The past decade has seen a marked increase in the number of youths seeking care for emotional and behavioral problems in emergency settings across the country. Emergency department visits for nonurgent psychiatric issues are common and among the largest contributors to the increase in emergency visits by youths (
1–
3). Because emergency departments provide acute and problem-focused care and rarely have on-site pediatric mental health specialists, they are usually considered suboptimal settings for nonsuicidal youths without psychotic symptoms (
4). In response to this concern, the American College of Emergency Physicians has called for research on pediatric mental health emergencies to enhance primary care and community resources and to minimize the use of acute crisis management settings (
5). Systems-based approaches have focused on access to and sustained use of community mental health care, including implementation of mobile crisis services to divert youths from the emergency department. Such approaches have not led to a decrease in the number of nonsuicidal, nonpsychotic youths seeking emergency care (
1–
3).
Many youths who visit an emergency department are already known to the mental health system, particularly if they have behavior problems (
6–
8). However, research has not examined the relationship between use of the emergency department and use of outpatient care before and after an emergency department visit. Youths who have a repeat emergency visit within six months of a prior visit may be at the highest emotional-behavioral risk, those who incur the highest mental health care costs, and those for whom effective services are most limited. Understanding patterns of outpatient care among these youths is a crucial first step in addressing the costs associated with their care and in determining whether factors related to the quality of care or their satisfaction with care in the emergency department underlie this resource use pattern. The objectives of this study were to identify for which patients and for what types of problems the emergency care setting was repeatedly used and how the use of emergency care by youths was related to their use of outpatient mental health treatment. The preliminary findings are intended to support future research that could inform systems-based approaches to patient-centered care.
Methods
Data for this study were collected from the Johns Hopkins Hospital Pediatric Emergency Department (JHH-PED), which is situated in a large general hospital. The clinical staff includes pediatric attending physicians, residents, nurses, and social workers. Each year approximately 23,000 youths from Baltimore and the Baltimore metropolitan region are seen in the JHH-PED. Most of the youths are African American (75%), and just over half are male (52%). One-third are under the age of three, and two-thirds range in age from three to 17. The Johns Hopkins Division of Child and Adolescent Psychiatry provides subspecialty consultation when requested for youths in psychiatric crisis. There were 4,092 psychiatric consultations for 2,903 youths in the eight-year period from 2002 to 2009.
The sample included youths who had an initial emergency department visit before December 31, 2008, and a second such visit within six months. The database included all consultations through June 30, 2009; therefore, the index visit cutoff date ensured that all youths had a six-month window in which a second visit could be documented. The six-month window was used to identify a high-risk sample with two visits in close proximity. The short period between visits increased the likelihood that the events underlying the visits were clinically related, because this relation has greater implications for the connection to outpatient care before and between visits.
A total of 338 (12%) of the 2,903 youths met these criteria. Compared with youths who were included in the study, those who were excluded did not differ in age, gender, race-ethnicity, legal guardianship, prior suicide attempt, presenting complaint, inpatient disposition, or psychiatric diagnoses except for mood disorders, the rate of which was higher among the repeat visitors (p=.001). Youths included in the study were significantly more likely than youths who were excluded to be enrolled in Medicaid (82% and 70%, respectively; p<.001) and to live in Baltimore City (90% and 80%, respectively; p<.001). The youths in the study sample were also more likely to be known to mental health care systems: 48% had had a psychiatric hospitalization (compared with 34% of the excluded youths; p<.001), 51% had made prior use of an emergency department for a psychiatric reason (compared with 37% of the other youths; p<.001), and 71% identified a current outpatient care provider at the time of the consultation (compared with 60% of the other youths; p<.001).
Data for this study were from the Pediatric Psychiatry Emergency Evaluation Form (PPEEF), a one-page form documenting age, gender, race-ethnicity, insurance status, psychiatric diagnoses, duration of psychiatric symptoms, current mental health service use at any facility, lifetime use of pediatric services for mental health concerns, lifetime psychiatric hospitalizations, and current aftercare plans. The PPEEF is completed in real time by the child psychiatry resident on the basis of his or her comprehensive clinical evaluation of the patient and represents the patient and family's best recollection and willingness to reveal information. Deidentified PPEEF data were entered into a computer database. The data could not be linked to the individual youths. The study received exemption from informed consent. All procedures were approved by the Johns Hopkins Medicine Institutional Review Board.
Data were analyzed with SAS, version 9.2. The McNemar chi square test was used to assess the significance of differences in variables between the first and second JHH-PED visits. Bonferroni correction for multiple comparisons ensured significance testing at the 5% level (p<.004). Logistic regression models were used to assess associations between variables documented at the index visit and self-reported connection to outpatient care at the second visit. Variables were added sequentially, and the log likelihood statistic was used to assess model fit at each step. First, the presenting complaint, prior psychiatric hospitalization, and prior suicide attempt were added to the model. Next, inpatient disposition after the emergency department visit and connection to outpatient mental health care at visit 1 were added. Finally, age, gender, and race-ethnicity were added.
Results
Most of the 338 youths in the sample were male (N=190, 56%) and African American (N=270, 80%). The mean±SD age of the sample was 12.6±2.9. Nearly all lived in Baltimore City (N=305, 90%), had Medicaid (N=276, 82%), and had a biological parent as their legal guardian (N=243, 72%). Before the index JHH-PED visit, 277 youths (82%) had had contact with the mental health system in another emergency care setting (N=171, 51%), an inpatient setting (N=163, 48%), or an outpatient setting (N=281, 83%).
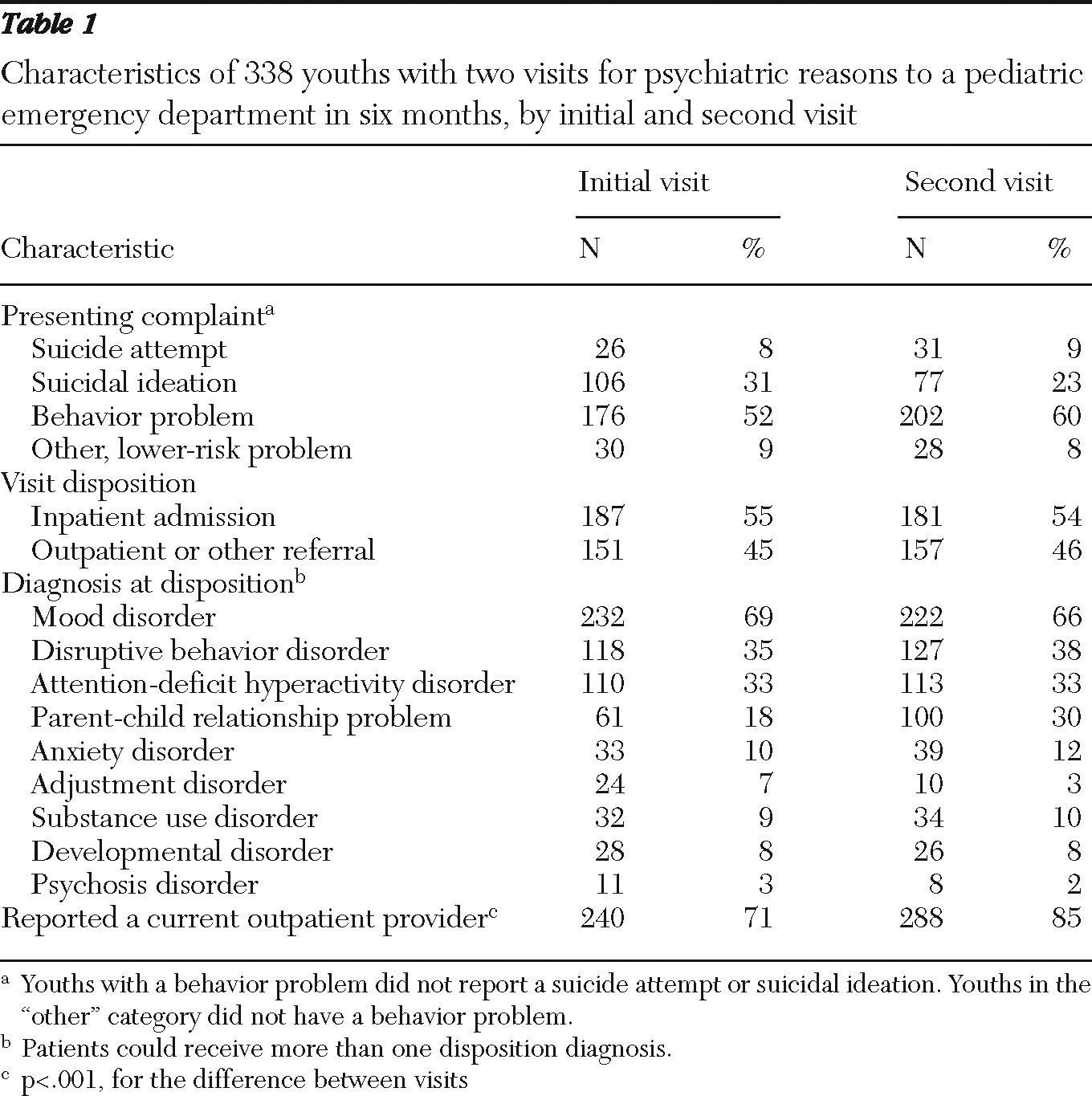
As shown in
Table 1, more than half the youths presented with a behavior problem at both the index and the repeat visit. At both visits less than 10% presented with a suicide attempt and 3% or less had psychotic symptoms. At both visits, more than half of the psychiatric consultations resulted in an inpatient admission. There were no significant differences between the two visits in diagnoses at disposition.
Youths were more likely to identify a current provider at the second visit (85%) than at the first visit (71%; p<.001). Nearly two-thirds (N=220, 65%) identified a current mental health provider at both visits, whereas only 30 youths (9%) did not identify such a provider at either visit. Of the 240 youths who were connected to outpatient care at the initial visit, 20 (8%) reported no current involvement with a provider at their second visit.
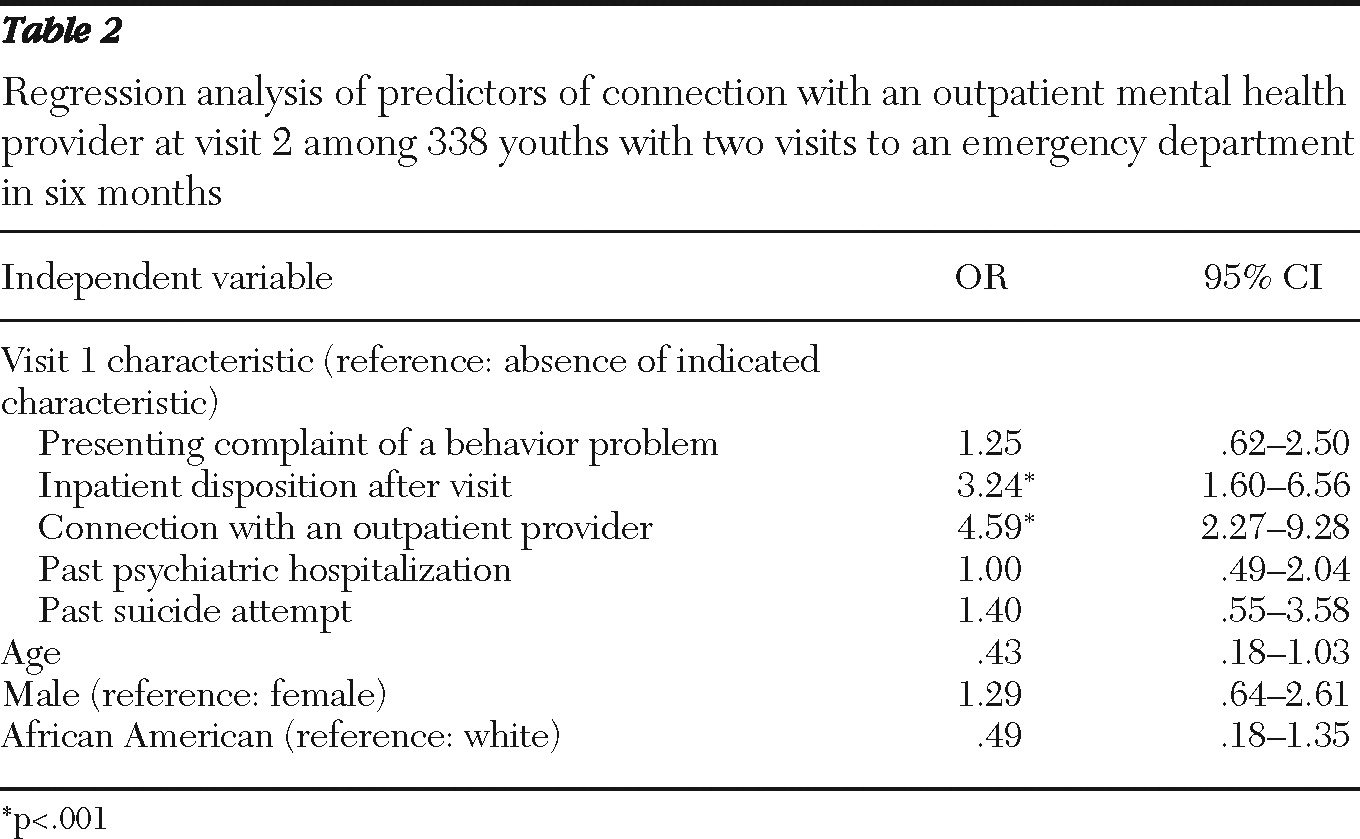
In the logistic regression models, the addition of the independent variables at each stage significantly improved the model fit. As shown in
Table 2, the likelihood of being connected to outpatient care at the second emergency department visit was nearly five times greater (odds ratio=4.59) among youths who reported a connection to care at the index visit than among those who were not connected to care at the index visit. The greater likelihood remained after analyses adjusted for presenting complaint, inpatient disposition, prior psychiatric hospitalization, prior suicide attempt, and demographic factors.
Discussion
In this study of 338 youths who presented to an emergency department in a psychiatric crisis, 12% had a repeat visit within six months, even though 71% reported at the initial visit that they had a connection to an outpatient clinician. In addition, most of the repeat users presented with nonsuicidal, nonpsychotic behavior problems at both visits, in line with previous research showing that such youths account for a large proportion (>85%) of psychiatric visits to emergency departments by children and adolescents (
1). The findings raise questions about the relationship between use of the emergency department and having a connection to outpatient mental health services.
The emergency department serves various roles in the continuum of child mental health services. Emergency settings are commonly thought to be “front doors to care,” that is, points of access to mental health care. For the 65% of youths who reported a connection to a community mental health provider at both visits, the emergency department may instead be one element in a continuum of mental health services.
Given the disconnection of the emergency department from other services, the large proportion of youths in this study who were already connected to outpatient care and who used the emergency setting for nonsuicidal, nonpsychotic problems raises questions about why they needed to do so. Perhaps their current connection to treatment increased the likelihood of direct referral by the outpatient provider to emergency settings for crisis management. In addition, some families may have found emergency care settings to be responsive to their acute needs and thus may have sought out such support repeatedly. Alternatively, the families in the study may have sought emergency care because of either tangible barriers to care (for example, limited office hours and accessibility of outpatient providers) or intangible barriers (for example, stigma and misperceptions about treatment). Views of families and outpatient providers about use of the emergency department for nonsuicidal, nonpsychotic problems may have an impact on the effectiveness of diversion programs. To fully understand the role of emergency care settings in the treatment of children with mental health problems, the temporal relationship between use of outpatient mental health services and visits to the emergency department must be examined.
The study was conducted at a single site, and findings may not generalize to all emergency care settings or patient populations. Youths with two psychiatric emergency visits within six months are likely to be a high-risk group, and the sample differed from youths who were not included in the analysis. However, the purpose of this study was to specifically target a high-risk group with two temporally related—and possibly clinically related—emergency visits. The JHH-PED is the only emergency department in Maryland with on-site child psychiatry subspecialists, which allowed the collection of more detailed information than at other emergency care sites. The PPEEF data analyzed in the study were from self-reports of family members in a crisis; data were not collected with a standardized measure. Information about the specialty of the outpatient providers seen by the youths was not collected. However, the intent of this study was to assess correlations that have not been examined in previous research and to generate information that could support future studies in which the demand for emergency services can be assessed more reliably. In addition, no information was obtained on the length of time between the most recent outpatient visit and the emergency department visit or on the frequency and consistency of care rendered by outpatient providers. The reliability of the results depends on the quality of evaluations conducted by residents in the JHH-PED. Although each cohort of residents has multiple supervisors, training in patient assessment and completion of the PPEEF is conducted by the training director (EF), and this training did not differ between years.
Conclusions
This study is a first step toward designing longitudinal studies that can clarify the temporal relationship between use of emergency care and use of specific types of outpatient services, along with associated costs, for youths with repeat visits to the emergency department. In addition, it will be important to understand how family preferences for use of emergency care services and variations in service use patterns are related to frequent use of emergency care. Research has found evidence that perceived barriers to care and parental beliefs about mental health treatment can affect access to outpatient mental health services as well as treatment adherence (
9–
12). Moreover, stigma associated with using outpatient mental health care may also be a key factor influencing use of emergency care for psychiatric crises. Finally, families and outpatient providers may follow a patient-centered paradigm that encourages emergency department use, whereas the current paradigm driving resource allocation and policy is a systems-based care model of diversion from the emergency department. A better understanding of the factors that sustain the use of emergency care can inform research, practice, and policy and help to create a system responsive to youths with psychiatric crises.
Acknowledgments and disclosures
The authors gratefully acknowledge Mark Riddle, M.D., for helpful comments.
The authors report no competing interests.