The assertive community treatment (ACT) model, which was designed to serve persons with severe and persistent mental illnesses in the community, has been widely implemented and studied in North America and Europe (
1,
2). Some modifications to the ACT model have been successfully incorporated for employment rehabilitation (
3), management of co-occurring disorders (
4), homeless populations (
5), and parolees (
6).
Cultural competence is a desired core competence for mental health professionals (
7). The Mount Sinai Hospital ACT program, with a mandate to specifically serve the underserved ethnocultural populations of metropolitan Toronto, has demonstrated that the ACT model can be modified to suit cultural needs and remain highly effective (
8). This successful outcome suggests that the ACT model is flexible and that providers can adapt it to various cultural and clinical environments while maintaining or enhancing its clinical effectiveness.
Mount Sinai Hospital ACT adapted the model to include bilingual and bicultural staff and assignment of clinicians to patients on the basis of cultural and language requirements whenever possible and to incorporate cultural and ethnic elements into each assessment and treatment plan. For example, the team has integrated traditional Chinese medicines and remedies commonly used by clients, introduced traditional interventions (such as acupressure techniques to control weight gain and a noodle group for social support), sought and promoted culturally appropriate supportive housing, and strongly incorporated families in clients' rehabilitation plans. Other clinical innovations of the Mount Sinai Hospital ACT include delivering multifamily psychoeducation groups (
9), prioritizing and incorporating cultural formulation and clients' explanatory models in overall care (
10), and having a general practitioner who is also a psychotherapist on the team to enhance assessment, management, and follow-up of clients' general medical and counseling needs.
As part of a global movement toward improving quality of life for patients with mental illness, the Japanese Ministry of Health, Labor, and Welfare has called for enhanced community care for these patients to facilitate discharge by 2013 of about 72,000 long-stay patients in psychiatric hospitals (
11). In 2000 the KUINA Center, located 110 km from Tokyo in the central part of Hitachinaka City (population 153,000), Ibaraki Prefecture, developed an ACT team based on the Mount Sinai Hospital ACT model to serve the seriously mentally ill population.
In contrast to Mount Sinai ACT's 100% government funding, the KUINA Center ACT has a mixed structure; 90% of funding is from government sources (of which half is from the prefecture level and half from the municipality level), and 10% is from fees charged to patients. The fees paid by patients for ACT are similar to fees that patients pay for general medical care (
11). Patients can obtain government aid to pay such fees, depending on their income. As a result, the KUINA Center does not turn patients away for financial reasons. The KUINA Center is a multifaceted, privately run, community social service agency that also provides case management services, hotline assistance, and a group home for individuals with psychiatric disorders. It is closely linked with a continuum of psychiatric services that includes outpatient clinic care, psychiatric day care, and inpatient hospital care. The Ibaraki Prefecture is divided into nine medical welfare circles. For Hitachinaka city's circle, there are two psychiatric hospitals, three general hospitals with outpatient psychiatry programs, and six private psychiatric outpatient clinics. Referrals to KUINA ACT come mainly from families of patients.
In 2001 Mount Sinai ACT, the Japanese Association of Mental Health and Welfare Professionals (JAMHWP), and the KUINA Center established an agreement: the staff of Mount Sinai ACT would provide ongoing training of the JAMHWP and the KUINA ACT staff. In Japan the training component is delivered in annual training sessions by two senior members of the Toronto team. In Toronto the training consists of two annual weeklong sessions.
This study mainly compared the Mount Sinai ACT and the KUINA Center ACT for fidelity to ACT guidelines and principles and populations served to determine whether the successful outcomes of Mount Sinai ACT could be reproduced in a Japanese setting. The findings may be useful for countries and jurisdictions that are new to the ACT model and are considering it to enhance their community support and treatment programs.
Methods
Data were collected between 2002 and 2005 in five domains of comparison chosen for the study: patient demographic profiles (review of charted intake forms), fidelity to the ACT model as defined in the Dartmouth Assertive Community Treatment Fidelity Scale (
12), client satisfaction (a patient and family standard questionnaire for both teams), patient clinical profiles (chart review), and outcomes over the study period (Brief Psychiatric Rating Scale [BPRS] and chart review).
Mount Sinai ACT collected data for the first 66 patients and KUINA ACT for the first 40 patients admitted to their programs. Mount Sinai ACT outcomes were based on comparisons of data for one year before admission to ACT and one year after admission. KUINA ACT patients were assessed on the same parameters, but the periods were six months before admission and six months after admission. The different periods used by the teams were chosen on the basis of availability of complete data sets at the time of the study.
Results
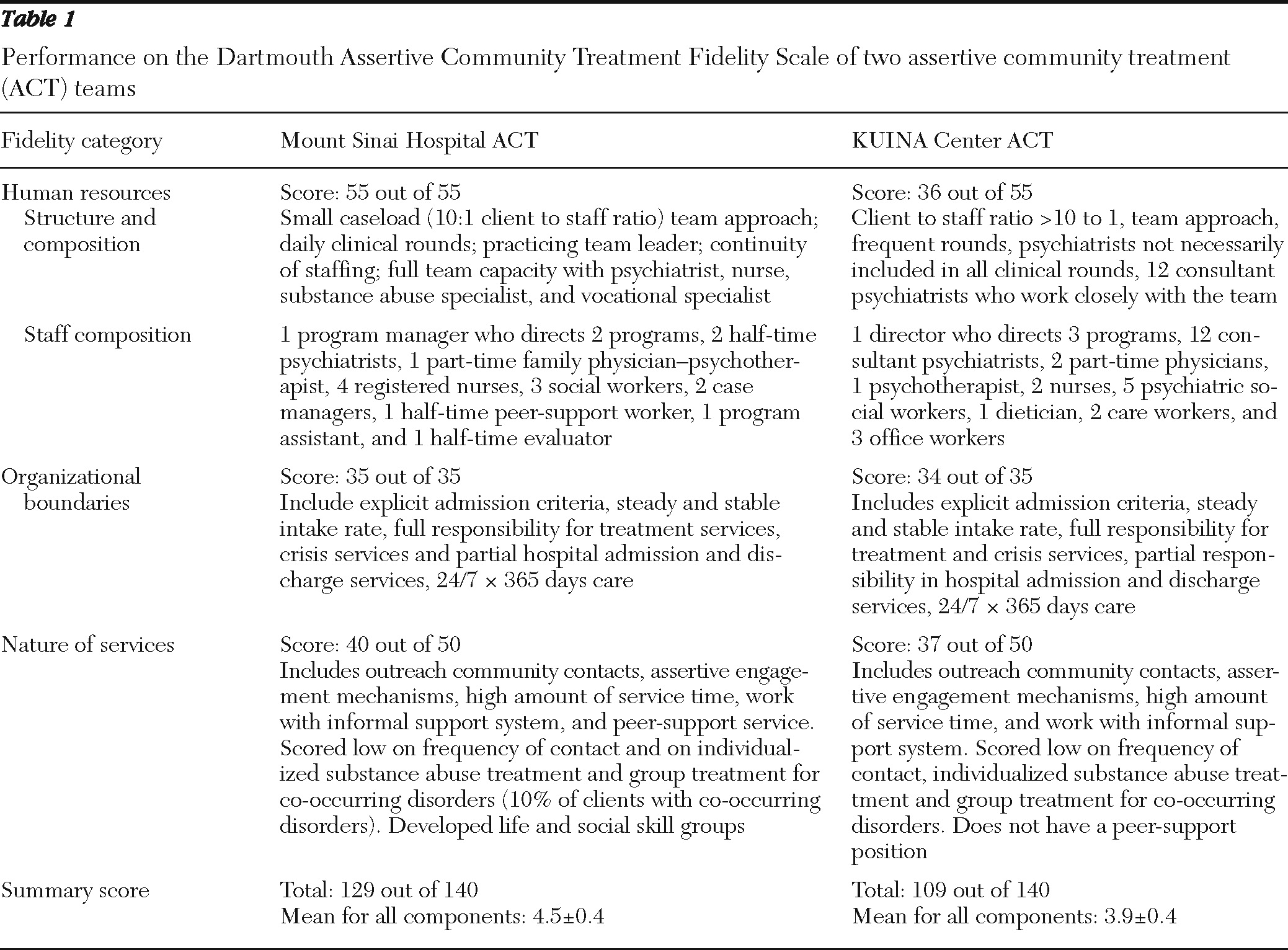
Table 1 summarizes highlights of the evaluation of the teams' fidelity to the standard ACT model. Mount Sinai Hospital ACT scored 4.5 and KUINA ACT scored 3.9 on the Dartmouth Assertive Community Treatment Fidelity Scale, indicating that both teams conformed to the basic ACT model.
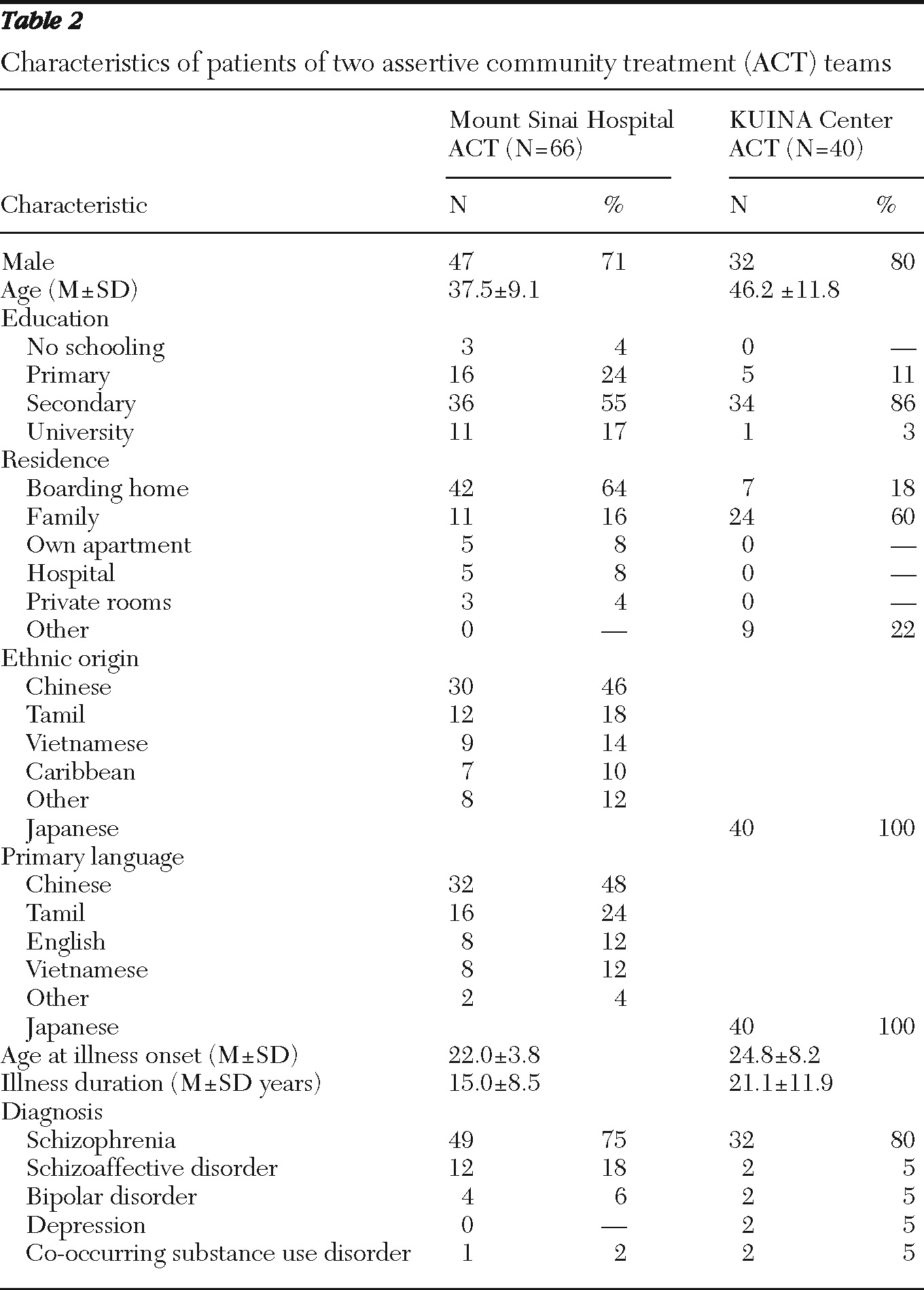
Demographic characteristics were largely similar in both client groups (
Table 2). However, the KUINA ACT clients were far more likely to live with their families, in contrast to the high rate of residence in boarding homes among the Mount Sinai Hospital ACT clients. Sixteen percent of Mount Sinai ACT patients lived with their families, compared with 60% of KUINA ACT patients. In addition, the Mount Sinai ACT sample was widely divergent ethnically and in languages spoken, compared with the homogeneous KUINA ACT sample. Rates of co-occurring substance use disorders were relatively low in both samples.
DSM-IV-TR diagnostic profiles were very similar between the groups.
There were several key differences in the two programs. Mount Sinai ACT serves a heterogeneous urban immigrant patient population of Chinese, Tamil, Korean, Vietnamese, Afro-Caribbean, and Aboriginal patients, whereas KUINA ACT serves a homogeneous Japanese population. Mount Sinai ACT clients must search for culture- and language-appropriate accommodations, and they encounter long waiting lists for program placements. KUINA ACT patients have more stable housing situations and easier, more rapid access to sheltered workshops and day care programs because many of these services are colocated within the KUINA Center. Mount Sinai ACT has established 233 formal and informal collaborations with community agencies, individuals, and services to meet the needs of patients, reflecting fragmentation of community services in Toronto. KUINA ACT has many of these services in one integrated, accessible location.
For Mount Sinai ACT clients, the mean reduction in hospital days was 78%; in the year before admission the mean number of hospital days was 97, compared with 21 in the year after. For KUINA ACT, the mean±SD reduction in hospital days was 72%±48%: 60±115 in the year before admission and 17±60 in the year after. In terms of total admissions, the reduction was 57% for Mount Sinai ACT (from 104 to 45 admissions), and 57% for KUINA ACT (from 14 to eight admissions). The mean reduction in the number of clients with at least one admission was 56% for Mount Sinai ACT (from 52 to 23 clients) and 50% for KUINA ACT (from 14 to seven clients).
BPRS scores significantly decreased from pre- to postadmission. For Mount Sinai ACT patients, scores decreased from 57±20 to 45±6, a change of −12 (p<.001). For KUINA ACT patients, scores decreased from 58±22 to 47±3, a change of –12 (p<.005).
Ratings of satisfaction by clients and families in the “satisfied” and “very satisfied” categories were high in both Toronto (45 clients, 91%, and 14 family, 100%) and KUINA (40 clients, 95%, and 20 family, 90%), indicating that the ACT model was perceived as acceptable and helpful in both populations.
Discussion
The original ACT model as conceived in Madison, Wisconsin, was not designed for patients from nonwhite ethnocultural groups. However, the favorable clinical outcomes found in this study are comparable if not superior to those reported in North American and European studies (
1,
2), suggesting that ACT is effective in both the diverse ethnocultural setting in Toronto and the homogeneous ethnocultural setting in Japan.
Both ACT teams achieved over 90% satisfaction levels. This is an important finding in light of reports that some patients, patient advocates, and other critics consider North American ACT too authoritarian, believing it interferes with clients' treatment and rehabilitation choices (
13). The Toronto and KUINA populations may have embraced ACT services because they are culturally appropriate and much needed.
Consistent with Japanese tradition, the study found that a large percentage of KUINA ACT patients resided with their families. Under the Japanese Mental Health Act, families are designated as custodians of their family members with mental illness (
11). However, although a high level of family support and involvement is helpful, it can also lead to increased burden for family members (
11). In contrast, when patients live with their families in Ontario, their financial support from the government-funded Ontario Disability Support Program is reduced (
14). The important role of family in patient care warrants greater study in different cultural settings (
15).
Both teams face challenges in collaborating with other service providers and creating a supportive community environment for patients with serious mental illness. KUINA ACT, as a community-based service agency, must collaborate with private hospitals in the area and create an effective interface with other community stakeholders. Mount Sinai ACT has a more fluid relationship with hospital care, but the program is challenged in the area of hiring skilled and culturally competent staff who can assist patients in dealing with issues of stigma, discrimination, and racism in the community and in the mental health system. Another challenge for the Toronto team is in establishing formal and informal collaboration with community agencies to meet the needs of ethnocultural clients who do not fit easily into mainstream services.
A final consideration in adapting the ACT model internationally is how it is to be funded. Mount Sinai Hospital ACT is supported entirely by the government, and KUINA ACT is funded through a mixed model of government and local community resources. Our findings suggest that both models perform well as long as the funding is adequate and sustained over time. An adequate social welfare system and the availability of other community resources, such as welfare support, housing, and shelters, are also crucial to ACT development (
15).
Conclusions
The ACT model was shown to be effective when it was adapted for a multicultural client group in Toronto, Canada, and an Asian client group in Japan. Although fidelity to core ACT elements is necessary, adaptations are also essential if the ACT model is to be optimally responsive to the specific needs of culturally diverse populations.
Acknowledgments and disclosures
The authors thank the Mount Sinai Hospital ACT team and the KUINA Center for their commitment to community outreach to those suffering with severe and persistent mental illness and acknowledge the invaluable assistance of Jack Wei and Jian Yang, M.D., Ph.D., on this project. They are especially grateful to the late Takashi Shiida, M.D., one of the founders in launching Canada-Japan ACT training in 2001.
The authors report no competing interests.