Multiple return visits to psychiatric emergency services are estimated to account for one-third of all visits (
1). Developing a better understanding of factors related to patients with multiple emergency service visits may improve the delivery of mental health care (
2). Several sociodemographic and clinical characteristics have been identified as predictors of repeat visits to psychiatric emergency services: having less access to resources (
3,
4), being male, being young or middle-aged, being unmarried, and having a psychotic disorder, a substance use disorder, or a personality disorder (
5).
In these longitudinal studies, the absence of diagnostic variability over time was assumed (
3–
5). However, several authors have noted that significant fluctuations in diagnoses are observed as longitudinal data become available (
6). Several factors may contribute to diagnostic variability, including the evolution of an illness, emergence of new information, and lack of reliable measurement (
6). Clinically, diagnostic variability can lead to diagnostic misclassification, inappropriate treatment recommendations, and iatrogenic effects (
7).
The purpose of this study was to examine characteristics of frequent visitors to a psychiatric emergency service in a French public teaching hospital over a six-year period (2001–2006). The focus of the study was the diagnostic variability of psychotic disorders. We hypothesized that the stability of diagnoses would vary over time and that variability would be greater among frequent visitors than among occasional visitors. Diagnostic variability was defined as the extent to which a patient's diagnosis was changed from a nonaffective psychotic disorder to an affective psychotic disorder.
Methods
The study was conducted in the psychiatric emergency service of a large, public teaching hospital in Marseille (
4). Located in southeastern France, Marseille is the country's second largest city, with a population of nearly one million. The study involved a retrospective review of administrative and medical databases from the psychiatric emergency service. We analyzed data from all episodes of care in the psychiatric emergency service from January 1, 2001, to December 31, 2006, for persons aged 15 and older. Eligible patients were those with psychotic disorders who made more than one visit to the psychiatric emergency service during the study period. Psychotic disorders were identified according to
ICD-10 criteria. [A list of the main
ICD-10 diagnostic categories of psychotic disorders is available as an online appendix to this report at
ps.psychiatryonline.org.] Frequent visitors, defined as patients who made six or more visits to the psychiatric emergency service during the study period (
2,
3), were compared with occasional visitors, defined as patients who made between two and five visits during the period. The French National Commission for Data Protection approved this study. Principles outlined in the Declaration of Helsinki were followed.
Demographic information consisted of age (age at first visit), gender, marital status (the most frequently reported status, either in a couple or single), dependent children (yes or no), and homelessness status (whether the patient received health care at least once during the study period while homeless [4]). Diagnoses were made by a psychiatrist on the basis of the ICD-10 sections. Each patient was assigned one principal diagnosis from the mental disorders category and one or more secondary diagnoses when comorbid psychiatric conditions were present.
Two mutually exclusive groups were established. The first was the group considered to have diagnostic stability; these were patients with at least one diagnosis of a nonaffective psychotic disorder but no diagnosis of an affective psychotic disorder and patients with at least one diagnosis of an affective psychotic disorder but no diagnosis of a nonaffective psychotic disorder. The second group was considered to have diagnostic variability; these were patients with diagnoses of both a nonaffective psychotic disorder and an affective psychotic disorder. A second definition of diagnostic variability, used by Schwartz and colleagues (
6) and by Baca-Garcia and colleagues (
8), was employed to test the robustness of the first definition; these were patients who did not receive a diagnosis in the same
ICD-10 category of psychiatric disorders (nonaffective psychotic disorders or affective psychotic disorders) in at least 75% of the evaluations.
Logistic regression analysis was used to estimate odds ratios for the association between sociodemographic or diagnostic factors and frequent-visitor status, after adjustment for confounding factors. Variables relevant to the model were selected on the basis of their clinical interest or a threshold p value (≤2) in the univariate analysis. Only results based on the first definition of diagnostic variability are reported here. An analysis using the second definition did not change our findings (data not shown). The final model included odds ratios and 95% confidence intervals. All tests were two-tailed, and the alpha value was set at <.05. Data were analyzed with SPSS, version 18.0.
Results
Data were obtained for 8,860 patients, who made 16,754 visits to the psychiatric emergency service during the study period. A total of 2,524 patients (29%) made more than one visit during the period, and 1,285 patients (15%) were given at least one diagnosis of a psychotic disorder. Seven patients were less than 18 years old (<1%). Patients with psychotic disorders made 7,010 visits, accounting for 42% of the total number of visits. Among those with psychotic disorders, 317 (25%) were identified as frequent visitors, and 968 (75%) were considered occasional visitors.
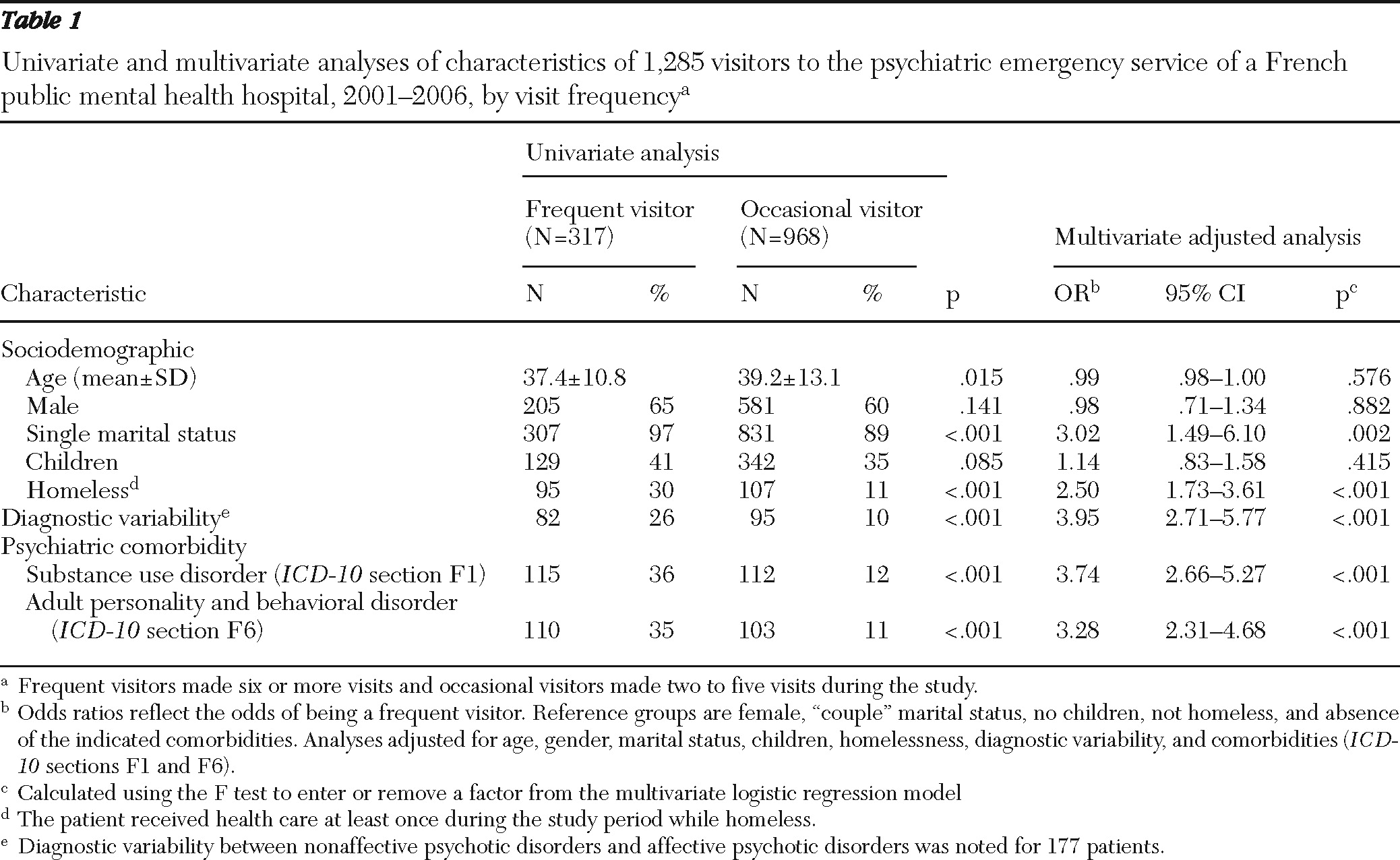
In the univariate analysis, three sociodemographic characteristics were significantly associated with being a frequent visitor: younger age (p=.015), single marital status (p<.001), and homelessness (p<.001) (
Table 1). The two groups did not differ significantly by gender or whether they had children.
Nonaffective psychotic disorders were more common among occasional visitors than frequent visitors. Over the study period, 721 occasional visitors (75%) and 215 frequent visitors (68%) were given a diagnosis of a nonaffective psychotic disorder (p=.021). Among the 317 frequent visitors, 62 (20%) were given a diagnosis of schizophrenia, schizoaffective disorder, or both, whereas 34 of the 968 occasional visitors (4%) were given either of these diagnoses (p<.05).
Affective psychotic disorders were also more common among occasional visitors than frequent visitors. Over the study period, 152 occasional visitors (16%) and 20 frequent visitors (6%) were given a diagnosis of an affective psychotic disorder (p<.001). Bipolar disorder with psychotic features was the most common diagnosis among patients who had an affective psychotic disorder—134 occasional visitors (14%) and 18 frequent visitors (6%) (p<.001).
As shown in
Table 1, diagnostic variability was greater among frequent visitors than among occasional visitors—26% and 10%, respectively (p<.001). The highest level of diagnostic variability occurred between schizophrenia and bipolar disorder—that is, the diagnosis of a patient was changed from schizophrenia to bipolar disorder or from bipolar disorder to schizophrenia. This occurred for 55 frequent visitors (17%), compared with 34 occasional visitors (4%) (p<.001). The next-highest level of variability occurred between schizoaffective disorder and bipolar disorder: 30 frequent visitors (10%) and 10 occasional visitors (1%) (p<.001). This was followed by variability between psychotic disorder not otherwise specified and bipolar disorder: 19 frequent visitors (6%) and three occasional visitors (less than 1%) (p<.001). Frequent visitors had higher rates of substance use disorders and personality disorders than occasional visitors.
A multivariate analysis confirmed the results of the univariate analysis, with the exception of findings related to age (
Table 1).
Discussion
This study found that frequent visitors to a psychiatric emergency service differed significantly from occasional visitors in several characteristics. They were more likely to be single and homeless and to have diagnostic variability, substance use disorders, and adult personality disorders. No significant differences were found between frequent and occasional visitors in age or gender. This finding contradicts those of most similar studies, which suggest that being male and young or middle-aged are predictors of repeat visits to emergency services (
3). However, several other studies have not found a correlation between frequent visits and either of these characteristics. Pasic and colleagues (
2) found that frequent and infrequent visitors did not differ significantly in age. Similarly, Hansel and Elliott (
9) found no difference in gender between these groups. It is important to note that strict comparisons between studies are difficult, because they vary in design, variables examined as predictors, samples, and definitions of frequent and occasional visitors.
In line with previous research (
3,
4), this study found that being single and being homeless were associated with being a frequent visitor. Lack of social support, general social disability, and homelessness are independent factors associated with frequent use of psychiatric emergency services (
4). This finding is particularly interesting because the French health system provides universal coverage, which might lead to the expectation that absence of economic barriers to health care should facilitate and improve access to outpatient psychiatric services and prevent individuals from visiting emergency services. An in-depth analysis of this finding is needed to better adapt the health care system to meet the unique expectations and needs of homeless patients and those in generally precarious socioeconomic standing (
4).
Diagnostic variability was greater in the frequent-visitor group than in the occasional-visitor group (26% and 10%). Potential sources of variability have been identified in longitudinal studies; they include patient variance (true changes within the patient), information variance (for example, more information available at follow-up), observation variance (for example, two observers), and criteria variance (different criteria at initial and follow-up assessments) (
6). Therefore, it seems logical that diagnostic variability would increase with the number of visits and that diagnostic variability would be higher in the frequent-visitor group. However, it is also possible that frequent visitors are patients with more complex diseases and thus more difficult diagnostic issues.
The primary question is whether current diagnostic distinctions and categories are valid. In our study, the variability mainly concerned schizophrenia and bipolar disorder. This finding can be explained by the lack of consistent evidence for differences in specificity, in terms of symptoms, etiology, treatment, and prognosis between diagnostic categories such as schizophrenia, bipolar disorder, and other psychotic disorders (
10). According to van Os (
10), the natural phenotype for psychosis is multidimensional, with different domains of distributed positive, negative, disorganized, depressive, manic, and neurocognitive symptoms that are continuous with normal mentation and relatively nonspecific with regard to traditional diagnostic constructs (or at least not specific enough to be of diagnostic value).
The variability we observed also involved a diagnosis of schizoaffective disorder changing to schizophrenia and bipolar disorder. This variability may be related to the issue of schizoaffective disorder, which is defined in the
DSM-IV and
ICD-10 within a rigid categorical classification system distinct from schizophrenia and bipolar disorder (
11). According to Lake and Hurwitz (
12), use of schizoaffective disorder as a diagnosis often solves diagnostic dilemmas associated with the atypical presentation of mood symptoms within the context of schizophrenia. Finally, our study also confirmed that diagnostic variability occurred in the category of psychosis not otherwise specified. The next generation of the
DSM and
ICD must find solutions for these difficult diagnostic issues.
As for comorbid psychiatric conditions, our findings are generally in line with those obtained in previous studies. Bruffaerts and colleagues (
13) found that occasional visitors were 60% less likely than frequent visitors to be diagnosed as having a personality disorder. A possible explanation is that more significant disabilities associated with personality disorders (for example, troubled relationships and dysfunction in everyday activities) may force patients to use psychiatric emergency services on a recurring basis (
14). Our study highlights the need to develop more effective and targeted prevention and intervention initiatives for those with personality disorders.
In addition, having a comorbid substance use disorder is associated with substantially increased emergency department use. Although substance use disorders are well-known risk factors for such use, health systems have difficulty in treating them. For example, the French health care system tends to focus on providing a patient with either mental health or substance abuse treatment services. The elevated rates of co-occurring substance use and severe mental disorders among frequent visitors to emergency psychiatric services may be an indication of insufficient and fragmented services for patients with dual diagnoses (
4).
Our study had several strengths and limitations. First, an important methodological aspect of our investigation was the definition of diagnostic variability. Diagnostic variability or stability over a longitudinal study is usually defined according to Schwartz and colleagues (
6), who proposed a comparison of the first evaluation (initial diagnosis) and last evaluation (final diagnosis). We chose another definition that we considered less restrictive because it took into consideration all diagnoses made during the study period (
15). However, although our definition offered a more comprehensive approach, there were several problems. We focused diagnostic variability on the two main categories of psychotic disorders in the
ICD-10—nonaffective and affective psychotic disorders. The incidence of diagnostic variability may have been different (likely higher) if we had chosen a more precise definition with more than two diagnostic categories. We felt that our choice was more appropriate because otherwise our results would have been too heavily influenced by the evolution of an illness or the emergence of new information in the context of a psychiatric emergency. Use of more specific subtypes might induce methodological artifacts that would contribute to the appearance of greater instability among frequent visitors. The clinical significance of this study should be cautiously interpreted in accordance with the chosen definition.
Second, there is no standard definition of high utilization of emergency services beyond the fact that frequent users repeatedly visit emergency departments. The literature identifies several cutoffs for defining high service utilization: more than one visit in a four-, six-, or 12-month period; more than six visits in an indeterminate period; six or more visits in a 12-month period; visit frequency in the upper tenth percentile; and 2 standard deviations above the mean number of visits (
2). Consequently, our cutoff choice is arbitrary. However, repeating our analyses with the definition of Pasic and colleagues (
2) (two standard deviations above the mean number of visits) or with a numeric index (number of visits) did not change the findings of our multivariate analysis (data not shown).
Third, an administrative database was the data source for the study. Data on several sociodemographic characteristics were not collected because of the difficulty of obtaining certain information in the emergency context (for example, employment and living arrangement), as well as the constraints of the French context, wherein we were unable to collect data on ethnicity. Diagnoses made by a large panel of psychiatrists in an emergency context may not be as accurate as those made with diagnostic research instruments and structured interviews. Furthermore, information about characteristics of the illness (such as severity, course, duration of untreated psychosis, and previous psychiatric history or comorbidity) was not available.
Fourth, our analysis involved only patients with more than one visit to the psychiatric emergency service. In the future, it would be interesting to analyze diagnostic variability among individual users by assessing data across different settings (for example, psychiatric emergency services and private psychiatric offices). Finally, because our study was conducted in France, our findings may not be generalizable to other health care systems.