Lewy bodies are intraneuronal eosinophilic inclusion bodies that are seen in the brainstem and cortex of patients with Parkinson’s disease and some patients with dementia. Studies
(1–
6) have suggested that dementia with Lewy bodies accounts for 10% to 25% of dementia cases in clinical populations. An international meeting developed operationalized clinical diagnostic criteria
7). Key features include persistent or recurrent visual hallucinations, parkinsonism, and fluctuating confusion associated with disturbances of consciousness.
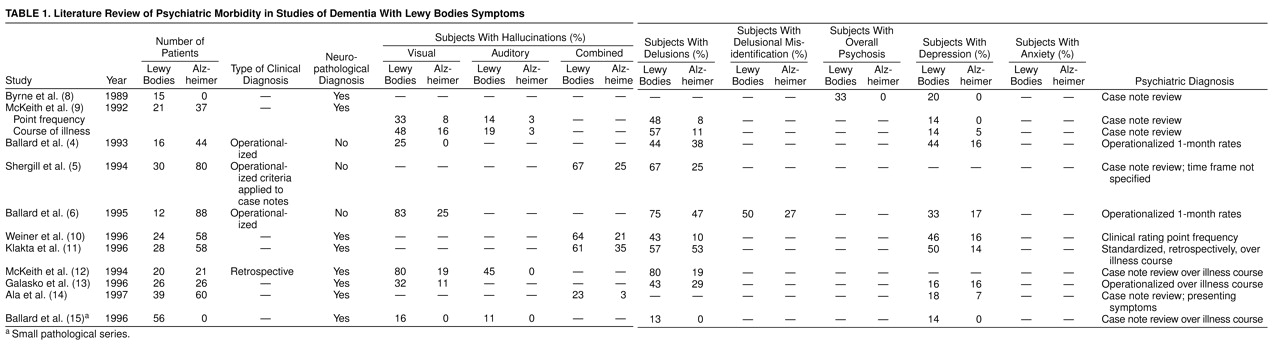
All studies have found visual hallucinations to occur significantly more frequently in dementia with Lewy bodies than in Alzheimer’s disease, although rates have varied greatly, from 25% to 83%, even when smaller studies are excluded from consideration (
Table 1)
(4–
6,
8–
15). Delusions are common in patients with dementia with Lewy bodies, with rates varying from 13% to 75%. Some groups have found delusions to have a significantly higher frequency in dementia with Lewy bodies than in Alzheimer’s disease (
Table 1)
(4–
6,
8–
15). Auditory hallucinations have received less attention, although they were described as more common in dementia with Lewy bodies than in Alzheimer’s disease by McKeith et al.
(9–
12). Rates have varied from 11% to 45% (
Table 1)
(4–
6,
8–
15). Delusional misidentification has not been studied in postmortem series, although two clinical studies found these symptoms to be common in patients with dementia with Lewy bodies
(6,
16).
The rate reported for depression has varied from 14% to 50% in patients with dementia with Lewy bodies. Using a broad clinical definition, Klakta et al.
(11) reported depression in 50% of patients with dementia with Lewy bodies. McKeith et al.
(9) reported depressive symptoms in 33% of patients with dementia with Lewy bodies, although only 14% met the criteria for major depression, whereas Ballard et al. in a clinical study
(6) found that 33% of patients with dementia with Lewy bodies had DSM-III-R major depression. Depressive symptoms are common in patients with dementia with Lewy bodies, although the proportion of patients with major depression requires clarification (
Table 1)
(4–
6,
8–
15).
The rates of many important psychiatric symptoms have not been accurately determined for patients with dementia with Lewy bodies. Equally important, it is unclear whether some of these symptoms are more common in patients with dementia with Lewy bodies than in Alzheimer’s disease patients and whether they change with increasing severity. The variability of previous reports is probably accounted for by the small study group sizes, the retrospective design of many studies, the different assessment methods for psychiatric symptoms, the variable time courses of symptom ascertainment, and the biases introduced by clinical selection criteria.
The current study focused on the two largest dementia with Lewy bodies cohorts reported so far. Our aims were to examine the frequency of psychiatric symptoms among patients with dementia with Lewy bodies and to evaluate the differences in symptom profile between patients with dementia with Lewy bodies and those with Alzheimer’s disease.
RESULTS
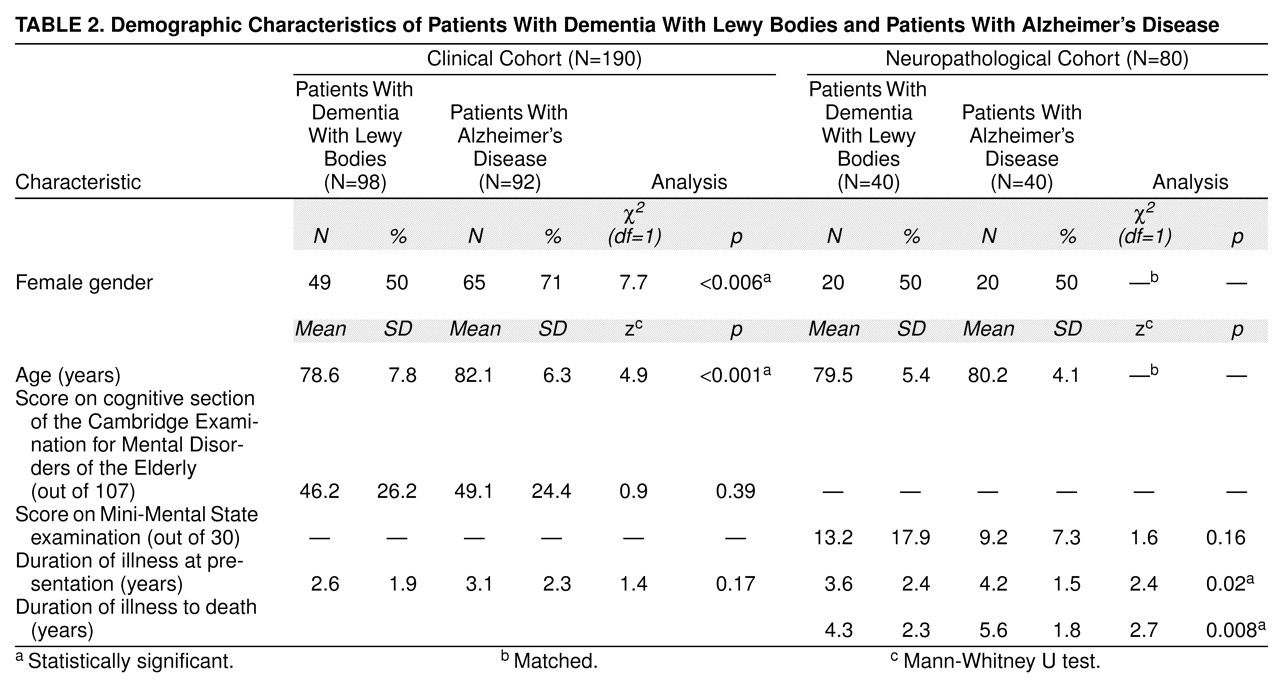
The clinical case register cohort included 337 patients with dementia, 329 of whom met the criteria for dementia with Lewy bodies (N=98), Alzheimer’s disease (92 probable, 74 possible), or vascular dementia (N=65). Only the patients with probable dementia with Lewy bodies or probable Alzheimer’s disease were considered in the present study. The neuropathological series included 40 patients with dementia with Lewy bodies who were compared with 40 Alzheimer’s disease patients matched by age and gender. Their demographic characteristics are described in
Table 2. The patients with dementia with Lewy bodies in the clinical cohort were more likely to be male and were significantly younger. The patients in the neuropathological cohort were matched for these variables, but the Alzheimer’s disease patients were significantly more cognitively impaired and had a longer illness duration (
Table 2).
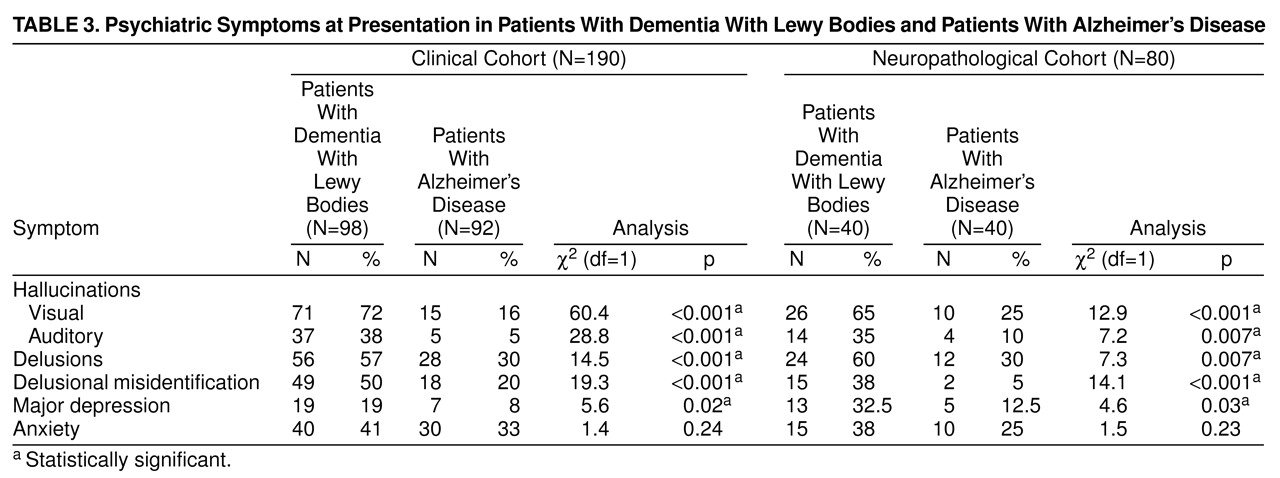
At presentation, visual and auditory hallucinations, delusions, delusional misidentification, and depression were significantly more common in patients with dementia with Lewy bodies, in both the clinical and neuropathological cohorts. The rates of individual symptoms are shown in
Table 3 and are similar in the two study groups, apart from the lower frequency of depression in the clinically diagnosed patients. Most psychiatric symptoms had rates exceeding 30% in patients with dementia with Lewy bodies from the clinical cohort, with visual hallucinations occurring in more than 70% of the patients. The two dementias showed the biggest differences regarding visual and auditory hallucinations and delusional misidentification.
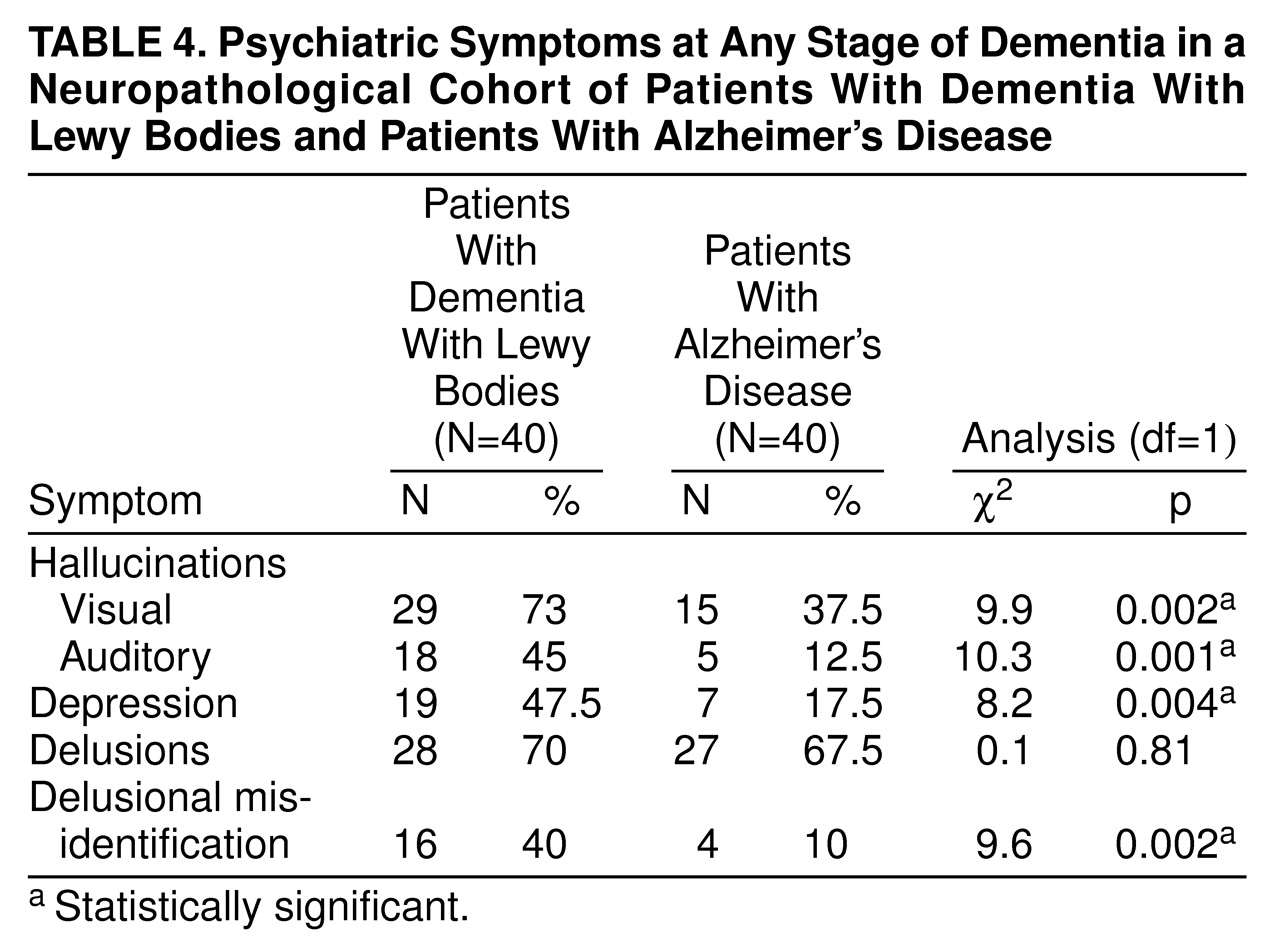
The differences in the frequency of psychiatric symptoms between patients with dementia with Lewy bodies and those with Alzheimer’s disease were less dramatic when observed over the course of the dementia, especially for delusions. That was also true for visual hallucinations, which occurred in more than 30% of Alzheimer’s disease patients over the course of the illness (
Table 4).
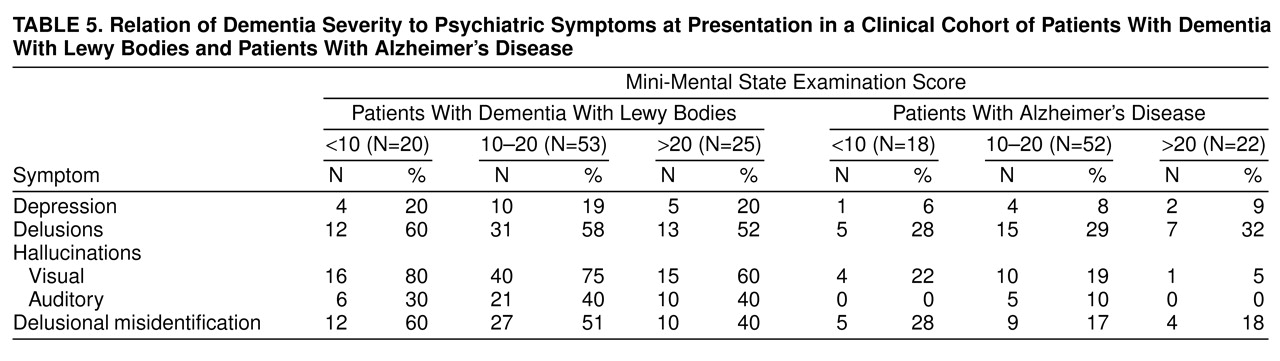
Table 5 shows the rates of key psychiatric symptoms in clinically diagnosed patients with mild, moderate, and severe dementia defined by Mini-Mental State examination cutoff scores. Most important, both auditory (0%) and visual (5%) hallucinations were extremely uncommon among Alzheimer’s disease patients scoring over 20 on the Mini-Mental State examination. Among patients with Mini-Mental State examination scores over 20, all patients with auditory hallucinations and 93% of patients with visual hallucinations had a diagnosis of probable dementia with Lewy bodies.
DISCUSSION
The strength of the current study is the combination of prospective clinical assessment with neuropathological confirmation of diagnoses in two independent but compatible cohorts with dementia with Lewy bodies.
The study confirms the high frequency of visual hallucinations (clinical cohort, 72%; neuropathological cohort, 65%), auditory hallucinations (clinical cohort, 38%; neuropathological cohort, 35%), delusions (clinical cohort, 57%; neuropathological cohort, 60%), and depression (clinical cohort, 19%; neuropathological cohort, 32.5%) at presentation to clinical services in patients with dementia with Lewy bodies. The rates are similar between the clinical and neuropathological cohorts for most symptoms except depression. The last discrepancy is not surprising given the higher mortality rates of depressed dementia patients
(31).
Visual and auditory hallucinations, delusions, and depression all occurred at significantly higher rates in patients with dementia with Lewy bodies than in Alzheimer’s disease patients. The presence of visual or auditory hallucinations in patients with Mini-Mental State examination scores greater than 20 was even more suggestive of dementia with Lewy bodies, which may have important implications for early diagnosis. Patients with hallucinations early in the course of their dementia are also a key group for intervention studies aiming to reduce the severity, persistence, and distress of these symptoms as well as preventing the expedited institutionalization that often ensues.
When symptom rates across the course of the dementia were calculated, the magnitude of difference between dementia with Lewy bodies and Alzheimer’s disease patients diminished. This is supported by previous work, where the differences in frequency of psychiatric symptoms for dementia with Lewy bodies and Alzheimer’s disease patients are more substantial in studies evaluating point or 1-month rates (
Table 1). Although a good psychiatric history is important and will more accurately identify a particular symptom over the course of an illness, it is suggested that the differential diagnosis of dementia with Lewy bodies can be made more accurately by focusing on symptoms over the month before presentation. This is particularly true for delusions, reflecting the tendency of Alzheimer’s disease patients to experience brief delusional episodes
(32).
Alzheimer’s disease patients in the clinical cohort were older and more likely to be female, whereas Alzheimer’s disease patients in the neuropathological cohort had more severe cognitive impairment and a longer duration of illness. Each of these factors may have elevated the relative frequency of some psychiatric symptoms, although the confounding effects would operate in the opposite direction from the current findings. Because patients from the clinical cohort met the clinical diagnostic criteria for dementia with Lewy bodies, it is possible that the reported rates of visual hallucinations may have been elevated by selection biases. However, the magnitude of difference was similar in the neuropathologically diagnosed patients.
Both cohorts reported in the current study showed significantly higher rates of depression with dementia with Lewy bodies than with Alzheimer’s disease. Five out of six previous studies have reported higher rates of depression in patients with dementia with Lewy bodies (
Table 1), although many of the study groups have not been large enough to demonstrate statistically significant differences. This is consistent with the current study, where the effect size was less substantial than for psychotic features.
Delusional misidentification and anxiety have received little previous attention. Anxiety was common in both patients with dementia with Lewy bodies and those with Alzheimer’s disease. However, delusional misidentification was substantially more common in patients with dementia with Lewy bodies and may also be of diagnostic importance.
Given the high frequency of psychiatric symptoms in patients with dementia with Lewy bodies, developing safe and effective treatments is a priority but depends on understanding treatment mechanisms. Perry et al.
(33) identified a strong association between visual hallucinations in patients with dementia with Lewy bodies and the severity of cholinergic depletion in the temporal cortex, a finding supported by parallel work with Alzheimer’s disease, suggesting that anticholinesterase inhibitors may improve psychosis
(34).
The mechanisms underlying other psychiatric symptoms have received less attention. A pilot study
(35) suggested a link between the severity of parkinsonism and depression in dementia with Lewy bodies. Given the established link between depression and Parkinson’s disease, the possibility that similar mechanisms are important merits further study.
For Alzheimer’s disease, Förstl et al.
(36) suggested that relative preservation of the parahippocampal gyrus is associated with delusions. The relative sparing of medial temporal lobe structures in patients with dementia with Lewy bodies
(37) may hence predispose them to delusional phenomena. Further work needs to focus on the neurochemical correlates of preserved temporal lobe structures to inform the development of therapeutic strategies. Förstl et al.
(36) suggested that delusional misidentification may be associated with more severe neuronal loss in the hippocampus.
While there is already sufficient evidence to merit trials of treatment intervention with cholinesterase inhibitors for visual hallucinations, further work is required to understand the basis of other psychiatric symptoms.
This report confirms a significantly higher frequency of psychiatric symptoms, especially psychotic features, in patients with dementia with Lewy bodies. The finding that these differences were especially pronounced in patients with mild dementia has implications for early diagnosis and treatment.