Involvement of the soluble intercellular adhesion molecule 1 (ICAM-1) in the disturbance of the blood-brain barrier in schizophrenia was observed in an earlier study by us
(1). ICAM-1 is a part of the receptor-ligand system that mediates the penetration of cells through the blood-brain barrier. Adhesion molecules are expressed on endothelial cells, and the expression is promoted by activating cytokines, levels of which have been found to be higher than normal in the CSF of schizophrenic patients
(2,
3). Vascular cell adhesion molecule 1 (VCAM-1), the ligand of very late antigen 4 (VLA-4), and ICAM-1, the ligand of lymphocyte-function-associated antigen 1 (LFA-1), are also expressed on astrocytes, microglial cells, and neurons
(4). The ICAM-1/LFA-1 and VCAM-1/VLA-4 systems promote accumulation of activated lymphocytes in the vessels of the target organ, and they also promote diapedesis through the endothelium into the parenchyma
(5). Moreover, it has been suggested that neuroleptics affect the blood-brain barrier
(6). Therefore, we investigated the expression of adhesion molecules on lymphocytes in patients with schizophrenia, the effects of antipsychotic treatment, and the relationship to the blood-brain barrier.
METHOD
In a prospective study we examined 45 schizophrenic patients (13 female, 32 male), diagnosed according to the criteria of DSM-III-R by the Structured Clinical Interview for DSM-III-R (SCID)
(7). All of the patients were inpatients, and each underwent a medical and neurological examination. In addition to a diagnosis of schizophrenia, the inclusion criteria were written informed consent, acute illness, and absence of other disorders. The mean age of the 45 included patients was 31 years (SD=9, range=18–55).
The majority of the patients had not been treated with neuroleptics for at least several months, and 16 had never received neuroleptics. The mean duration of illness was 54.5 months (SD=77.9, range=6–300).
Of the 45 patients, 22 (eight female, 14 male) were reexamined before being discharged; their ages ranged from 22 to 44 years (mean=31, SD=6). Their duration of treatment ranged from 1 to 4 months (mean=2.6, SD=1.8). Treatment included butyrophenones, phenothiazines, thioxanthenes, clozapine, and other atypical neuroleptics according to naturalistic clinical conditions.
A comparison group of 41 healthy volunteers (18 female, 23 male) aged 20 to 53 years (mean=29, SD=8) was also examined.
A lumbar puncture was performed if clinically indicated. A lumbar puncture is performed in the hospital during a detailed organic examination of first-episode schizophrenic patients and patients who have not previously undergone a full organic examination during the course of the disorder. Of the 45 schizophrenic patients, 32 (12 female, 20 male) underwent a lumbar puncture. Their mean age was 31 years (SD=10).
Blood drawing and lumbar puncture were performed between 9:00 a.m. and 11:00 a.m. Peripheral blood mononuclear cells were separated by Ficoll density gradient centrifugation and stored in liquid nitrogen.
Lymphocyte subsets and the expression of activation markers were analyzed by specific monoclonal antibodies. The following monoclonal antibodies were used for single-, two-, and three-color analysis, respectively: CD4, CD8; LFA-1 (CD11a); and VLA-4 (CD49d); mouse IgG1-fluorescein isothiocyanate or phycoerythrin was used as an isotype control. Forward and right-angle scatter were used to gate on lymphocytes for the analysis of subsets. The cell numbers were calculated as the percentage of peripheral blood lymphocytes.
CSF was analyzed to determine the content of total protein, albumin, and IgG and the quotient of CSF albumin divided by serum albumin. Albumin and immunoglobulin were determined by immunonephelometry (Beckmann, Munich). CSF reference values were chosen according to the literature
(8).
For statistical analysis, Student’s t test for independent samples or the Mann-Whitney U test was used to compare the cell numbers of the comparison subjects with those of the patients. The paired Student’s t test was used to compare the values of the schizophrenic patients before therapy and after improvement.
RESULTS
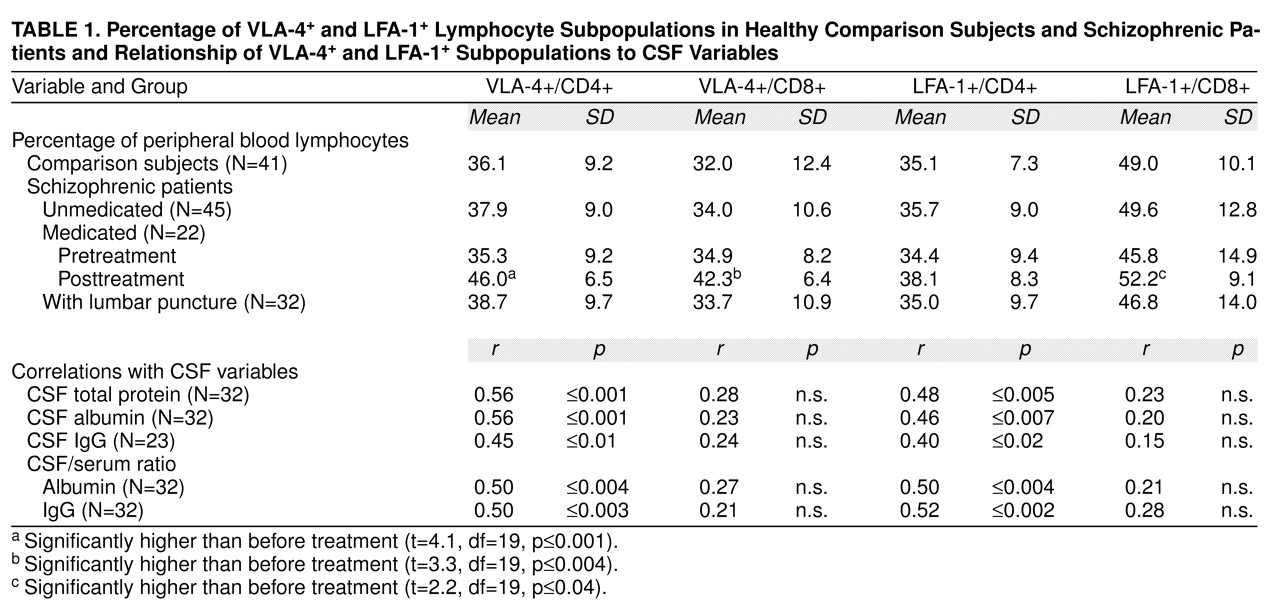
Lymphocyte subpopulations for the comparison group, the unmedicated and medicated schizophrenic patients, and the patients who underwent lumbar puncture and results regarding the relationship between CSF results and adhesion molecule expression are shown in
table 1.
After treatment, the schizophrenic patients had significantly higher values for VLA-4+/CD4+ cells (t=5.1, df=59, p≤0.0001) and VLA-4+/CD8+ cells (t=4.5, df=59, p≤0.0001) than those found for the comparison group.
To examine the differential influence of neuroleptics on the immune measures, the patients were divided into four treatment groups: butyrophenones, phenothiazines, clozapine, and other atypical neuroleptics. No differential influences of the drugs were found.
The mean values of the CSF variables were within their normal ranges: albumin, 20.2 mg/100 ml (SD=6.3); IgG, 2.5 mg/100 ml (SD=1.0); CSF/serum ratio of albumin, 4.8 (SD=1.5); and CSF/serum ratio of IgG, 2.3 (SD=0.8). High total protein levels were observed in three patients (9%), and a high CSF IgG level was found in two patients (6%).
A disturbed blood-brain barrier, as indicated by an age-corrected CSF/serum albumin ratio greater than 7.4, was found in six (19%) of the 32 patients.
We separated the patients into two groups according to whether they had a damaged blood-brain barrier or not. As regards the CD4+ cells, the patients with disturbed blood-brain barriers had higher values for both LFA-1+/CD4+ cells (Mann-Whitney test, z=2.8, N=32, p≤0.004) and VLA-4+/CD4+ cells (z=2.4, N=32, p≤0.02) than did the patients with intact blood-brain barriers. No difference between these groups was found in regard to the VLA-4+/CD8+ and LFA-1+/CD8+ cells.
DISCUSSION
Two findings of this study should be highlighted: the increase in the VLA-4+/CD4+ and VLA-4+/CD8+ cells during neuroleptic treatment and the relationship of the VLA-4+/CD4+ and LFA-1+/CD4+ lymphocytes to permeability of the blood-brain barrier.
The close relationships between the VLA-4+ and LFA-1+ adhesion molecule receptors on CD4+ cells, the disturbed blood-brain barrier, and the CSF content of albumin and IgG suggest that changes in these peripheral lymphocyte subtypes are associated with changes in the blood-brain barrier.
Both the ICAM-1
+/LFA-1
+ and the VCAM-1
+/VLA-4
+ pathways are involved in adhesion of lymphocytes, permeability of the blood-brain barrier, and penetration of cells into the parenchyma
(5). It seems that in schizophrenia, CD4
+ cells of both pathways are involved in blood-brain barrier permeability.
There are indications of defective presentation or recognition of antigens, or both, in schizophrenia
(9). Our results suggest that treatment with neuroleptics is associated with an increase of the VLA-4
+molecule on T lymphocytes. Since VCAM-1 and VLA-4
+ act as co-stimulatory signals in antigen recognition
(10), the increase of the VLA-4
+ cells may lead to improved antigen presentation or recognition and to changes in permeability of the blood-brain barrier. The latter may reflect an improvement in communication between CNS and peripheral blood.
However, other immunonological or behavioral aspects of the immune-CNS network may also be involved in the regulation of adhesion or activation, and they should be evaluated in further studies.