In the 1800 trial of James Hadfield, a brain-injured discharged soldier who was charged with shooting at King George III in a Drury Lane theatre, Judge Lloyd Kenyon took the unusual step of instructing the jury to state the grounds for its verdict. A verdict of “Not Guilty; he being under the influence of insanity” was returned (1,2). Verdicts of not guilty on the grounds of mental illness (NGMI), using a range of definitions, are now recognized in most English-language jurisdictions (
3–
8).
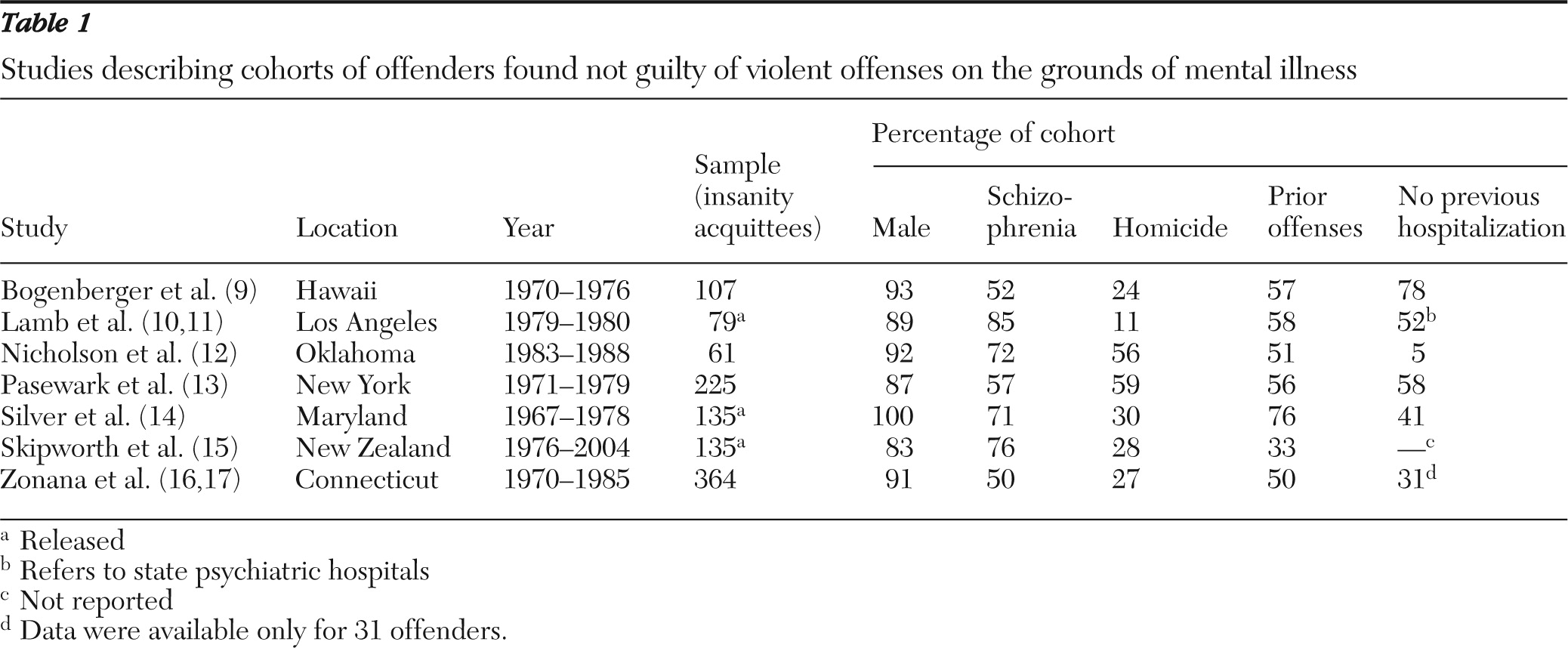
Many articles discuss the legal, philosophical, and political aspects of mental illness defenses. However, there are relatively few studies describing the clinical characteristics of violent offenders who were found NGMI (
9–
17) (
Table 1). These studies suggest that most people who receive NGMI verdicts are men with a diagnosis of schizophrenia who have committed homicide offenses. Recent studies have indicated that patients with untreated psychosis are greatly overrepresented in samples of homicide offenders with psychotic illness (
18–
21), and cohorts of NGMI offenders also include a large proportion of patients who had not previously had treatment for psychosis (
9,
11,
13,
14). However, no studies of NGMI offenders have compared those who have never been treated for psychotic illness and those who had received treatment for psychotic illness before the offense.
The defense of mental illness in all states of Australia is based on the 1846 English case of
R v. McNaughten (
22). However, the definition was broadened by the 1933 case of
R v. Porter (
23), which considered, among other issues, the capacity of accused persons to reason with sense and composure about the moral wrongfulness of their conduct. The effect of the Porter test, as it has become known, is that most homicide offenders with severe mental illness in New South Wales receive an NGMI verdict. The relative availability of the NGMI defense in New South Wales and the detailed records held by the New South Wales Mental Health Review Tribunal (MHRT) provided an opportunity to examine the characteristics of a large and well-defined sample of persons with psychotic illness who were found NGMI by the higher courts of charges of murder, attempted murder, wounding, or assault causing grievous bodily harm.
The main aim of this study was to compare the demographic, clinical, and criminological characteristics of two groups of persons found NGMI for an offense—those who committed the offense during a first episode of psychosis and those who had previously received treatment for psychosis. The specific a priori null hypothesis was that there would be a similar proportion of offenders in the first episode of psychosis among those found NGMI of homicide offenses and those found NGMI of nonlethal assaults.
Methods
Sample
In New South Wales a verdict of NGMI can be made only by the District and Supreme Courts, which hear charges arising from assaults resulting in serious injury and homicides, respectively. There are separate provisions in the local courts for offenders with mental illness who commit less serious crimes. After a verdict of NGMI, the offender becomes a forensic patient and the conditions of detention and subsequent release are determined by the MHRT. Lists of current and former forensic patients allowed the identification of documents related to 272 persons who had been found NGMI of violent offenses committed between 1992 and 2008. Data were extracted from statements of police and other witnesses, written judgments, and psychiatric reports tendered in court, using the same methods described in our earlier studies of homicide during psychotic illness in New South Wales (
19,
24,
25).
Each case was classified according to whether the offense occurred during a first episode of psychosis or after previous treatment for psychosis on the basis of a stage-of-illness model (
26) and the definition of first-episode psychosis (
27). The term “first-episode psychosis” is used synonymously with never-treated psychosis; however, it includes patients in their first weeks of antipsychotic treatment who have yet to respond to treatment. First-episode psychosis was defined as the period between the onset of positive symptoms of psychosis and an adequate period of treatment, irrespective of whether there had been previous remissions without treatment. Patients were categorized as having previously treated psychosis if they had ever received an adequate period of treatment with antipsychotic medication, regardless of whether there had been a remission from acute symptoms as a result of treatment or whether the patient was adherent to treatment at the time of the offense.
Data extraction and reliability
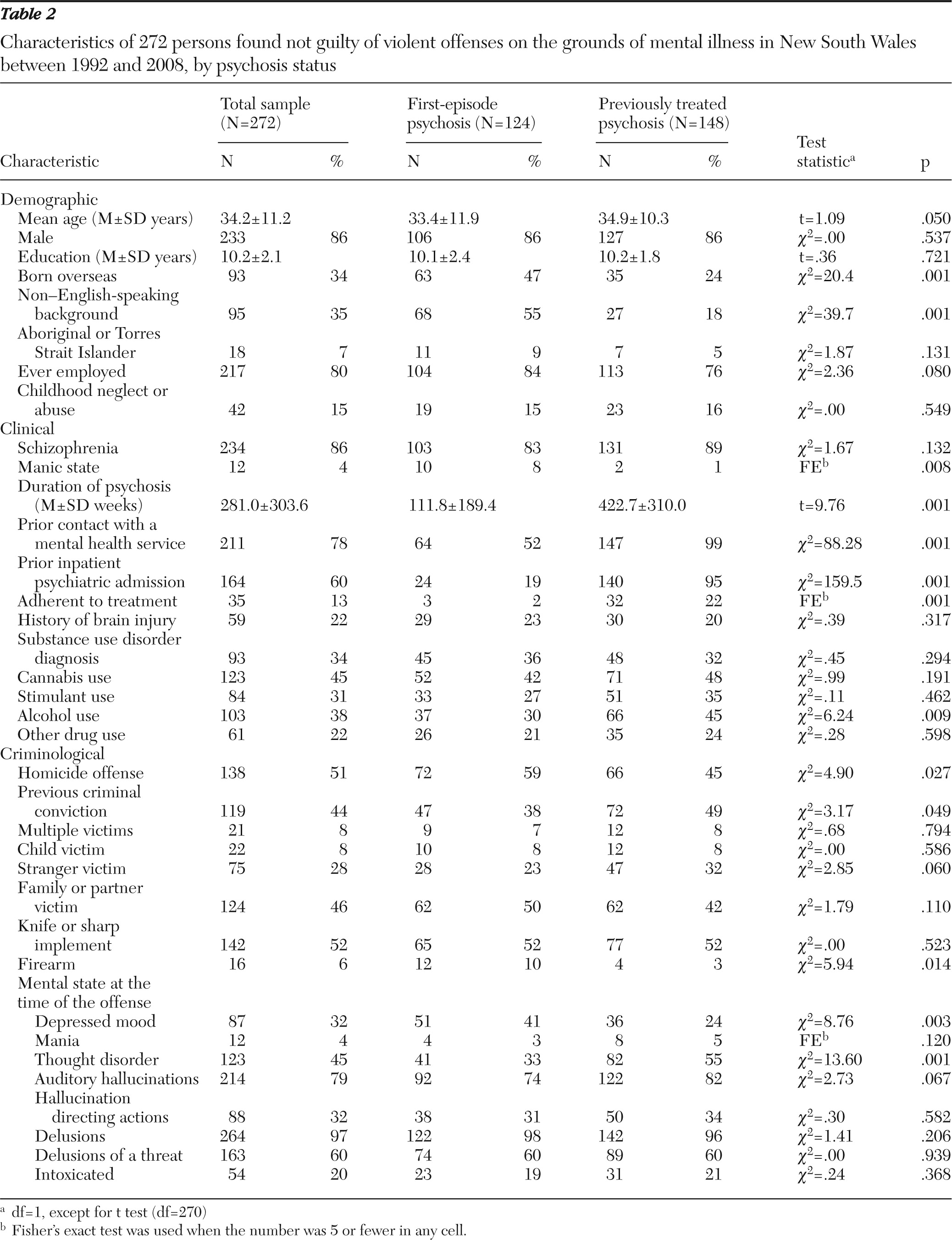
The sociodemographic, clinical, and criminological information collected is listed in
Table 2. The data were independently extracted by the first and second authors, with initial disagreement on 204 (2%) of 10,064 data points, including eight disagreements about first-episode status and 87 cases of disagreement about the duration of psychosis. Points of difference were resolved by a further examination of the patients' files. Disagreements about the duration of psychosis largely involved the number of years that patients with long-standing illnesses had been unwell. When documents contained conflicting data about the duration of illness, the shorter duration was used. Relevant information was not available for approximately 2% of data points, and omitted data points were scored as absent. In an overlapping study that included some cases from the study reported here, we found a high level of reliability in expert opinions regarding the diagnosis of psychosis (
κ=.8) (
28) and the opinion of psychiatrists about the availability of an NGMI defense (
κ=.6) (
29).
Statistical analysis
The characteristics of two groups of persons with psychosis found NGMI of violent offenses were compared: those who were in a first episode of psychosis and those who had previously received treatment with antipsychotic medication. The categorical variables were compared with chi square statistics or a Fisher's exact test if there were five or fewer in any cell. Continuous variables were examined with an unmatched, two-tailed Student's t test. Factors that were associated with first-episode or previous-treatment status with a p value of ≤.1 on bivariate testing were included in a multiple logistic regression model with first-episode psychosis as the independent variable. The results of the examination of differences in the characteristics of first-episode and previously treated patients should be interpreted with caution because no Bonferroni correction was made for the number of comparisons.
Ethical approval
Permission to conduct the study was obtained from the St. Vincent's Hospital Human Research and Ethics Committee and the MHRT.
Results
Sample and first-episode status
Between 1992 and 2008 a total of 272 persons were found NGMI of a violent offense in New South Wales (
Table 2). They included 138 found NGMI after a homicide, which indicated an annual rate of .13 NGMI verdicts for homicide per 100,000 of the total population and accounted for 8% of the 1,729 homicides recorded in New South Wales during the study period. The proportion of offenders who had never received treatment for psychosis was significantly higher among homicide offenders (72 of 138, 52%) than among those charged with other violent offenses (52 of 134, 39%) (p=.027).
Criminological variables
Fewer than half of the offenders had a previous criminal conviction (44%), which included convictions as a juvenile and convictions for driving offenses. As shown in
Table 2, about half of the victims were family members or intimate partners (46%). A little over a quarter of the victims were strangers (28%), although strangers were less likely to be the victims of a homicide offense (19 of 138, 14%) (χ
2=26.7, df=1, p<.001). The most common method of assault was with a knife or sharp implement (52%), and only 6% of offenders used a firearm.
Clinical features
Eighty-six percent of the 272 offenders had a diagnosis of schizophrenia or schizophreniform psychosis (
Table 2). The primary diagnoses of the remaining patients were schizoaffective disorder (N=13, 5%), delusional disorder (N=6, 2%), drug-induced psychosis (N=4, 2%), psychosis associated with epilepsy (N=4), psychotic depression (N=3, 1%), bipolar disorder (N=2, 1%), other organic psychosis (N=2), postnatal psychosis (N=2), and mental retardation (N=2). Of the 272 offenders, 34% had a co-occurring substance use disorder, and 20% were reported to have been intoxicated at the time of the offense. Previous substance use, particularly the use of cannabis (45%), was reported for a large percentage of offenders. A history of a previous brain injury resulting in loss of consciousness was reported in over a fifth of cases (22%).
One of the legal requirements for a finding of NGMI is the presence of a “defect of reason,” which in medical terms translates to the presence of a delusional belief or a severe disturbance of the capacity for rational thinking. Therefore, in our sample a delusional belief at the time of the offense was reported in almost every case (97%). The most common delusion was that the victim posed a threat to the offender (60%). Auditory hallucinations were reported by 79% of the offenders, and 32% reported that the hallucinations either directed their actions or warned them about the victim shortly before the offense. Twelve patients, ten of whom had a diagnosis of schizoaffective disorder, were described as being in a manic state at the time of the offense. A third of the offenders (32%) reported a co-occurring depressed mood at the time of the offense.
Comparison of first-episode and previously treated groups
Of the total of 272 offenders found NGMI, 124 (46%) were classified as being in their first episode of psychosis, including two who killed fellow patients on the day of admission to a psychiatric hospital and another two who killed a person within a month of starting antipsychotic treatment.
Despite a mean delay of more than two years between the onset of psychotic symptoms and the offense, first-episode patients were significantly younger than those who had previously received treatment (
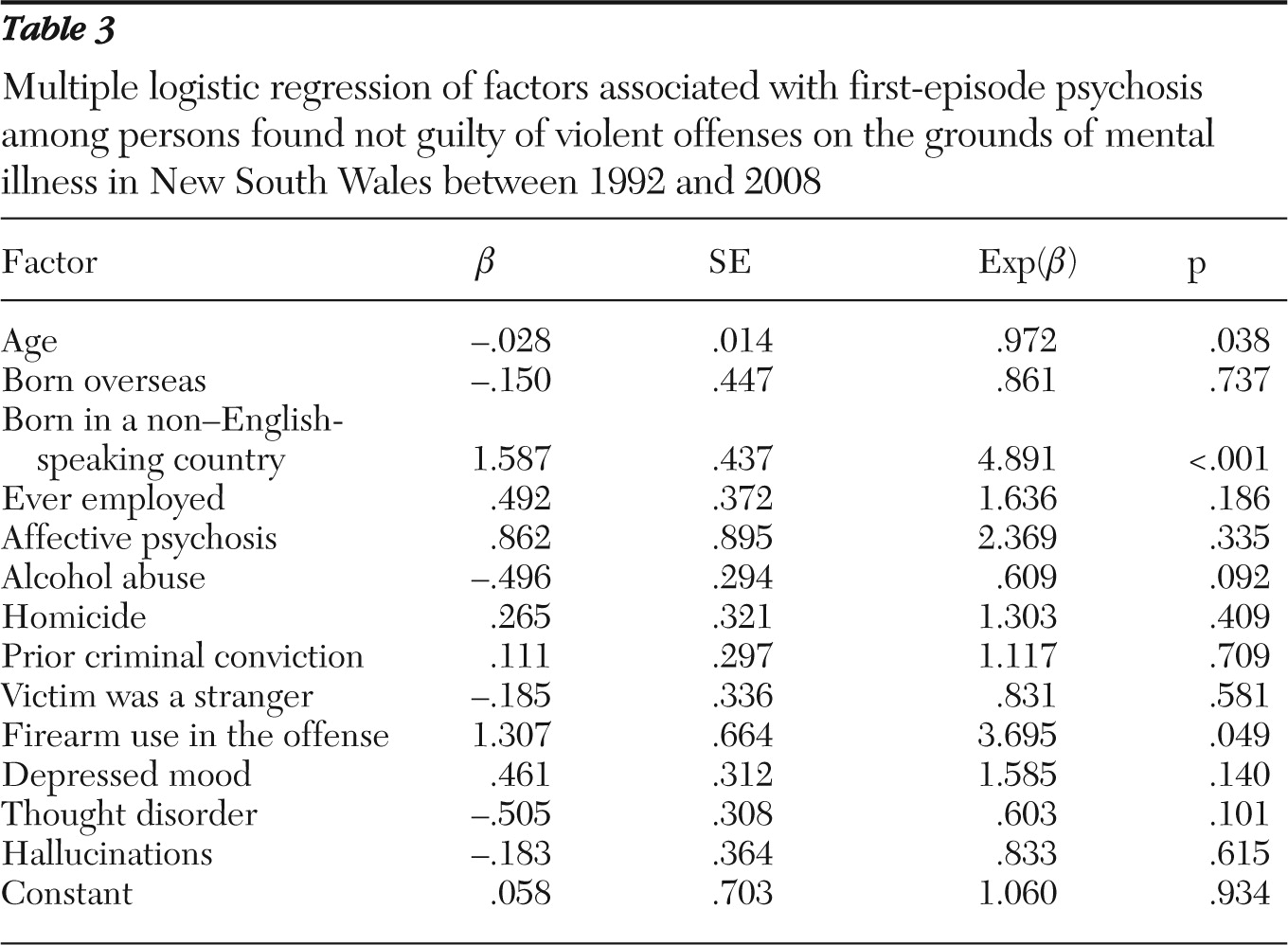
Table 2). No significant differences were found in the proportion of males, the number of years of education, the proportion who had ever held paid employment, or the patterns of substance abuse. First-episode patients were more likely to have been born overseas, to be from a non-English-speaking country, to report depressed mood at the time of the offense, to have a diagnosis of an affective psychosis, and to have used a firearm. A larger proportion of the previously treated patients were described as exhibiting thought disorder at the time of the initial assessment, and a larger proportion of the previously treated group had a prior criminal conviction. Multiple logistic regression found that younger age, coming from a non-English-speaking country, and use of a firearm in the offense were independently associated with being in the subgroup with first-episode psychosis (
Table 3).
Discussion
This study examined characteristics of the 272 people who were found NGMI of a serious violent offense committed in New South Wales between 1992 and 2008. With respect to the a priori hypothesis, we found that the proportion of first-episode psychosis patients was higher among homicide offenders (52%) than among offenders who had committed severe nonlethal assaults (39%). However, the finding that nearly half of both the homicides and the severe nonlethal assaults by patients with a psychotic illness occurred before initial treatment for psychosis suggests that there is also a strong association between severe nonlethal violence to others and first-episode psychosis.
The strength of that association can be inferred from studies of the epidemiology of schizophrenia. Meta-analyses have calculated the incidence of new cases of schizophrenia to be 21.9 per 100,000 population per year and the prevalence to be 440 cases per 100,000 population (
30). This suggests that in any given year in a population with a typical incidence and prevalence of psychosis, the number of people with an established psychotic illness will be about 20 times higher than the number of new presentations (440:22=20:1). A similar ratio of the number of untreated to treated patients in the community can be inferred from the estimate of the mean duration of untreated psychosis—about one year (
31)—and the generally prolonged or lifelong course of schizophrenia. Thus the finding of similar proportions of first-episode and previously treated patients in a sample of patients with psychosis who had committed an act of violence suggests a marked overrepresentation of first-episode patients and the presence of a strong association between first-episode psychosis and violent acts. We previously reported an association between first-episode psychosis and homicide (
19,
25,
32), violent suicide attempts (
33,
34), and episodes of major self-mutilation (
35). The finding of a large proportion of patients in a first episode of psychosis in a sample of patients with psychosis who had committed an act of severe nonlethal violence indicates an elevated risk of that form of harm associated with first-episode psychosis.
We found that among NGMI offenders, those in a first episode of psychosis differed from previously treated patients on a number of demographic, diagnostic, clinical, and criminological variables. Not surprisingly, the first-episode patients were younger, although the average age at onset was higher than might be expected even after the prolonged average duration of untreated psychosis was taken into consideration. The younger age might be explained by a larger percentage of patients with the paranoid subtype of schizophrenia in the first-episode group compared with the previously treated group (
19). Patients in the first-episode group were more likely to come from non-English-speaking countries. This is consistent with results of a German study of homicide by persons with mental illness, which found a greater risk of homicide during psychosis among non-German-speaking immigrants (
36).
Our study also found differences in the patterns of symptoms of first-episode and previously treated patients. Those in the first-episode group were more likely to have a diagnosis of affective psychosis and to report feeling depressed at the time of the offense, often in response to distressing delusional beliefs. Previously treated patients were more likely to be described as exhibiting disorder of form of thought at the time of the initial psychiatric evaluation, probably because of a larger proportion of patients with disorganized and treatment-resistant subtypes of schizophrenia in this group (
19).
A larger proportion of the first-episode patients committed their offenses with a firearm. However, this finding might be explained by a change in gun laws in Australia after a notorious mass shooting in 1996 that resulted in a ban on automatic weapons and closer scrutiny of applicants for firearms licenses. The changes made it more difficult for patients with established mental illness to obtain legal access to firearms. The changes to gun laws have been followed by a steady decline in the proportion of suicides (
37) and of homicides (
38) by means of firearms. The rates of substance abuse and intoxication with alcohol and other drugs at the time of the offense were similar in both groups, although patients with previously treated psychosis were more likely to have reported regular use of alcohol. Previously treated patients were also more likely to have a criminal record, including for minor offenses, possibly because they were older or had come to the attention of the police in the course of their illness. The high rate of substance use disorders in the sample as a whole (34%) is consistent with the role of substance use in potentiating violence among persons with a psychotic disorder (
39–
41).
A limitation of the study is that the sample was identified on the basis of a legal verdict, which could affect the sample in two ways. First, a finding of NGMI in New South Wales is less likely when the prosecution elects to contest a case in which the defense of mental illness is raised, either on the basis of a psychiatric opinion disagreeing with that plea or at the request of the victim's family. This had the effect of narrowing the sample to persons with the most severe forms of mental illness—that is, to cases in which both the defense and the prosecution experts agreed that the defense of mental illness was available. Second, some persons who had the defense of mental illness open to them elected to enter a plea of guilty in order to receive a fixed sentence, rather than risk the indefinite detention that can follow an NGMI verdict. This was particularly true for assaults resulting in less serious injuries. A further limitation of the study is the retrospective nature of assessments and reliance on data collected for court purposes rather than for research. However, the court verdicts relied on contemporaneous observations and detailed corroborative history, as well as on psychiatric opinions that have been shown in a related study to be highly reliable (
28), and it is unlikely that the results of a prospective study in which data were collected soon after the offense would have been very different.
Conclusions
This study confirmed the association between homicide and first-episode psychosis and demonstrated that a large proportion of serious nonlethal assaults committed during psychotic illness are committed before initial treatment for psychosis. The findings add to the evidence for a particular association between first-episode psychosis and the most serious forms of violence. Many of the first-episode patients in this study had been psychotic for several years and responded well to treatment provided in custody. The results of this study suggest that earlier treatment of psychosis might prevent some homicides and serious nonlethal assaults.
Acknowledgments and disclosures
The authors thank Greg James, Q.C., and Robert Hayes, Ph.D., current and past presidents, respectively, of New South Wales MHRT, for providing access to the data.
The authors report no competing interests.