Vocational rehabilitation (VR) services for people with mental illnesses have received increasing attention as a result of the President's New Freedom Commission Report of 2003 and recovery transformation initiatives (
1). After decades of concern about the negative impact of employment on clinical stability, it is now recognized that individuals with mental illnesses, including persons with schizophrenia, bipolar disorder, and major depressive disorder, would, could, and should work (
2). Nonetheless, the unemployment rate for people with psychiatric disabilities has hardly budged from the 75%–85% range in the past three decades (
3).
The VR system has been described as unresponsive to the employment aspirations of those with psychiatric disabilities (
4), and questions have been consistently raised about the effectiveness of the partnership between mental health providers and their local VR office (
4–
6). VR counselors sometimes comment that the mental health system refers many people with psychiatric disabilities whom VR counselors feel are unable to benefit from VR services and fails to provide enough support for those who do receive VR services. Mental health counselors sometimes comment that VR counselors do not accurately assess the vocational potential of mental health consumers, are too quick to categorize far too many as ineligible for the services, and do not adequately accommodate the unique needs of this population.
The national Rehabilitation Services Administration's (RSA) 911 data set offered an opportunity to explore whether the VR experiences and outcomes for individuals with psychiatric disabilities differ in meaningful ways from those for individuals with other disabilities. Only a limited number of studies have used these data, and most have used data from only one state and focused on only one disability group rather than comparing outcomes across groups (
7–
9).
This study used RSA 911 data from the period 2005–2007 to examine three hypotheses: first, people with psychiatric disabilities are more likely than those with other disabilities to be found ineligible for VR services, to be categorized as having refused services, or to be determined to be too uncooperative to continue with services; second, people with psychiatric disabilities will have poorer competitive employment outcomes than those with other disabilities; and third, people with psychiatric disabilities will experience less decline in their use of public support (such as Supplemental Security Income and Social Security Disability Insurance) than those with other disabilities.
Methods
Deidentified national RSA 911 service records were obtained for individuals whose VR service records were closed in 2005 (N=470,522), 2006 (N=468,944), and 2007 (N=458,221). In addition to demographic, service use, and cost data, the RSA data set contains two variables that indicate the type and cause of the individual's primary impairment. The impairment code variable includes 20 broad categories (such as visual, respiratory, and psychological) and an impairment cause variable that provides more detail about specific impairments. This study used a sample of 865,825 adults aged 18–65 who were separated into three groups: psychotic disorders, including schizophrenia spectrum disorders (N=59,137); affective disorders, including depression, bipolar, and other mood disorders (N=153,859); and other disabilities, which combined data for individuals with physical, sensory, and developmental impairments (N=652,829). [Details about the sampling process are provided in an appendix available online at
ps.psychiatryonline.org.] The study was determined to be exempt from institutional review board review.
The RSA data set included variables such as gender, race-ethnicity, age, and education for each service recipient. A binary (yes-no) variable was created to indicate whether an individual's access to VR services was limited; the following reasons for closing a case, as determined by VR staff, were coded for the closure variable: the disability was too significant for the individual to benefit from VR services, the individual was perceived as refusing services, and the individual was viewed as uncooperative. Competitive employment was defined as full-time or part-time employment in an integrated setting, in a self-employment situation, or in a state-managed business enterprise program with or without supports and with compensation at or above the higher of the state or federal minimum wage (
10). Competitive employment at application and closure was determined with available data on employment status at each time point. Information about wages and hours worked was examined to determine whether wages met the state or federal minimum wage standard. Amount of public support income received at application and closure was coded in the data set. There were no missing data for the competitive employment data, and less than 3% of the population was excluded in the public support analyses because of missing data about public support at application or closure.
A chi square test with post hoc pairwise comparisons was used to examine the statistical significance of the association of impairment type and eligibility for and participation in VR services. A logistic regression was used to examine the adjusted association of competitive employment status at closure and impairment type, with controls for sociodemographic factors and competitive employment status at application. Analyses of variance in conjunction with Tukey's multiple-comparison procedure were used to compare the average monthly amounts of public support received by individuals in different impairment groups and to compare the change in the amount of public support at application and closure across the groups.
Results
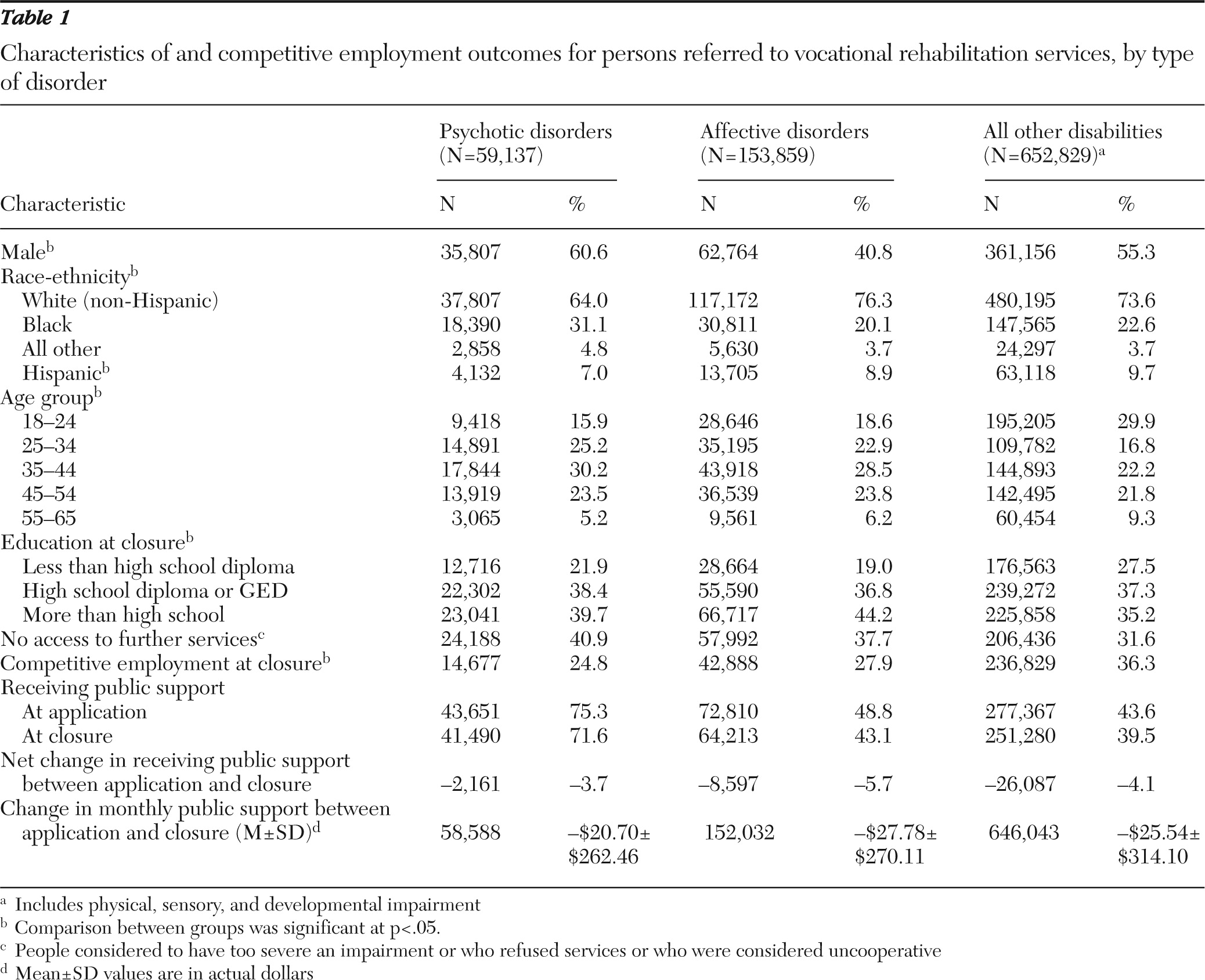
Table 1 includes the study sample characteristics and outcomes. The percentage of individuals in the psychotic disorders group whose cases were closed because their impairments were deemed too significant to benefit from services, because they reportedly refused services, or because they were viewed as uncooperative was significantly higher than for those with affective disorders (40.9% compared with 37.7%,
χ2=185.75, df=1, p<.001) and other disorders (40.9% compared with 31.6%,
χ2=2,132.28, df=1, p<.001). The percentage of persons with affective disorders was also higher than that of the group with other disorders (
χ2=2,081.97, df=1, p<.001).
As shown in
Table 1, the group with other disorders had higher competitive employment rates at closure than the groups with psychotic disorders (
χ2=3,116.37, df=1, p<.001) or affective disorders (
χ2=3,880.93, df=1, p<.001). However, the net changes in competitive employment rates within each group (percentage who were competitively employed at application subtracted from the percentage competitively employed at closure) were quite similar. Post hoc pairwise tests showed that the three groups differed in job gains and job loss (
χ2>100.00, df=2, p<.001). Those with psychiatric disabilities consistently gained fewer jobs and had higher job losses (employed at application but not at closure) than those in the group with other disorders.
The likelihood of achieving competitive employment at closure was significantly lower for individuals with psychotic disorders (odds ratio [OR]=.63, 95% Wald confidence interval [CI]=.62–.65, p<.001) and affective disorders (OR=.69, CI=.68–.70, p<.001) than for those with other disabilities. Furthermore, individuals with affective disorders were significantly more likely than those with psychotic disorders to obtain competitive employment(OR=1.09, CI=1.06–1.11, p<.001). Competitive employment at closure was positively associated with being younger (OR=.99, CI=.99–.99, p<.001), male (OR=1.02, CI=1.02–1.03, p<.001), and competitively employed at application (OR=2.85, CI=2.81–2.88, p<.001). Competitive employment was less likely among blacks (OR=.88, CI=.87–.89, p<.001) and individuals of all other (nonwhite) races and ethnicities (OR=.82, CI=.80–.84, p<.001) than among whites. Finally, a competitive employment outcome was more likely for individuals with more than a high school education (OR=1.53, CI=1.52–1.55, p<.001) and less likely for individuals with less than a high school education (OR=.88, CI=.87–.89, p<.001) than for those with a high school diploma or GED.
Persons with psychotic disorders were more likely than those with affective disorders (χ2=13,571.01, df=1, p<.001) or other disorders (χ2=22,434.62, df=1, p<.001) to be receiving public support at closure. The net percentage reduction in this support was similar for all three groups. The percentage reduction in the number of individuals with psychotic disorders who received public support at application versus closure was lower than the corresponding percentages for those with affective disorders (χ2=1,658.65, df=1, p<.001) and other disorders (χ2=2,196.18, df=1, p<.001). A larger proportion of individuals with psychotic disorders who did not receive public support at application received it at closure compared with those with affective disorders (χ2=1,052.93, df=1, p<.001) and other disorders (χ2=939.93, df=1, p<.001). All three groups experienced a decrease in the average amount of public support received from application to closure. The difference between those with psychotic disorders and the other two groups in amounts received was significant (p<.001), as was the difference between those with affective disorders and other disorders (p<.05). These findings were confirmed with the Kruskal-Wallis test.
Discussion and conclusions
Our results indicated that there are continued disparities in perceived eligibility and outcomes for individuals with psychiatric disabilities compared with those with other disabilities who received VR-funded services. These differences occurred despite our inability to predict which specific individuals would be unable to work and the possibility that rejection of offered services and “uncooperativeness” could be symptoms of a poor fit between what is offered and the needs of individuals with psychiatric disabilities. Mental health providers need to continue to provide the supports necessary to those they refer to VR to ensure successful use of VR services. VR counselors can reexamine potential preconceptions about the ability of individuals with psychiatric disabilities to succeed and to explore a full range of work options. Improving communication between VR counselors and mental health providers is likely to have positive impacts on both access and outcomes (
11).
Competitive employment, rather than other types of employment outcomes (such as sheltered or transitional employment), is the standard outcome of primary interest in most current vocational studies. Overall, VR services were associated with increased competitive employment and decreases in public support for all groups. For example, although the monthly reductions in entitlements may seem small at the individual level, the magnitude of the annual decrease in public support for persons receiving VR services was $14,553,259 for those with psychotic disorders, $50,681,388 for those with affective disorders, and $197,999,259 for those with other disorders. Our findings suggest that VR services may be effective, but more rigorous designs are needed to reach more definitive conclusions. Nonetheless, our results also suggest an outcome disparity between those with psychiatric disabilities and those with other disabilities.
Limitations to consider include our use of administrative RSA data, which likely included errors in data entry and completeness. However, such errors are not expected to bias results in one direction or the other and should not dramatically influence our results. The validity of the psychiatric impairment categories may also be questionable given that the VR providers lacked a standardized assessment approach. Nonetheless, the overall findings of differences between persons with psychiatric disabilities and those with other disabilities would still hold.
Clearly there is room for improving employment for all disability groups. Future studies should examine the types of services received to assess whether people with different types of disabilities receive different types or levels of services, which may be responsible for differential impact in outcomes. Future outcome studies can also examine job tenure and individuals' subsequent long-term attachment to the labor market and whether VR services affect consumers with different disabilities at different rates. We also expect that new and more effective VR models will be needed and that other factors in employment, such as the age, gender, race-ethnicity, and education differences we found, also need greater empirical research attention and recommendations for practice. For persons with psychiatric disabilities, a major focus for research would address discrimination and transportation factors and how they affect employment. Current policies, including promotional efforts to increase knowledge about and use of available incentives to employment, should also receive attention.
Acknowledgments and disclosures
Support for the study was provided by grant H133B100037 (Dr. Salzer, principal investigator) from the National Institute on Disability and Rehabilitation Research and the Department of Education. The contents of this article do not necessarily represent the policy of the Department of Education, nor endorsement by the federal government.
The authors report no competing interests.