Although major depressive disorder in late life is a common condition (
1), effective treatments are available. In fact, the rate of recovery at 1 year is relatively high, ranging from 59% to 72%, which is similar to the rate among younger depressed patients (
2–
4). At the same time, the rate of resistance to treatment in geriatric depression has not been well-defined. There is disagreement regarding the definition of treatment resistance and what treatment should be given before a depression can be called treatment resistant (
5).
Using consensus definitions of remission, relapse, and recovery in major depressive disorder (
6), in the Pittsburgh study of maintenance therapies in late-life depression we sought to determine 1) the rate of nonremission during acute therapy and 2) the rate of relapse during continuation therapy for patients who initially have a remission but then relapse and do not recover despite vigorous treatment. By examining both of these rates prospectively, we sought to determine the frequency of resistance to treatment among elderly patients with recurrent, nonpsychotic major depression.
METHOD
Patients meeting eligibility criteria (described below) entered the study after providing written informed consent according to institutional review board procedures. Six hundred eighty-seven patients were screened, and 187 with recurrent, nonpsychotic major depression were entered into the protocol of the study of maintenance therapies in late-life depression at the Western Psychiatric Institute and Clinic, Pittsburgh, from 1989 to 1996. The subjects' mean age was 67.6 years (SD=5.8), and their mean score on the 17-item Hamilton Rating Scale for Depression (
7) was 22.2 (SD=4.2). The study group was 74.9% female and 93.0% Caucasian, and 81.2% of the subjects had had 12 or more years of education. Their mean age at onset of lifetime depression was 48.2 years (SD=16.7), the mean number of prior episodes was 4.9 (SD=4.5), the mean interepisode period of wellness was 13.4 months (SD=10.2), and the median duration of the current episode was 18.3 weeks. One hundred eighty patients actually began treatment, since five patients had spontaneous remissions and two refused treatment. All subjects were required to have recurrent unipolar major depression (nonpsychotic) as determined by a semistructured interview with the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (
8), a score of 17 or higher on the 17-item Hamilton depression scale (
7), and a score of 27 or higher on the Mini-Mental State examination (
9). The 500 patients who were excluded from the study had other psychiatric diagnoses (N=135), major depressive disorder, single episode (N=119), an interepisode wellness interval greater than 2.5 years (N=63), medical contraindications for use of nortriptyline (N=43), or delusional (N=24) or intermittent (N=23) depressive disorders; or they did not meet the study age criteria (N=12), were currently in psychiatric treatment or desired immediate treatment (N=20), were in remission (N=13), did not have a psychiatric diagnosis (N=20), did not want to make the time commitment (N=11), or had too brief a remission between episodes (N=1); or they were excluded for other miscellaneous reasons (N=16). At study entry all patients were further evaluated with the Interpersonal Support Evaluation List (
10), the Brief Symptom Inventory anxiety scale (
11), and the Cumulative Illness Rating Scale (to estimate concomitant medical burden) (
12).
Diagnosis of episodes of major depression is the responsibility of our clinical research center's Clinical Core, which uses a structured interview and best-estimate consensus approach to determine diagnosis. The Clinical Core is also responsible for ensuring high levels of interrater reliability on Hamilton depression scale scores (intraclass correlation coefficient=0.89), on the assessment of medical comorbidity, and on other outcome measures.
The subjects received nortriptyline titrated to plasma steady-state levels of 80–120 ng/ml (mean level=89.8 ng/ml, SD=25.7, and mean dose=78.7 mg/day, SD=32.4, at steady state). A mean of 5.4 weeks (SD=4.1) was required for achieving the 80-ng/ml threshold concentration. By design, during acute therapy patients participated in weekly clinic visits, and they received at least 12 interpersonal psychotherapy sessions focusing on issues of bereavement, role transition, or interpersonal conflict as the primary interpersonal psychotherapy problem (
13). The mean duration of acute treatment for patients whose depression remitted was 13.7 weeks (SD=7.2), but for patients whose response trajectories were slow, brittle, or partial, acute treatment was extended to 26 weeks. Along with nortriptyline, adjunctive medications were given to enhance response to treatment (lithium, perphenazine, paroxetine, methylphenidate, or lorazepam) or to alleviate medication-induced side effects (bethanechol for urinary retention, laxatives for constipation) (
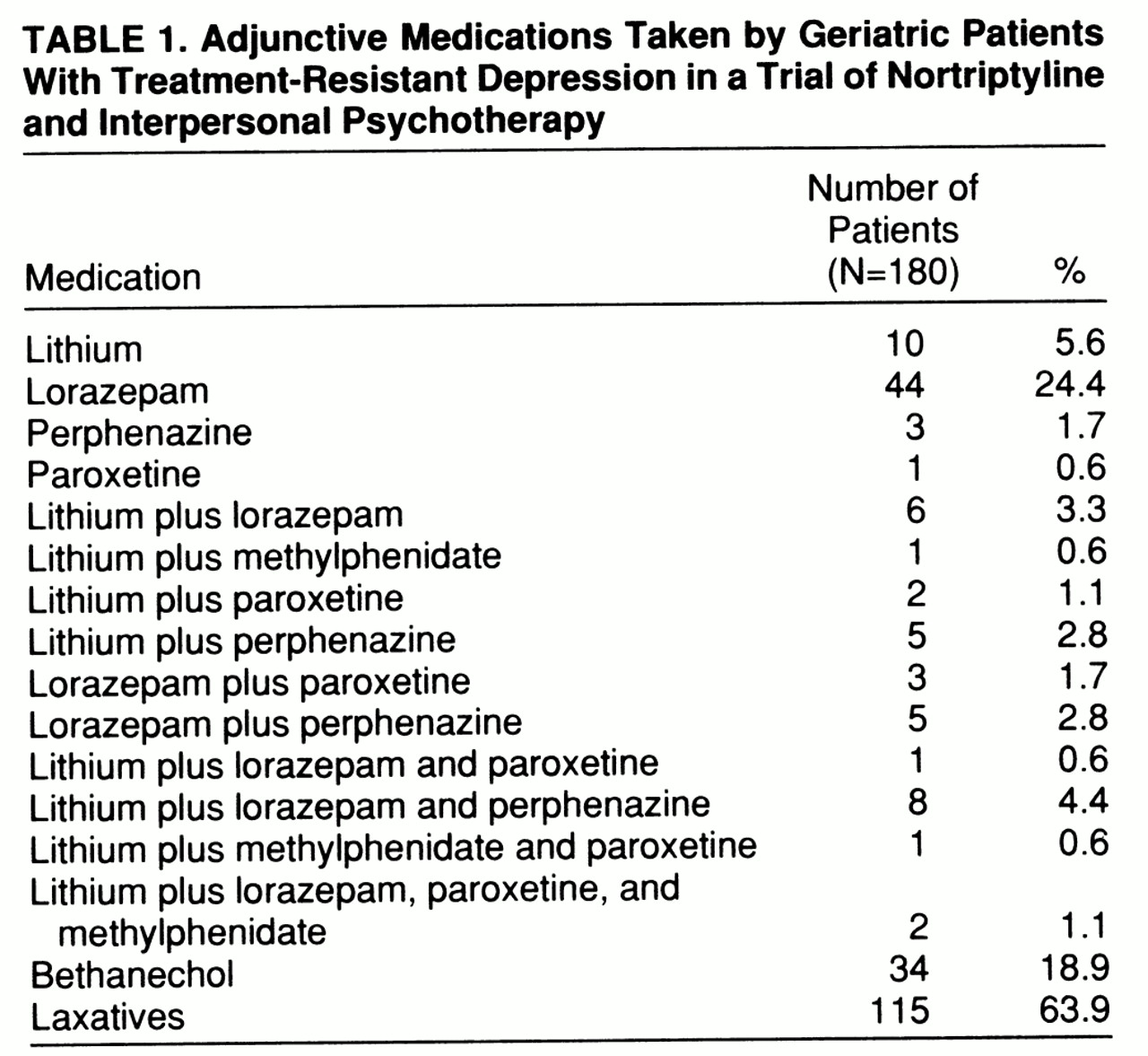
14).
With respect to treatment outcome measures, we followed the convention of Frank et al. (
6) for defining remission, recovery, and relapse. Specifically, when patients achieved a score of 10 or less on the Hamilton depression scale for 3 consecutive weeks during acute therapy, their index episode was declared to be in remission. Partial remission was defined by a Hamilton depression score of 11–14 at the end of acute therapy. Relapse was defined as the reappearance of depressive symptoms in sufficient numbers and duration to meet the SADS criteria for a current major depressive episode. After acute therapy, a 16-week period of continuation therapy began, during which patients received the same dose of nortriptyline used during acute therapy and twice-monthly interpersonal psychotherapy. After completing continuation therapy, patients were declared to be in recovery as long as they had not experienced a relapse into a major depressive episode. Patients who relapsed while in continuation therapy reentered the acute treatment phase. Resistance to treatment was defined as lack of recovery despite completion of treatment. Thus, treatment resistance included both subjects who did not achieve remission with acute therapy and those who relapsed during continuation therapy and were not restabilized.
In the data analysis, a total of 12 demographic and clinical characteristics of recovered and nonrecovered patients were compared. Categorical variables were examined with chi-square analysis or Fisher's exact test, as appropriate, while continuous variables were examined with t tests.
RESULTS
Twenty-one patients dropped out during acute therapy, and seven during continuation therapy. Reasons for dropout included treatment refusal (N=13), other medical problems (N=6), noncompliance (N=4), side effects (N=2), delusions (N=1), death from myocardial infarction (N=1), and other diagnosis (bipolar disorder, N=1). Among the patients who completed acute treatment (N=159), there were 19 who did not respond, a rate of 11.9% (95% confidence interval=6.9–16.9). In addition, some of the patients who had responded initially relapsed during continuation therapy and did not recover (N=9). Thus, the frequency of treatment resistance, defined as not achieving recovery, was 18.4% (28/152, i.e., 19 patients who did not respond during acute therapy plus nine who relapsed during continuation therapy and did not recover, divided by the 180 who entered treatment minus 28 dropouts) (95% confidence interval=12.2–24.6). Of the six subjects with partial remission who entered continuation treatment, one relapsed and was not restabilized.
The demographic and clinical features of the 119 patients who fully recovered and the 28 patients who did not recover differed statistically in only two respects. First, the nonrecovered group was older than the recovered group (mean age=69.7 years, SD=5.9, and mean=67.2 years, SD=5.5, respectively; t=2.11, df=145, p<0.04). Second, marital status differed between these groups: the nonrecovered group contained more divorced or separated individuals (28.6%) than the recovered group (10.1%) (p<0.03, Fisher's exact test). In both cases, differences between the subgroup who never experienced remission (N=19) and the subgroup who fully recovered (N=119) were significant on pairwise contrasts; that is, the subjects in the subgroup with no remission were significantly older and more likely to be living alone than the group who fully recovered. The nine subjects who relapsed after initial remission were more similar in age to those whose depression never remitted, but they were equally as likely to be living with a spouse as those who fully recovered. There were no statistically significant differences between the 119 fully recovered patients and the 28 who did not recover in the comparisons on the 10 other baseline demographic and clinical measures we used: gender, ethnicity, education, age at onset of lifetime illness, duration of current episode, number of episodes, and scores on the 17-item Hamilton depression scale, the Interpersonal Support Evaluation List, the Brief Symptom Inventory anxiety scale, and the Cumulative Illness Rating Scale.
During treatment 51.1% (N=92 of 180) of the patients received adjunctive medications to enhance response to treatment, and 68.3% (N=123 of 180) received medications for side effects (
table 1). The rate of adjunctive pharmacotherapy was higher among patients who did not experience remission (N=17 of 19, 89.5%) or who relapsed (N=8 of 9, 88.9%) than among those who fully recovered (N=53 of 119, 44.5%) (p=0.0003 and p=0.01, respectively, Fisher's exact test). The primary interpersonal psychotherapy focus (data available for 127 patients [15]) was role transition for 40.9% of the patients, interpersonal conflict for 34.6%, grief for 22.8%, and social isolation for 1.6%.
DISCUSSION
Our estimation of resistance to treatment in geriatric recurrent major depression in the Pittsburgh study of maintenance therapies in late-life depression was 18.4%. This prospective determination rests on the definition of treatment resistance as inability to achieve recovery from the episode of depression despite completion of treatment. This study provided a unique opportunity to examine the frequency of treatment resistance, since two key groups could be identified: 1) patients whose depressive episodes did not remit during acute therapy and 2) those whose episodes remitted with acute therapy but who relapsed during continuation therapy and then did not recover. Our aggregate estimate of treatment resistance included both of these groups who did not achieve recovery.
We compared our observed rate of resistance to treatment in elderly depressed patients with the rates in two other large naturalistic studies, after adjusting estimates of treatment resistance to rates per 100 person-years and including dropouts. We divided the number of subjects with treatment-resistant depression by the total time in years that all subjects were in treatment (acute and continuation). This value was then multiplied by 100 to obtain a rate of treatment resistance per 100 person-years. Thus, in Hinrichsen's study of elderly patients initially hospitalized for major depressive disorder (
2), follow-up at 1 year after naturalistic treatment yielded 28% who had not recovered and another 13% who had initially responded but then relapsed (41 cases per 100 person-years). Alexopoulos and colleagues (
4) found that 26% of patients had not recovered at 1 year (26 cases per 100 person-years), while within 2 years 23% had not recovered. Converting our rate of treatment resistance with use of the formula we have described yields a rate of 28.9 cases per 100 person-years. Differences in severity of illness between study groups (e.g., Hinrichsen's study included only hospitalized patients) may account for the different rates of treatment resistance seen in these three studies.
There are several constraints on the generalizability of our findings. First, only geriatric patients with recurrent, nonpsychotic unipolar major depression were included in the study. Second, patients with psychosis or cognitive impairment (Mini-Mental State score <27) were excluded. Third, the study group was mostly female and relatively homogeneous ethnically. Also, while the group included patients who were hospitalized at some time during their treatment, the majority of the participants were outpatients throughout the entire study. On the other hand, the Pittsburgh study of maintenance therapies in late-life depression did provide structured diagnostic assessments with long-term follow-up of diagnostic stability, standardized treatment, prospective documentation of treatment response (or nonresponse) with predetermined criteria, monitoring of treatment compliance through plasma drug levels, and a relatively large study group size, thus providing a rigorous examination of treatment resistance in geriatric depression. In addition, more than one-half of our patients received nortriptyline augmented by at least one other agent. The frequent need for adjunctive medication may suggest that our patients were more complex than, and not representative of, individuals with major depression found in other settings such as primary care. Our experience also indicates the complex nature of treating late-life depression. The fact that the study was carried out in a university center known for depression research may have resulted in attracting individuals whose depression is more difficult to manage, which is typical of individuals who come to a specialized treatment center. Our experience underscores, therefore, the need for specialist involvement in the care of individuals who do not respond to standard treatment regimens.
The demographic and clinical features of the recovered and treatment-resistant groups in our study were quite similar except for age and marital status. Although the mechanisms are unclear, the modestly greater age of the nonrecovered group may indicate a biological vulnerability, while the difference between groups in marital status highlights the importance of psychosocial factors in treatment outcome.
Although a previous report (
16) indicated that age at onset of lifetime depression before 50 years may be associated with resistance to treatment, the age at onset in our study did not differ significantly between groups. In contrast to another report suggesting that nonresponders were more likely to have a longer index episode of depression and higher baseline anxiety (
17), we found no such differences. Overall, the striking similarity between our two groups with regard to demographic and clinical features suggests that the mechanisms underlying treatment resistance in our study may have been due to other unmeasured biological variables (such as genetic factors or pharmacodynamic effects) or to unmeasured psychosocial variables (including severe life events).
In summary, by defining resistance to treatment as lack of remission with acute therapy or relapse during continuation therapy and subsequent lack of recovery, and by examining the frequency of resistance to treatment prospectively, we were able to provide a clinically relevant estimate of treatment resistance in recurrent, nonpsychotic geriatric depression. Because the study allowed acute combined treatment of up to 26 weeks with an antidepressant prescribed to achieve specified steady-state levels, as well as weekly interpersonal psychotherapy and pharmacologic augmentation when necessary, and because the study strongly emphasized compliance with the therapy regimen, it provided very intense, sustained treatment. Future research is needed to increase understanding of the underlying mechanisms of resistance to treatment and to improve therapeutic options.