In view of the scarcity of health care resources and the increasing numbers of patients with chronic illnesses, patient self-management is widely welcomed (
1). Self-management interventions focus not only on increasing adherence to the medical regimen but also on promoting social and work-related activities and on coping with the emotional consequences of the disease (
2). Many patients with a chronic somatic condition report emotional problems, such as depressive symptoms, that restrict their social participation (
3). Even relatively mild depressive symptoms might reduce patients' quality of life (
4).
The core mechanism in self-management is increasing or returning control and responsibility to the patient. In terms of adherence to treatment, daily activities, and emotional consequences, patients with lower levels of education generally have poorer outcomes (
5,
6). By focusing on increasing or returning control to patients, self-management interventions might particularly benefit patients with lower education levels, who have been shown to have a diminished sense of control and poorer health outcomes (
7,
8). Self-management may therefore contribute to narrowing the differences in chronic disease outcomes between persons of different education levels.
Using data from the Depression in Elderly With Long-Term Afflictions (DELTA) study, a randomized controlled trial conducted in the Netherlands (
9), we examined whether patients with chronic illness who were mildly to moderately depressed and who had a low level of education would benefit more from self-management support than their counterparts with a higher level of education. In a previous report, we noted that nine months after the DELTA study, patients who received the intervention had significantly fewer depressive symptoms than patients in the control group who received care as usual (
9). In the study reported here, we examined possible disparities between groups with different levels of education in terms of the benefits derived from the self-management intervention.
Methods
The DELTA study was a two-armed, randomized controlled trial, conducted between October 2003 and May 2005, with an additional nine months of follow-up (
9). Patients with type 2 diabetes or chronic obstructive pulmonary disease (COPD) aged 60 years or older were recruited from 89 randomly selected family practices in the southern region of the Netherlands. The Patient Health Questionnaire was used to screen for depression. The Mini International Neuropsychiatric Interview was used to confirm the diagnosis of depression and to exclude patients who had major psychiatric comorbidity, such as schizophrenia, and suicidal ideation (these patients were referred to their family doctor). Finally, patients with severe major depression (a score of >18 on the Hamilton Depression Rating Scale) were also excluded. The selection procedure has been described more fully elsewhere (
9).
After providing informed consent, 361 patients with mild to moderate symptoms and either diabetes (N=185) or COPD (N=176) were randomly assigned to the intervention or to usual care. Stratification was used to ensure an equal distribution of the underlying diseases (diabetes or COPD) and family practices across the intervention and control groups. A block size of two was used because we expected to include a small number of patients per general practice and we wanted to have equal numbers in both groups. The study was approved by the Medical Ethics Committee of Maastricht University and the Maastricht University Hospital.
Compared with the control group that received care as usual (N=178), patients in the intervention group (N=183) received an additional tailored and nurse-administered intervention aimed at reducing depression and increasing quality of life. Because promoting self-management skills was the means to achieving health improvements, the nurses were trained in techniques of self-management and cognitive-behavioral therapy; reattribution of negative cognitions and problem solving were core elements of the intervention (
9). Over three months, patients in the intervention group received two to ten visits by the nurse (an average of four visits).
Level of education was determined at baseline by using eight ordinal categories. These were also grouped into three hierarchical levels: low education (that is, primary education, for children aged 6 through 11 years), medium education (that is, lower vocational education for adolescents aged 12 through 16 years), and high education (that is, higher than lower vocational education, including university, for persons aged 12 and older). The primary outcome measure was depressive symptoms, as measured by the Beck Depression Inventory. Also examined were health-related quality of life, as measured by the physical and mental component scores of the 36-item Short-Form Health Survey, and control beliefs, as measured by Pearlin and Schooler's Mastery Scale (
10) and Sherer and colleagues' General Self-Efficacy Scale (
11). Control beliefs reflect the supposed pathway by which self-management affects outcomes. All outcomes were assessed at baseline and at one week and three and nine months after the intervention.
Linear regression was used to examine differences by education level in the effectiveness of the intervention for the three separate follow-up phases and for each of the five outcome measures. Analyses controlled for age, sex, underlying somatic disease, and baseline scores on all measures.
Results
The control and intervention groups were highly similar in terms of age, sex, underlying disease, and baseline scores. Of 24 tests of the difference between groups, only one was statistically significant—the mean age in the group with the highest education (72.68±6.95 years for the intervention group and 70.12±6.21 years for the control group (p=.03) (data not shown).
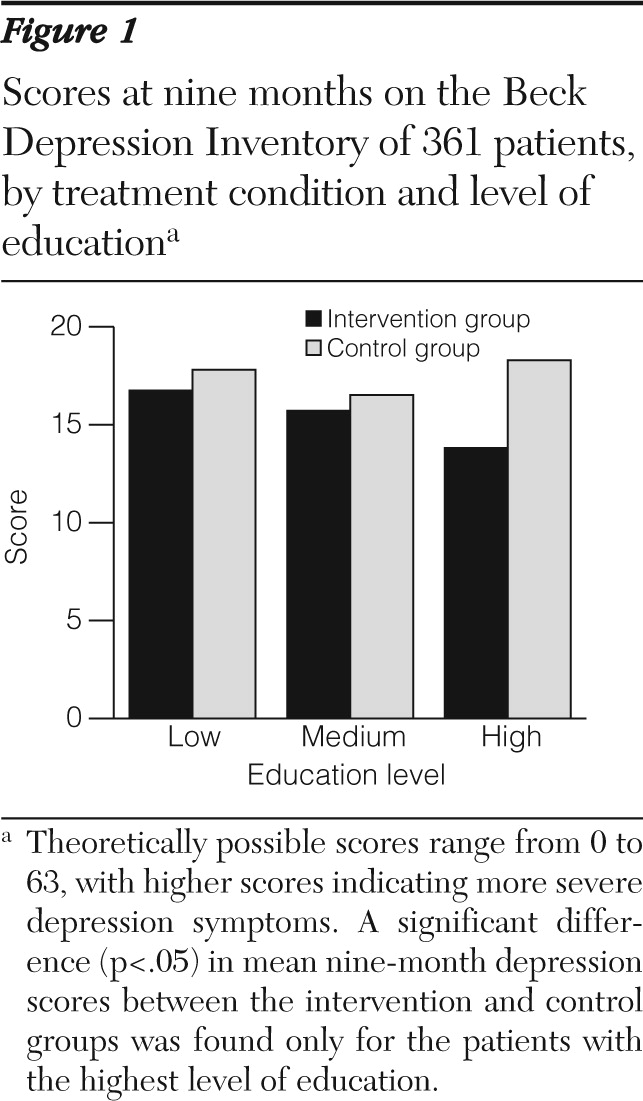
For all five outcomes, the interaction term between education level (the eight categories) and group (intervention or control) at both the three-month and nine-month follow-ups was either significant at the .05 level (seven of ten tests) or approaching significance at the .10 level (three of ten tests) (data not shown). Subgroup analyses indicated that patients who had only a primary education did not benefit in terms of any of the five outcomes. The positive effects of the intervention appeared confined to the group with the highest level of education, as shown in
Figure 1 for the primary outcome of depression symptoms.
Nine months after the intervention, only patients with the highest level of education in the intervention group showed a clinically relevant improvement in depression (a 50% or greater reduction over baseline) (
12). Of the 39 patients with the highest level of education in the intervention group, 11 (28%) showed a clinically relevant improvement at nine months, compared with one (2%) of the 46 patients with the highest level of education in the control group. Of the 36 patients in the intervention group with the lowest level of education, four (11%) showed a clinically relevant improvement in depression at nine months, compared with six (13%) of the 47 control group patients with the lowest level of education (data not shown).
Additional analyses indicated that findings were similar for patients with diabetes and with COPD and were independent of the severity of the disease (data not shown). Although the results of the initial screening questionnaire showed that persons with lower levels of education had higher depression scores, these persons were nevertheless more likely to decide not to participate in the intervention or to drop out after the intervention. We also found that the number of contacts with the nurse and the mean duration of visits did not differ between the groups with high and low levels of education. In addition, the diabetes and COPD groups did not differ in terms of how completely the intervention had been delivered to them (as reported by the nurses).
Discussion
The benefits of our short self-management intervention for older patients with chronic illness who were mildly to moderately depressed were confined to those with higher levels of education. An intervention with a different design that had a different balance of the elements of self-management and reattribution, that was embedded more strongly in the regular health care system, or that provided “booster” sessions of the intervention might have resulted in more equal benefits of depression treatment across the education groups (
13). However, efforts to reduce differences in outcomes of depression treatment between groups with different levels of education have been discouraging, whether they are based on psychopharmacology or psychotherapy (
6,
14). Thus differences in education should be taken into account when self-management interventions are implemented; otherwise self-management support might widen rather than narrow the differences in health outcomes between patients with chronic general medical conditions who have different levels of education.
Groups with lower levels of education have more to gain from such interventions. However, self-management interventions that aim to strengthen personal characteristics, such as control beliefs, might be less effective when environmental factors that induce beliefs about having low control (for example, low job control, economic deprivation, and poor neighborhood and housing conditions) are not addressed among persons with a low level of education. At the same time, participants with a higher level of education may also have benefited from their greater intellectual and cognitive abilities, enabling them to better understand the principles and potential of self-management (
15). Because we did not examine the environmental and intellectual correlates of education level, further studies should examine how factors related to the environment and to intelligence interact with self-management interventions and how these factors could also be addressed.
It should be acknowledged that the DELTA randomized controlled trial was not designed to specifically examine differences in effectiveness between groups on the basis of education (
9). This would have required different power calculations; also the stratification in the randomization scheme would have had to take into account the patients' education levels. A posteriori, in all three education groups, few baseline differences were noted between the intervention and control groups, and statistical power appeared sufficient to find significant interaction effects and positive effects among patients with higher levels of education.
Conclusions
Self-management interventions, which aim at increasing or returning control and responsibility to patients, have been shown to be effective and are therefore widely implemented. We predicted that patients with lower levels of education would benefit more from such interventions than patients with higher levels of education because the former group's generally lower levels of control would leave more room for them to benefit. Our findings indicated, however, that patients with only a primary education did not benefit from the self-management intervention, unlike patients with higher levels of education, for whom the intervention was effective. Future studies should investigate whether improving self-management skills also depends on having an environment that promotes and supports self-efficacy or on having higher intellectual abilities. Patients with lower levels of education may benefit more from an intensified problem-solving and stepped-care approach (
13). DELTA is currently evaluating an intensified self-management approach with a relatively strong emphasis on problem solving instead of on reattribution techniques, especially for people with lower levels of education.
Acknowledgments and disclosures
This study was funded by the Program on Health Care Efficiency Research (grant 945-03-047) of the Netherlands Organization for Health Research and Development (ZonMw). The authors thank Kitty Daemen, B.N., Henny Geelen, B.N., Francine Hendriks, B.N., and Mieke Witte, B.N., for administering the intervention; Wendy Engering, B.N., for her contribution to patient recruitment; and Dorien Mintjes, M.Sc., for her contribution to data entry. The authors also thank MEMIC—the Centre for Data and Information Management at Maastricht University—for providing a data management system.
The authors report no competing interests.