the QOC have demonstrated good internal consistency reliability (Cronbach's alpha coefficients of .87 and .89, respectively), as well as strong correlations between the three theoretical and empirical factors (
33). The measures were taken before and after each phase of the intervention rollout. To assess intervention validity, we evaluated changes in patients' and staff members' perceptions of the environment before and after implementation of the therapeutic environment interventions, changes in trauma sensitivity ratings before and after implementation of the trauma-informed care and rules and language interventions, and changes in ratings of involvement in treatment planning before and after the intervention to improve patient involvement in treatment planning.
Observation phase
Given previous findings suggesting that managerial commitment to reducing seclusion and restraint on psychiatric inpatient units is associated with a substantial change in seclusion and restraint use (
23–
29), we included an observation-only phase at the beginning of the implementation schedule. For most of the units, this observation-only period was extended into the second phase of the implementation schedule before full randomization of the order of interventions across units. This procedure was used to ensure that we could carefully control for effects associated with observation of the process over time, management and staff commitment to reducing seclusion and restraint, and regular and timely feedback about institutional seclusion and restraint usage. The observation phase, coupled with the randomization scheme, was intended to provide robust experimental control in the real-world clinical setting of the intervention trial.
Acuity measures
The mean±SD length of stay and mean illness severity rating were determined for each phase of the implementation schedule by using the University Healthcare Consortium (UHC) database. For each inpatient discharge, an illness severity rating is assigned by UHC on the basis of the patient's number of psychiatric and medical comorbidities. Each case in the system is categorized into one of the following illness severity classes: minor, moderate, major, and extreme. High values tend to be associated with patients who have problems that are difficult to treat and who have poor outcomes. The ratings are used only to characterize patients with conditions that are severe enough to warrant inpatient hospitalization. To quantify illness severity, we assigned a number to each category (minor=1, moderate=2, major=3, and extreme=4). Data on illness severity and length of stay were included in the statistical models to control for potential effects of variability in illness severity on use of seclusion and restraint.
Analyses
PROC MIXED in SAS, version 9.2 (
34), was used to examine the effects of the various interventions on rates of seclusion and restraint in the units over time. Each unit's monthly rate of seclusion and restraint served as the primary dependent measure (point of measurement as level 1) during the study period, and rates were permitted to cluster within unit over time (inpatient unit as subject ID). To satisfy the assumption of normality of the residuals of the fitted models, the natural logs of the rates were used and residuals of each model were examined for normality (Shapiro-Wilk's test). First, covariates (for example, acuity level, time, and mean length of stay) were entered as model predictors. Significant covariates were then carried forward into the main model, which was designed to assess the effects of the various stages of the intervention rollout on rates of seclusion and restraint over and above the significant covariates. Each intervention was entered into the model simultaneously, and each unit's intercept was entered as a random effect. Slopes for seclusion and restraint rate over time were also permitted to vary as random effects. The covariance matrix was first-order autoregressive, and the restricted maximum likelihood was used for estimation.
For each phase of the rollout and for each hospital unit, mean factor scores were calculated from the QOC questionnaires representing unit-level environmental ratings, trauma sensitivity ratings, and treatment plan involvement ratings. These values were used to examine the validity of the intervention. One-tailed, independent t tests were used to examine changes in key patient-reported factors before and after implementation of the intervention across all units. Although these patient-reported measures were obtained pre- and postintervention on each unit, the interventions were rolled out in three-month increments, and thus the patient samples on the units were different (independent) at the two time points. Paired-sample t tests were used to examine changes in staff members' QOC ratings before and after each stage of the rollout because the same staff members provided ratings at each time point.
Before evaluating the overall difference in mean seclusion and restraint rates between the baseline, preintervention phase (January 2005 through February 2006) and follow-up, postintervention phase (April 2008 through June 2008), the assumption of independence of observations was evaluated by examining the autocorrelation function of the monthly rate values across both phases. Given the small number of data points in the follow-up phase relative to baseline, nonparametric Wilcoxon's rank-sum test was used to examine the overall change in mean monthly rate from the baseline to the follow-up phase.
Unit staff and other model details
For more details on the research effort, including information on the unit staff composition, research design logic, and managerial perspectives on the engagement model initiative, see articles by Borckardt and colleagues (
32), Danielson and colleagues (
33), and Hardesty and colleagues (
35).
Results
Acuity measures
The mean±SD acuity score throughout the engagement model implementation period was 1.68±.06. The mean±SD length of stay during the period was 7.15±.24 days.
Intervention validity
A total of 446 patient QOC questionnaires were collected during the engagement study. Mean scores for each QOC factor, each rollout period, and each unit were calculated.
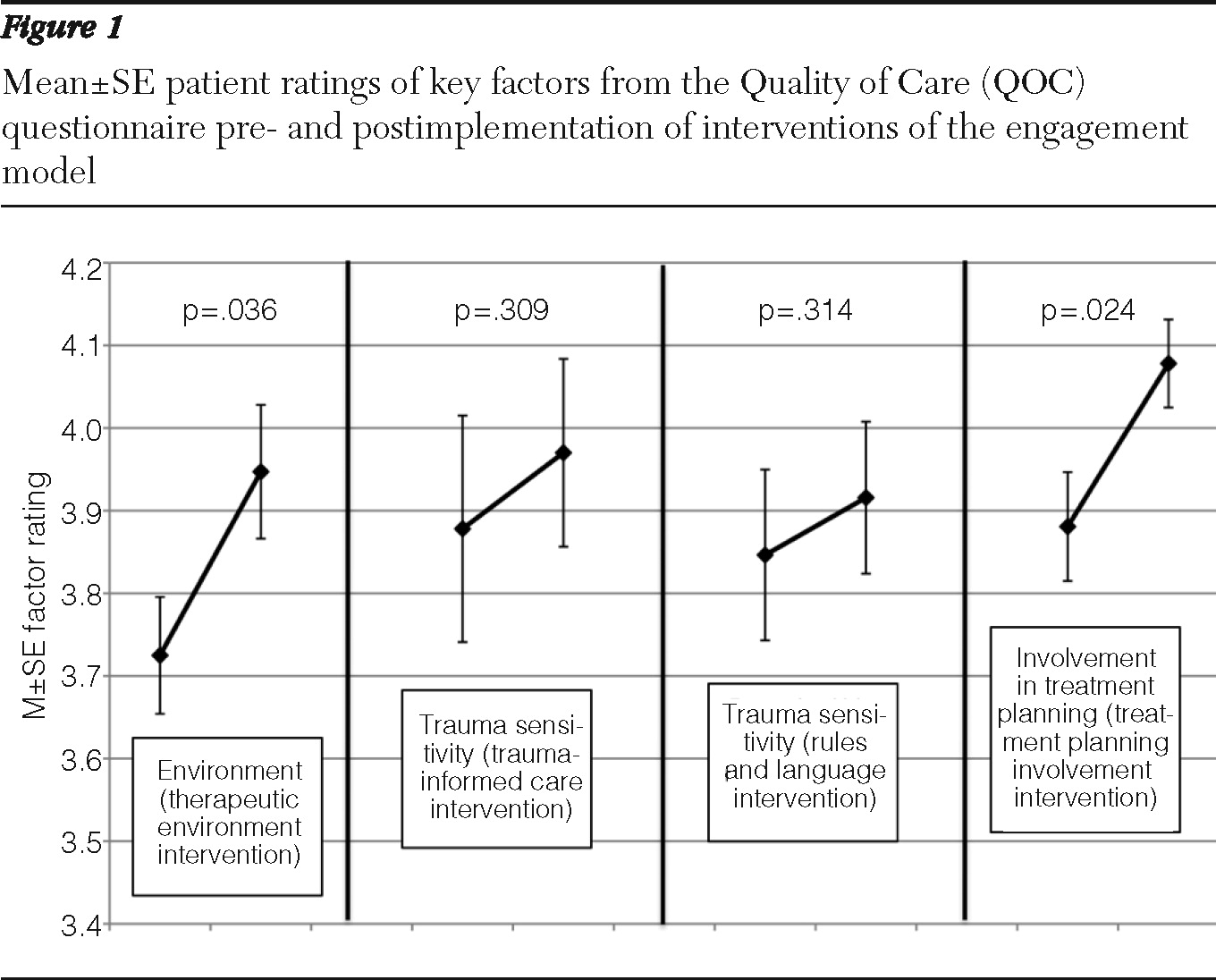
Figure 1 shows patient ratings of key factors from the QOC) questionnaire pre- and postimplementation. A significant increase in patients' average rating of the physical environment was observed from preintervention to postintervention for the first therapeutic environment intervention across the five inpatient units. The mean±SE rating was 3.72±.16 before the intervention and 3.94±.18 after the intervention (t=2.07, df=8, p=.04). This finding suggests that patients' perceptions of the pleasantness of the inpatient environment improved after the environmental interventions. A significant increase in patients' perceptions of their involvement in the treatment planning process was observed after interventions to improve patients' engagement in treatment planning. The mean±SE rating of their involvement was 3.88±.15 before the intervention and 4.08±.12 after the intervention (t=2.33, df=8, p=.02). No change was observed in patients' ratings of the trauma sensitivity of the staff before and after implementation of the trauma-informed care intervention. The preintervention mean rating was 3.88±.23, and the postintervention mean rating was 3.97±.25. In addition, no change was observed in ratings of trauma sensitivity before and after the rules and language intervention. The preintervention mean rating was 3.85±.23, and the postintervention mean rating was 3.92±.21.
A total of 340 staff QOC questionnaires were collected during the engagement study. Mean±SE scores for each QOC factor, each engagement rollout period, and each unit were calculated. No statistically significant changes were observed in staff members' QOC ratings after any intervention. The mean staff environment rating was 3.5±.41 before the therapeutic environment intervention and 3.78±.29 after the intervention. The mean rating of patient involvement in treatment planning was 3.75±.32 before the intervention to increase patient involvement in treatment planning and 3.92±.48 after the intervention. The mean staff trauma sensitivity rating was 4.25±.10 before the trauma-informed care intervention and 4.30±.08 after the intervention. The mean trauma sensitivity rating was 4.25±.13 before the trauma-informed care intervention and 4.22±.12 after the intervention.
Overall, these findings suggest that patients' ratings of the environment and their involvement in treatment planning increased significantly after interventions designed to affect these factors. All other intervention validity measures showed nonsignificant changes.
Effects of the model on rate of seclusion and restraint
During the study period, the frequency of incidents of seclusion far exceeded the frequency of incidents of restraint: 97% of incidents involved seclusion, and 3% involved the use of restraint. None of the lags from the autocorrelation function of the monthly rates during the baseline and follow-up phases were significantly different from zero, suggesting satisfaction of the assumption of independence of observations for comparing baseline to follow-up rates. The mean±SD seclusion and restraint rate during the baseline phase was .027±.018 per patient day, and the mean rate during the follow-up phase was .005±.002 per patient day. The entire engagement model initiative was associated with an 82.3% reduction in use of seclusion and restraint when the mean monthly rate during the baseline phase (January 2005 through February 2006) was compared with the mean monthly rate during the follow-up, postintervention phase (April 2008 through June 2008) (Wilcoxon=6.00, z=−2.65, p=.008).
The effects of acuity, length of stay, and time on log seclusion and restraint rate were evaluated, and the residuals of the fitted model were normal. Acuity was associated with significant variability in the rate of seclusion and restraint (F=9.33, df=1 and 127, p=.003), but time and length of stay were not.
Next, the effects of the engagement model interventions were examined. The residuals of the fitted model containing all of the engagement model component predictors, including the observation-only phase effect and the acuity covariate, were normal. After the analysis controlled for the effects of acuity and the observation-only phase effect, one intervention was uniquely associated with significant reductions in the rate of seclusion and restraint independent of when and where it was implemented in the schedule. The implementation of change to the physical characteristics of the therapeutic environment was associated with a significant reduction in use of seclusion and restraint (F=7.94, df=1 and 119, p=.006). None of the other interventions of the engagement model were uniquely and significantly associated with a reduction in use of seclusion and restraint [A figure showing the rates of seclusion and restraint over time on the various units is presented in an online appendix to this article at
ps.psychiatryonline.org.] Because there were two separate implementations of environmental change on each unit, a follow-up model was conducted that included each environmental change implementation separately. Only the second environmental change was associated with a significant change in the rate of seclusion and restraint (F=4.99, df=1 and 125, p=.03).
Discussion
In this randomized, controlled study, the effects of a behavioral and environmental intervention (the engagement model) on the use of seclusion and restraint were observed across five inpatient psychiatric units. A significant 82.3% decrease in the use of seclusion and restraint was observed when the mean rate during the baseline phase was compared with the mean rate during the follow-up phase across all units. At the very least, these findings suggest that the use of seclusion and restraint can be decreased. The substantial reduction found in this study supports recent national and international efforts to improve the quality of care in psychiatric settings and reduce the use of institutional methods of control among psychiatric inpatients, a population recognized to be vulnerable because of serious mental illness and a high prevalence of a history of traumatic events. An important benefit of the study's multiple-baseline design was the ability to control for the effects of time and order of implementation of the interventions, as well as to control for institutional “placebo” effects resulting from changes in staff members' use of seclusion and restraint that resulted from the knowledge that their behavior was being observed.
Only one intervention component, changes to the physical characteristics of the therapeutic environment, was associated with a decrease in use of seclusion and restraint regardless of when and where it was implemented. Although two environmental interventions were implemented on each unit, only the second was uniquely associated with change. This finding suggests a cumulative effect of multiple environmental changes on each unit. Modifications of the therapeutic environment are arguably among the easiest changes to implement on an inpatient psychiatric unit, in that they are readily accepted and do not require training of staff. The current study design does not allow elaboration of the reasons why such changes were uniquely associated with decreases in the rate of seclusion and restraint. However, we suggest that the physical changes to the inpatient units served as consistent reminders to staff of the commitment to behavioral change and the dedication of the institution to eliminating use of seclusion and restraint. An inviting, calm unit environment may help set the tone for patients' and staff members' behavior on psychiatric hospital units.
The validity of the interventions is an important consideration when interpreting the findings. The findings suggest that patients' ratings of the environment and their involvement in treatment planning increased significantly after interventions designed to affect these factors, supporting the validity of implementing these specific unit-level changes. Although no other intervention validity measures evidenced statistically significant changes for either staff members or patients, the differences in patients' and staff members' scores before and after each intervention were in the hypothesized directions, with the exception of staff members' ratings of trauma sensitivity after the rules and language intervention. Thus seven of eight measures moved in the expected direction, providing preliminary support for the validity of the intervention. Nonetheless, the lack of unique association between the rate of seclusion and restraint and many of the interventions of the engagement model may result from a failure to implement these interventions in a fully meaningful way on all hospital units.
Despite the strengths of this study, we were unable to provide any control for the timing of the implementation of the AIDET intervention because it was a larger organizational initiative, and we had limited flexibility to randomize the interventions within our implementation schedule. Another limitation was that the effect of the interventions on patients' and staff members' perceptions of improvement in the quality of care on the inpatient units was not consistent. The environmental intervention and the intervention to increase involvement of patients in treatment planning were associated with significant improvements in the relevant domains of patient-perceived quality of care in independent patient samples but were not associated with significant improvements in staff-perceived quality of care. No other interventions were associated with significant improvement in patients' and staff members' perceptions of quality of care. Thus we cannot conclude that the other interventions had no effect on the rate of seclusion and restraint per se, because those interventions may have not been as well implemented as the environmental and treatment-planning interventions. Furthermore, the study may have had adequate power to detect only large changes. Other limitations include the fact that the initiative took place at a single hospital with five units serving patients of various types and levels of illness severity. It is not clear how the study's limitations might affect generalizability.
Conclusions
Altogether, the findings offer hope for efforts to reduce use of seclusion and restraint in psychiatric settings. Research is needed to replicate and extend these findings to understand patients' perspectives on similar institutional interventions and to determine the cost-effectiveness of similar interventions. Such data will yield a better understanding of effective means to improve the therapeutic climate of inpatients with severe mental illness.
Acknowledgments and disclosures
This study was part of a nonsponsored clinical research initiative. The project did not provide financial support for any of the authors.
The authors report no competing interests.