It has been estimated that 10% of women will receive a diagnosis of PTSD in their lifetime, with one-third of illness episodes enduring longer than 60 months
(1) . In addition, data from the National Comorbidity Survey suggested that 79% of women with lifetime PTSD have at least one comorbid diagnosis
(2) . The most consistently reported risk factors for PTSD are female gender, history of an affective disorder
(3), childhood adversities, poverty, and family history of substance abuse or psychopathology
(4) . Given the high risk of PTSD in women and the chronic course of the illness, it is likely that many women experience PTSD at the time they become pregnant. To our knowledge, specific profiles of PTSD symptoms among pregnant women with and without a diagnosis of PTSD have not been prospectively examined. Similarly, no study has compared PTSD symptoms in pregnant and nonpregnant women at risk for PTSD.
Pregnancy is associated with considerable hormonal changes that might influence the expression of an illness. For example, progesterone and glucocorticoids in pregnancy have been associated with blunted memory and diminished anxiety, suggesting that an investigation of PTSD symptom profiles in pregnancy is warranted
(5,
6) . In this study, we hypothesized that pregnant women at risk for PTSD would have decreased recall of trauma and lessened hyperarousal, compared with nonpregnant women at risk for PTSD. We compared data on PTSD symptom profiles, trauma, and illness correlates from a community sample of low-income pregnant women with those from a sample of nonpregnant women who participated in the National Comorbidity Survey
(2) .
Method
Data Collection
Eligible women spoke either English or Spanish and were receiving prenatal care between February 2003 and July 2004 at any of three federally funded obstetrics clinics in the New Haven, Connecticut, area. All women receiving prenatal care were approached by a trained research assistant (master’s-level or bachelor’s-level social workers) on selected clinic days that changed weekly depending on patient flow. Screening occurred only once, at any point in the pregnancy. Participants included 948 pregnant women, constituting 91.4% of those approached. The women were a mean of 25.8 weeks pregnant when evaluated (SD=9.9, range=4.0–41.7); 12.1% (N=115) were in the first trimester, 41.0% (N=389) in the second, and 46.8% (N=444) in the third trimester. More than one-half of the women identified themselves as Hispanic (N=500, 52.7%), 32.0% (N=303) as non-Hispanic black, and 12.9% as non-Hispanic white (N=122) (2.43% identified another racial group). Written informed consent was obtained from all subjects and Institutional Review Board approval was obtained from all sites.
Research assistants administered a questionnaire that included questions on lifetime mental health diagnosis and treatment; questions on hazardous substance use; the Primary Care Evaluation of Mental Disorders (PRIME-MD) Brief Patient Health Questionnaire
(7) ; and the PTSD module from the MINI International Neuropsychiatric Interview (MINI)
(8), supplemented with an 11-question event list from the Composite International Diagnostic Interview (CIDI)
(9) . The event list was modified slightly to include a question on domestic violence, defined as “pushed, grabbed, slapped, punched, kicked, beat up, or choked by a partner or anyone else who lives with you.” The symptom criteria were evaluated for one event per respondent. Respondents who named multiple traumatic events were asked to nominate their “most upsetting” event for purposes of this study. For women with current PTSD, we did not limit our analysis to the most upsetting event. Open-ended responses that did not refer to specific events, were vague, or confounded with PTSD (e.g., depression) were eliminated. For all events, we asked the month and year when the event occurred.
A brief medical record abstraction of the subject’s prenatal chart was performed to identify any psychiatric treatment, number and date of prenatal visits, hazardous substance use, major medical illnesses, and other medical problems in current pregnancy.
Statistical Approach
For the pregnant cohort, bivariate associations between PTSD diagnosis and risk variables were computed by using the chi-square test or the Fisher’s exact test (if the expected cell size was <5) and logistic regression (proc logistic) calculated with SAS version 9.1
(10) . A multiple logistic regression analysis was constructed to describe the sociodemographic correlates of PTSD among all women. Variables entered into the adjusted model included those that were significant at an alpha level of 0.01. A separate analysis was completed with data from women who reported a traumatic event. Variables entered into the adjusted model included those that were significant at an alpha level of 0.05. Chi-square tests were used to compare PTSD symptom rates between all nonpregnant women who experienced a traumatic event from the original National Comorbidity Survey (1990–1992) cohort and pregnant women who experienced a traumatic event from our cohort.
A comparable sample of nonpregnant women from the National Cormordity Survey was selected by using the following criteria: 1) income equal to 300% of the poverty level or less and 2) living in a metropolitan or urban county as classified by the Rural-Urban Continuum Codes for Metro and Nonmetro Counties. Responses to CIDI questions referring to symptoms of PTSD occurring during the past month were examined. Rates of 1-month and lifetime PTSD and individual PTSD symptoms and traumatic events were stratified by race (white, black, Hispanic, and other).
Results
PTSD in Pregnant Women
Among the pregnant subjects, the lifetime exposure to trauma was 29.3% (N=278), with 28.4% (N=79) of subjects experiencing a trauma in the year before screening. Thirty-three (3.5%) pregnant women met the current PTSD criteria, including 11.9% (N=33) of the individuals with lifetime exposure to trauma. The most common traumatic events endorsed by the pregnant women with PTSD were sexual molestation (48.5%, N=16), other extremely stressful or upsetting event (42.4%, N=14), domestic violence (36.4%, N=12), rape (27.3%, N=9), serious physical attack or assault (27.3%, N=9), and witnessing someone being badly injured or killed (24.2%, N=8). Lifetime mental health treatment was endorsed by 51.5% (N=17) of the pregnant women with PTSD, and 24.2% (N=8) were receiving mental health treatment at the time of screening.
Comorbidity
At their prenatal visit, 66.7% (N=22) of women with PTSD met the criteria for depression, and 36.4% (N=12) met the criteria for panic disorder. Of the 33 women with PTSD, 27.3% (N=9) reported currently using alcohol or illicit drugs, and 36.4% (N=12) reported a lifetime history of illicit drug or alcohol abuse. It is noteworthy that 33.3% (N=11) of the women who met the PTSD criteria replied either “sometimes” or “more than half the days” to thoughts of self-harm.
Factors Associated With PTSD
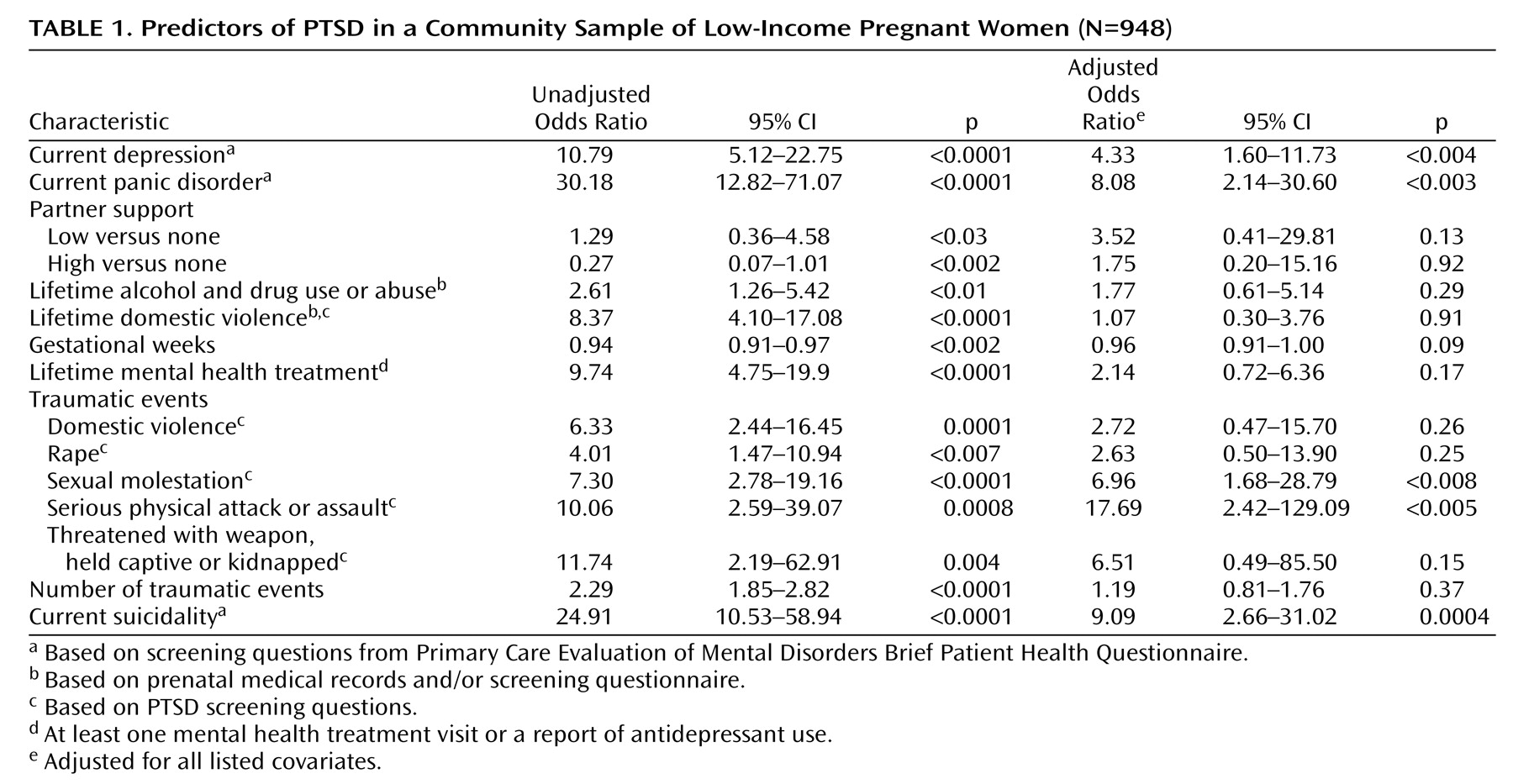
Current depression (OR=4.33, 95% confidence interval [CI]=1.60–11.73), current panic disorder (OR=8.08, 95% CI=2.14–30.60), current suicidality (OR=9.09, 95% CI=2.66–31.02), sexual molestation (OR=6.96, 95% CI=1.68–28.79), and serious physical attack or assault (OR=17.69, 95% CI=2.42–129.09) predicted a diagnosis of PTSD among all pregnant women in the study sample (
Table 1 ).
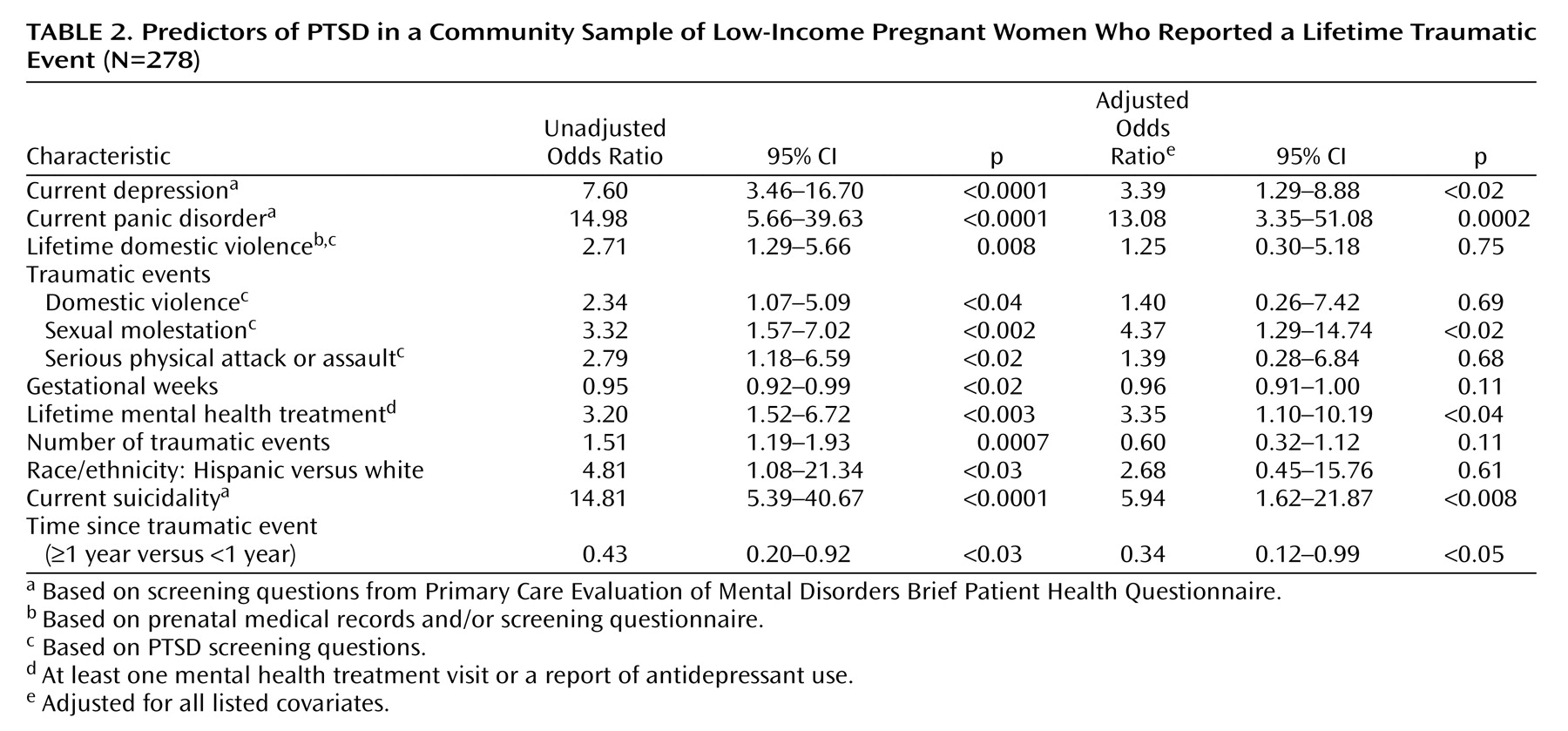
Lifetime treatment (OR=3.35, 95% CI=1.10–10.19), current depression (OR=3.39, 95% CI=1.29–8.88), current panic disorder (OR=13.08, 95% CI=3.35–51.08), current suicidality (OR=5.94, 95% CI=1.62–21.87), and sexual molestation (OR=4.37, 95% CI=1.29–14.74) predicted a diagnosis of PTSD among pregnant women who reported a traumatic event (
Table 2 ). A PTSD diagnosis was less likely in women who experienced a trauma more than a year ago (OR=0.34, 95% CI=0.12–0.99), compared to women who experienced a trauma within the last year.
PTSD Symptoms in Pregnant and Nonpregnant Women
Almost 5% (N=584) of the nonpregnant women in National Comorbidity Survey cohort experienced a trauma, and 3.9% (N=41) met the CIDI diagnostic criteria for PTSD (1-month prevalence rate). As predicted, significantly more of the nonpregnant women in the National Comorbidity Survey cohort who had experienced trauma reported reexperiencing events (i.e., dreams, intense recollections, flashbacks, or physical reactions), compared with the pregnant women in our study who had experienced trauma (79.4% [N=464] of the nonpregnant subjects, compared with 29.5% [N=82] of the pregnant subjects; c 2 =203.3, df=1, p<0.0001). Other significant differences between the two cohorts existed for the following symptoms: loss of interest (pregnant women: 54.7% [N=152], nonpregnant women: 21.1% [N=97]; c 2 =87.5, df=1, p<0.0001) and irritability (pregnant women: 64.6% [N=53], nonpregnant women: 48.5% [N=96], c 2 =6.1, df=1 p<0.02). There were no symptom differences between the two samples in sleep, concentration, event avoidance, or hyperarousal.
Discussion
These results show that PTSD is not unusual among pregnant women. In our study sample, 11.9% (N=33) of individuals who experienced a traumatic event screened positive for PTSD in pregnancy. As commonly described, PTSD is associated with a high degree of comorbidity and suicidality. It is noteworthy that 33% of the pregnant women with PTSD in this study had thoughts of self-harm and more than 27% used illicit drugs or alcohol despite their gravid state.
Fewer pregnant women (29.5%) than nonpregnant women (79.4%) reexperienced a traumatic event. To our knowledge, these are the first findings reported on the symptom profile of PTSD in pregnant women. However, studies including pregnant and nonpregnant women with PTSD in the same cohort are needed to confirm our results. These findings are consistent with the notion that elevations in hormone levels during pregnancy diminish the expression of selected symptoms of PTSD. However, indirect effects such as increased contact with the prenatal medical system could have provided support and decreased stress symptoms.
There are hazards to comparing cohorts from two different studies. Of chief concern is bias due to case misclassification. Both studies used the same event list to probe for traumatic events. However, the CIDI is a more comprehensive interview and may allow better symptom detection, hence explaining the higher endorsement of reexperiencing symptoms. On the other hand, most symptoms were not endorsed at a higher rate in the National Comorbidity Survey cohort. In fact, two symptoms were endorsed at higher rates among the women in our sample, compared to the National Comorbidity Survey cohort, suggesting that reexperiencing is selectively less frequent in pregnant women.
The rates of traumatic events (29.3%) and PTSD (3.5%) reported by the pregnant women in this study were in the ranges found among 1,224 pregnant women in Sweden (25%–28% and 2.3%, respectively)
(11) . Yet, the prevalence rate of PTSD in our study is significantly lower than the 7.7% rate reported by Loveland et al.
(12) for a cohort of 744 low-income women in Missouri and St. Louis. The discrepant finding may be due to the requirement in the previous study that respondents speak English, which resulted in a sample composed predominantly of African American and non-Hispanic white women. Our instrument was administered in English and Spanish, and more than one-half (52.7%) of the women in our sample defined themselves as Hispanic white or Hispanic black, with 40.5% speaking only Spanish. Although specific data on immigration status and country of origin were not collected in our evaluation, the majority of the Spanish speakers were recent (within the last year) immigrants to this country, and a moderate number of the African American women were also foreign born. Several epidemiological surveys have examined the effect of immigration status on the mental health status of Hispanic women and men. The largest found that, overall, the rate of any psychiatric disorder in non-Hispanic whites was almost twice that in Mexican Americans
(13) . Furthermore, the prevalence of any mood and anxiety disorder among U.S.-born Mexican Americans was nearly twice that among foreign-born Mexican Americans. A smaller study examined a subset of Mexican Americans (N=484) within the National Comorbity Survey and found that U.S.-born Mexican Americans had higher rates of PTSD than their foreign-born counterparts
(14) but were still at significantly lower risk than non-Hispanic whites. These findings may explain why our sample, which included many recent immigrants, had a comparatively low PTSD rate but still displayed comorbidity of PTSD, depression, and other poor health behaviors. Given the morbidity associated with PTSD and the association with health behaviors that affect the mother and fetus, further prospective studies that chart symptoms and explore effective treatments during pregnancy are needed.