Considerable heterogeneity among persons with mental illness who have concurrent substance use disorders has been described (
1). DSM-IV distinguishes independent axis I mental disorders from substance-induced mental disorders. While differentiating dually diagnosed patients with an independent mental disorder and a substance use disorder from those with a substance-induced mental disorder has proven difficult (
2), dually diagnosed persons with independent mental disorders have been found to differ from those with substance-induced mental disorders in types of mental disorder and substance use diagnosis and in perceived treatment needs (
3–
5). For example, in one study (
5) patients with substance-induced mental disorders plus substance use disorders were more likely to have an affective disorder and to abuse cocaine than were dually diagnosed patients with independent mental disorders. We previously reported (
3) that dually diagnosed persons with independent mental disorders were more likely to be referred for mental health treatment and less likely both to receive a substance abuse treatment referral and to have received any substance abuse treatment at follow-up. However, little is known about the nature and outcomes of the treatment provided in the preceding study.
We determined whether persons with independent mental disorders plus substance use disorders who were identified at an index inpatient hospitalization differed from persons with substance-induced mental disorders plus substance use disorders at 1-year follow-up in terms of diagnosis, service utilization, quality of life, and substance use and related functional problems.
METHOD
The patients were selected from a prospective study, described extensively elsewhere (
3,
4,
6,
7), of patients consecutively admitted to two inner-city hospitals from April 1988 to December 1990. Eligible subjects were between 18 and 65 years of age. After complete description of the study to the subjects, written informed consent was obtained.
At baseline and at 1-year follow-up the following assessments were performed: 1) Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P) (
8), 2) Lehman Quality of Life Interview (
9), and 3) Addiction Severity Index (
10). The SCID-P was modified so that substance-induced mental disorders could be distinguished from independent mental disorders by assessing three aspects of the relationship between psychiatric symptoms and substance use: temporal sequence, co-occurrence, and patient perceptions (
7).
One-year follow-up was completed for 62% of the 273 patients meeting the baseline study criteria (N=168). This study included persons with assessments at both time points who had baseline diagnoses of a current independent mental disorder plus a substance use disorder (N=71) or a substance-induced mental disorder plus a substance use disorder (N=38). They were compared to single-diagnosis patients with independent mental disorders only (no substance use disorders) (N=59). The attrition rate did not differ across study groups.
Of the 168 total subjects, 57% were men (N=96), 60% were African American (N=101), 40% had never been married (N=67), and 31% had schizophrenic disorders (N=52). Their mean age was 32.7 years (SD=9.3), and they had a mean education level of 10.4 years (SD=2.4).
Group differences at baseline and follow-up were assessed with chi-square tests and analyses of variance (ANOVAs). Differences from baseline to follow-up within groups were assessed with paired t tests. Follow-up analyses were done by using the groups determined at baseline. Responses on the Addiction Severity Index and Quality of Life Interview that were rated as unreliable were omitted from the analyses. Each ANOVA group was subjected to Bonferroni adjustment to hold family-wise type I error to 0.05. F tests with significant results were followed by post hoc pairwise comparisons of mean values, performed by using Tukey's honestly significant difference, with type I error held to 0.05 for comparisons of means across all variables. The tests were two-tailed.
RESULTS
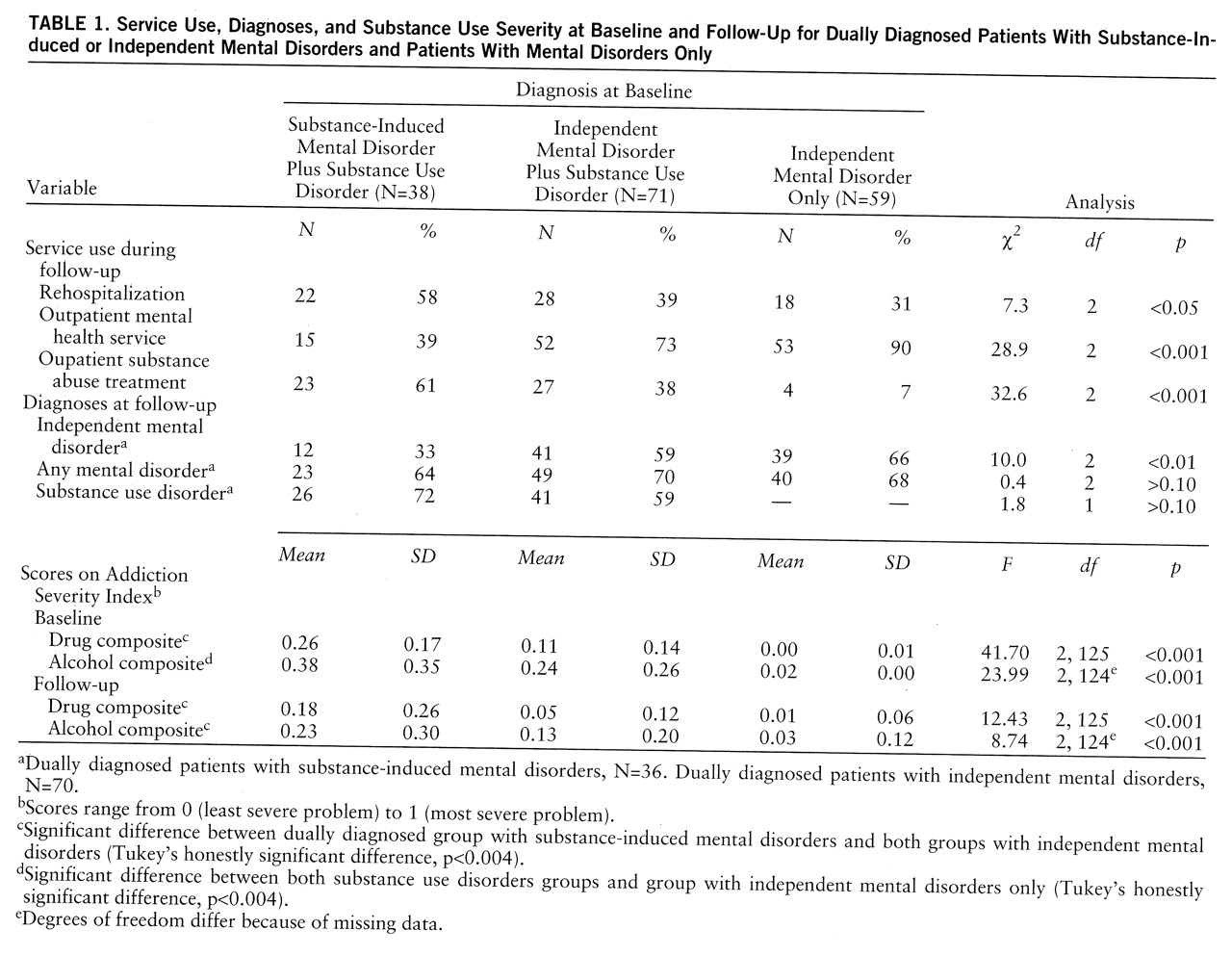
During the follow-up period, the patients with substance-induced mental disorders plus substance use disorders were significantly more likely to be rehospitalized, were less likely to receive outpatient mental health services, and were more likely to receive substance abuse treatment than were patients in either of the other two groups (
table 1).
The dually diagnosed patients with independent mental disorders at baseline were significantly more likely to have independent mental disorders at follow-up than were the patients with baseline substance-induced mental disorders. No group differences emerged in the likelihood of any mental disorder or in the rate of substance use disorders at follow-up (
table 1).
The patients with substance-induced mental disorders plus substance use disorders had worse drug severity scores at both baseline and follow-up than did the dually diagnosed patients with independent mental disorders (
table 1). The baseline scores for alcohol severity on the Addiction Severity Index did not differ significantly between the two dual diagnosis groups, but the patients with substance-induced mental disorders had worse alcohol severity scores at follow-up. The follow-up group differences disappeared when the baseline differences were controlled with analysis of covariance.
In other areas of functioning, at baseline the dually diagnosed patients with substance-induced mental disorders had significantly worse family/social composite scores on the Addiction Severity Index than did the patients with independent mental disorders only (substance-induced mental disorders plus substance use disorders: mean=0.37, SD=0.24; independent mental disorders plus substance use disorders: mean=0.28, SD=0.25; independent mental disorders only: mean=0.16, SD=0.21) (F=8.84, df=2,140, p<0.001). No other differences in medical status, employment, or psychological functioning were observed at baseline. The persons with independent mental disorders plus substance use disorders improved in scores on the Addiction Severity Index legal composite (change=0.09, SD=0.18) (t=4.00, df=63, p<0.001) and psychological composite (change=0.18, SD=0.26) (t=5.17, df=53, p<0.001) from baseline to follow-up. No follow-up group differences in quality of life or functional status were observed.
DISCUSSION
The dually diagnosed patients with substance-induced mental disorders in this study received different and perhaps more costly treatment than the dually diagnosed patients with independent mental disorders. More patients with substance-induced mental disorders were rehospitalized and received outpatient drug treatment. Fewer of these patients received outpatient mental health treatment. The greater use of drug treatment services by these persons may reflect a realization of clinician recommendations (
3). However, their greater hospital use suggests expensive crisis-oriented treatment and inattention to mental health difficulties.
Patients with substance-induced mental disorders plus substance use disorders may require more intensive dual diagnosis treatment. Substance abuse treatment is essential given that in this study such patients remained the most severely impaired in the alcohol and drug domains. The persistence of mental disorders in this group suggests that mental illness requires attention, perhaps through brief psychiatric management. The substance-induced mental disorders did not simply disappear; they recurred and required psychiatric care. The cost of intensive outpatient treatment might be offset by the cost of hospital days used by these patients.
That the dually diagnosed persons with independent mental disorders at baseline were more likely than those with substance-induced mental disorders to have independent mental disorders at follow-up suggests that this distinction remains somewhat consistent. That all groups were equally likely to have any mental disorder suggests the overall vulnerability of these individuals to the chronicity of mental illness, albeit in different forms.
This study is limited by the nature of the original study group and the attrition experienced at follow-up. These weaknesses are balanced by the careful and comprehensive assessments and the prospective design. The differential outcomes of dually diagnosed persons with substance-induced mental disorders and independent mental disorders merit further study.