There is accumulating evidence that maternal psychiatric disorders, including eating disorders, occurring in the postnatal period are associated with adverse effects on child development
(1 –
3) . A key way in which these disorders affect children’s development is by disrupting mother-infant interaction
(2) . Eating disorders are relatively common among women of childbearing age, affecting approximately 4% of women
(4) . The problems that these women experience have a considerable impact on the mother-child relationship and on the child. Of particular concern is the findings that by their infants’ first birthday, mothers with eating disorders are more likely to be involved in major episodes of mealtime conflict with their infants than are comparison subjects, as well as having other interactional difficulties, and that these episodes are associated with lower infant weight
(5,
6) . Two maternal responses are strongly associated with the development of such conflict: where mothers do not detect and respond to their infants’ signals and where mothers have difficulty in allowing their infants to express age-appropriate needs for autonomy through self-feeding and experimentation with food. Mealtime conflict is therefore the end product of a series of episodes of poor parental responsiveness secondary to maternal eating psychopathology centering on food and mealtimes. Furthermore, conflict in family relationships has been shown to have adverse effects on child development
(7) .
Video-feedback intervention to promote positive parenting is a relatively new treatment that has been shown to be useful in helping mothers and infants at risk
(9), although we know of no studies to date that have included mothers with psychiatric disorders
(10) . The strength of video feedback is that it provides direct access to the details of mother-child interaction, rather than relying on maternal perceptions and reports. The present study was designed to test whether such a treatment, targeted specifically at mother-child interaction, would diminish mealtime conflict by helping mothers recognize, support, and respond to infant signals and initiatives and whether it would increase infant weight and improve infant autonomy at mealtimes more than a control treatment in which mothers received counseling.
Method
Participants
Eligible participants were women ages 18–45 years with infants between 4 and 6 months old. The women met the DSM-IV diagnostic criteria for an eating disorder, either bulimia nervosa or a similar form of eating disorder of clinical severity, i.e., a bulimic subtype of eating disorder not otherwise specified
(4) . The inclusion criteria were 1) overevaluation of body shape or weight to a degree reaching clinical severity, 2) recurrent episodes of loss of control over eating (i.e., subjective or objective bulimic episodes), and 3) secondary social impairment. Mothers with severe comorbid psychiatric disorders were excluded.
In order to identify potential participants, women with infants ages 8–24 weeks attending routine postnatal baby clinics in north London and Oxford, U.K., were screened by using the Eating Disorder Examination Questionnaire
(11) (adapted for postnatal use). Informed consent was obtained for the two-stage screening procedure. Women who showed evidence of significant disturbance in eating habits and attitudes were invited for an interview using the Eating Disorder Examination
(12) . Each woman who fulfilled the eligibility criteria was invited to participate in the trial and was visited at home by a psychiatrist (A. Stein or one of two other psychiatrists), who confirmed the diagnosis by clinical interview. After complete description of the trial, written informed consent was obtained. The study was approved by the relevant local research ethics committees. The mothers were randomly assigned to the two interventions by using block randomization with fixed blocks of size six, computer generated by an independent statistician and stratified according to eating disorder diagnosis (bulimia nervosa or bulimic type of eating disorder not otherwise specified). Allocation concealment was facilitated by using sequentially numbered opaque sealed envelopes for consecutive and eligible study participants.
Interventions
Thirteen 1-hour treatment sessions were offered in the mothers’ homes beginning when the infants were between 4 and 6 months old and completed by the time the infants were 12 months old. The intervention group received video-feedback interactional treatment that was a modification of that developed by Juffer et al.
(9) . The control group received supportive counseling. This was chosen because it is an active, nonspecific intervention that does not address the mother-infant interaction directly and has been shown to be an effective therapy for mothers with difficulties in the postnatal period
(13) . In order to address the mother’s eating disorder specifically, both groups also received guided cognitive behavior self-help for eating disorders, which has been shown to be suitable for use in primary care settings
(14) . It was modified for the postnatal period and administered during half of each of the first eight sessions. As all of the therapies were nondirective, it was possible to integrate the guided self-help with the other two therapies following pilot testing. All therapies were conducted according to standardized treatment protocols.
The therapists (L.H., M.L., J.L.) were experienced in child and family mental health care and undertook project-specific training. Weekly team meetings, supervised by psychiatrists (including A. Stein, R.S.), were held to discuss the progress of therapy and to review videotapes and samples of tape recordings of the treatment sessions to ensure consistency and compliance with the protocol.
The aim of the video-feedback treatment was to prevent or reduce mother-infant conflict and enhance mother-child interaction, principally during mealtimes, by facilitating maternal recognition of and responsiveness to her infant’s cues and by improving her awareness of the infant’s developing skills and needs. The therapist videotaped the mother and infant at home during mealtimes at alternate visits. At the following visits, the therapist and mother watched and discussed extracts selected by the therapist to highlight the infant’s signals and exploration and to draw out and enhance the mother’s observational skills. The baseline assessment videotape was used in the first session; thus, seven videotapes were used in total.
Treatment comprised three stages. The first concentrated on the infant’s perspective, focusing on his or her signals (initiatives toward the mother, exploratory behavior, indications of hunger and satiety, and attempts at self-feeding). The second stage included the mother’s perspective, highlighting mother-infant initiatives, mutual responses, moments of shared emotion, and the success of sensitive, prompt reactions to infant cues. Third, as treatment progressed, the videotapes were used to help the mother identify and address potential triggers of mealtime conflict.
The counseling treatment provided the mother with support specifically for herself by means of empathetic listening. It helped the mother reflect on self-selected aspects of her life and related feelings. It aimed to encourage and support any changes she initiated, thereby developing a sense of empowerment and self-confidence.
Mothers in both groups were provided with a self-help manual, adapted for the postnatal period from two established treatments
(15,
16), that contained information about eating problems and explained the program’s six steps. The guided cognitive behavior self-help treatment aimed to help the mother regain control over her eating, reduce vomiting and laxative use, and reduce extreme concerns about shape and weight. Guided by the therapist and using the guided self-help stepwise approach, the mother was helped to implement the relevant steps.
Assessments
Assessments of the groups were undertaken before treatment, when the infants were 4–6 months old, and after treatment when the infants were age 13 months. The mothers and infants were videotaped during the principal solid meal of the day. Considerable time was allowed to help mothers feel at ease and get used to the camera at both assessments. If, in the mother’s opinion, the posttreatment meal was not typical, a further meal was videotaped on a separate occasion (six cases). All videotapes were rated by independent raters blind to group assignment (including H.W.). Investigators blind to group assignment conducted the Eating Disorder Examination interviews and the videotaping for the assessments.
Outcomes
Primary outcome
The primary outcome measure was the level of conflict during the principal meal of the day, measured every 2 minutes for the duration of the meal and averaged. Conflict/harmony was rated on a 1 (conflict) to 5 (harmony) scale
(6), on which conflict was defined as a battle for control between the mother and infant with associated infant distress, noncompliance, and invariable disruption of feeding. Key ingredients of this battle for control were a refusal to allow infant self-feeding, or to allow feeding at the infant’s own pace, and maternal concern about messiness. Infant behaviors such as repeated food refusal were common features of conflict. The occurrence of a significant conflict episode during the meal formed a dichotomous co-primary outcome measure. Such conflict was judged to have occurred if a conflict was at a severe or marked level of clinical concern (rating of 1 or 2) for any 2-minute observational period.
Secondary outcomes
A number of secondary outcomes were assessed:
Infant weight, standardized against population norms (17) . Other measurements of mother-infant interaction. These outcomes were developed from a number of sources
(5,
18) . For time-sampled rating scales, measurements were made every 2 minutes for the duration of the meal and were then averaged. First, maternal facilitation was measured on a time-sampled rating scale of 1–7. It was defined as any maternal behavior that assists the infant in an activity in which he or she is already engaged or seems ready to engage. Such facilitation requires that the mother notices what her infant is doing, or is wanting or attempting to do, and sensitively gauges when and how assistance or encouragement is needed.
The second outcome was the number of verbal responses to infant cues (appropriate and inappropriate). This measure was developed from the original sensitivity measures of Ainsworth et al.
(18) . A response was categorized as appropriate when the mother verbally responded to her infant’s cue (action, facial expression, or vocalization) in a manner congruent with that cue. The response was classified as inappropriate when the mother responded verbally to her infant’s cue in an incongruent or mismatching manner.
The third outcome, appropriate nonverbal responses to infant cues, was rated on a time-sampled rating scale of 1 (poor), 2 (moderate), and 3 (good). This measured the extent to which the mother nonverbally and congruently picked up her infant’s cues.
The fourth additional interaction outcome was the number of events of maternal intrusiveness: actions that inappropriately cut across, took over, or disrupted the infant’s activities.
Infant autonomy involving self-feeding initiatives. This was a dichotomous measure (yes/no) indicating whether the infant was allowed to self-feed with fingers or a utensil (e.g., spoon) or had access to his or her own plate of food or a joint plate.
Maternal eating disorder psychopathology, eating habits, and attitudes. The mothers were reassessed with the Eating Disorder Examination
(12) . Because eating disorders are associated with high levels of depressive symptoms, the latter were measured by using a validated questionnaire, the Edinburgh Postnatal Depression Scale
(19) .
Expectations and perceptions of treatment
The mothers’ expectations of treatment were assessed on a 1–5 scale. After treatment, maternal perceptions of treatment benefits were assessed with an 18-item questionnaire on which each item was rated from 1 (strongly disagree) to 5 (strongly agree). The questionnaire comprised four subscales: practical issues, help with eating disorder, self-esteem and feelings about self, and relationship with baby.
A number of other outcomes measured at this time were not part of our hypotheses and will be analyzed later and written up separately.
Statistical Analyses
Data from our previous study of mothers with an eating disorder showed that 59% of mother-infant pairs experienced at least one significant episode of mealtime conflict
(6) . In order to detect an anticipated 50% reduction in the number of mother-infant pairs experiencing such conflict, i.e., from 60% to 30% at a 5% significance level (two-tailed) with a power of 80%, a group size of 42 mothers in each group was required.
Descriptive and analytical statistical analyses were performed by using SPSS 11.0 for Windows (SPSS, Chicago) and Stata release 7.0 (Stata Corp., College Station, Tex.). Continuous variables were investigated for departure from normality by using the Shapiro-Wilk test, and the treatment groups were compared by means of two-sample t tests and Wilcoxon rank-sum tests, as appropriate.
For the normally distributed outcome, the child’s age- and sex-standardized weight at age 13 months, we used linear regression to estimate the direction and magnitude of the treatment effect, adjusting for the mother’s baseline eating disorder classification and the child’s standardized weight at baseline.
For dichotomous outcomes, the groups were compared by using chi-squared tests. In addition, we calculated odds ratios that were adjusted for baseline eating disorder classification and baseline measurement where applicable, using logistic regression.
In order to test the consistency of the outcomes assessments, the reliability on the video-coding measures was calculated for 20% of the subjects. Interrater reliability (weighted kappa) on the rating scale outcome measures ranged from 0.81 to 0.87. For event-sampled behaviors, the percentage concordance ranged from 77% to 94%. Both of these indicate good agreement.
Results
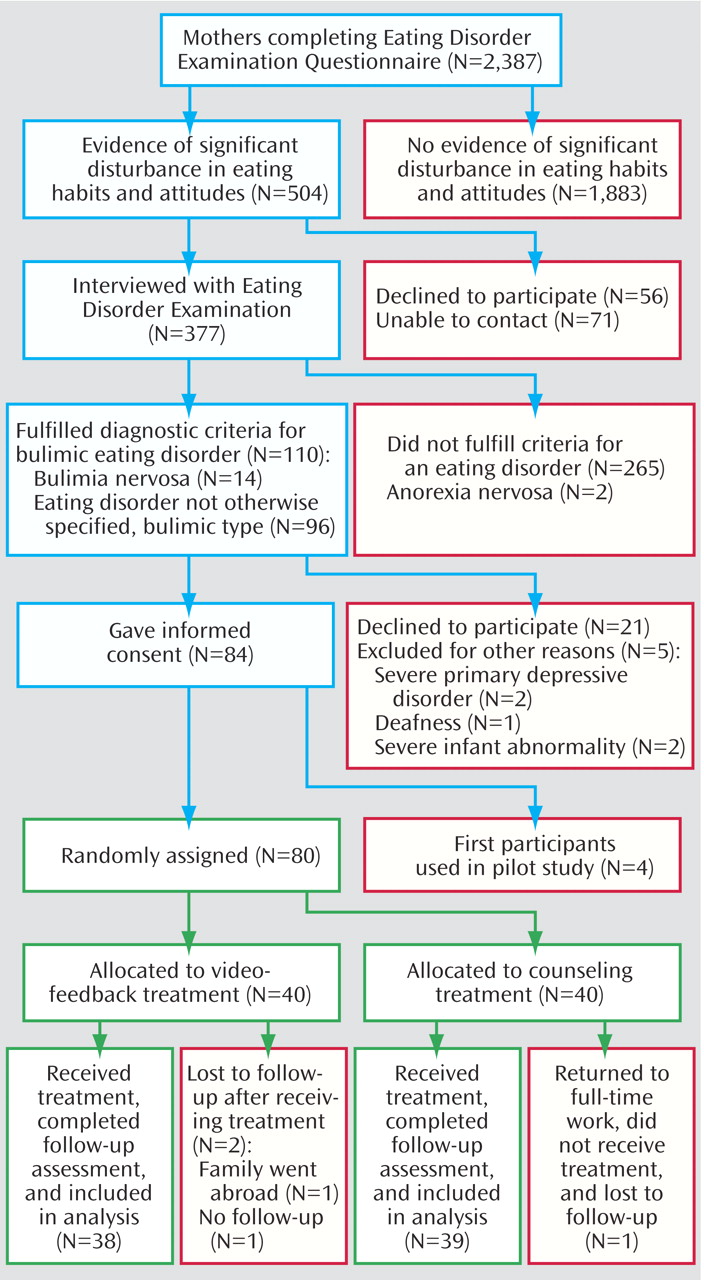
The Eating Disorder Examination Questionnaire was completed by 2,387 women, of whom 504 (21.1%) scored high and 377 (15.8%) agreed to be interviewed with the Eating Disorder Examination interview. Of these 377, 110 (29.2%) fulfilled the eligibility criteria. Ultimately, 80 women were randomly assigned to video feedback (N=40) or counseling (N=40). Participant flow is shown in
Figure 1 .
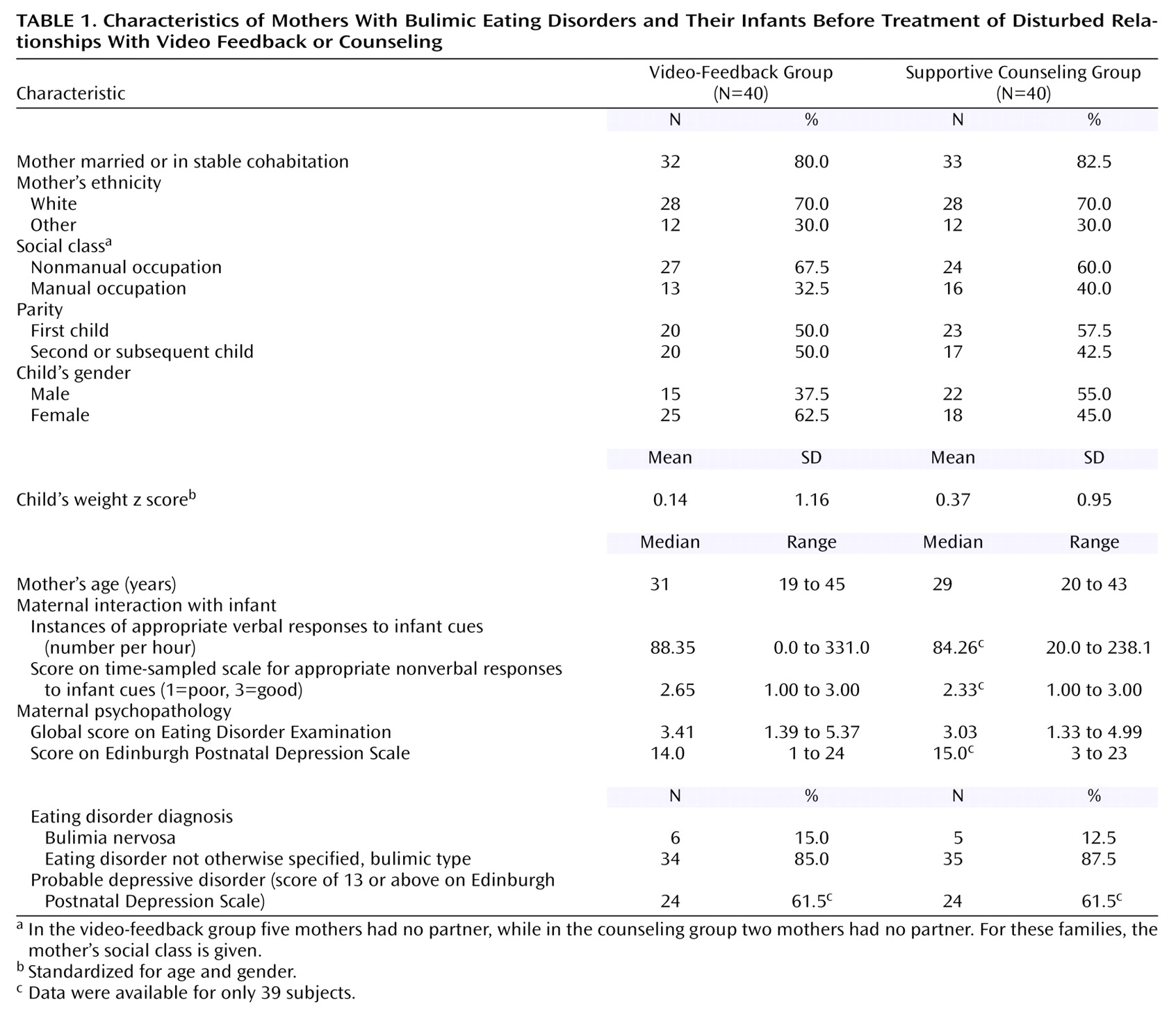
Baseline demographic characteristics and clinical presentation were well balanced across the treatment groups (
Table 1 ) except for indications of imbalances in infant gender and weight.
For all outcome data available, statistical comparisons were on an intention-to-treat basis, i.e., N=38 for the video-feedback group and N=39 for the counseling group. There were no differences between the two groups in the mean number of sessions completed: 12.1 (SD=1.9) for the video-feedback group and 11.1 (SD=3.5) for the counseling group.
Mother-Infant Interaction
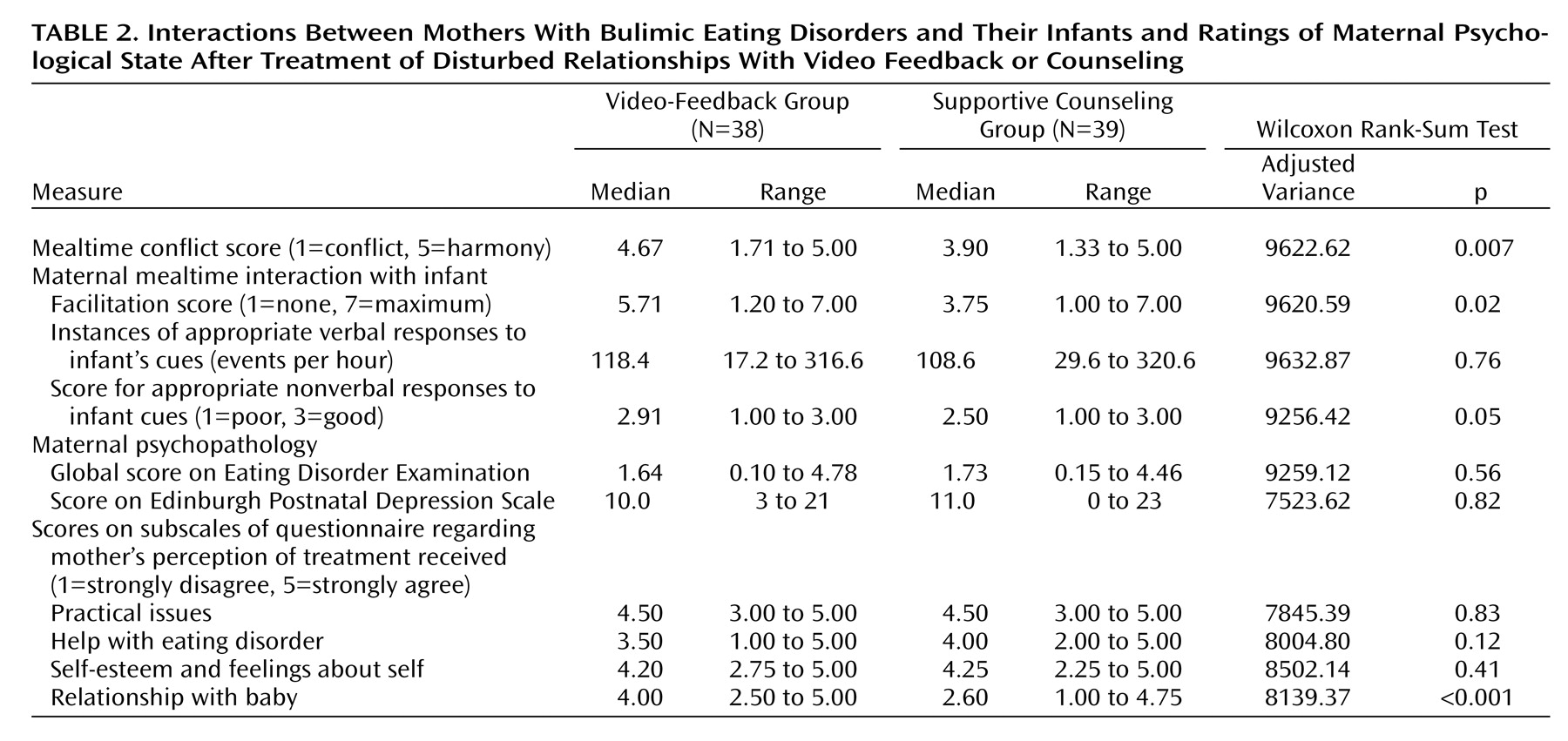
The group that received video feedback exhibited significantly less conflict than the group that received supportive counseling, according to scores on the conflict rating scale (
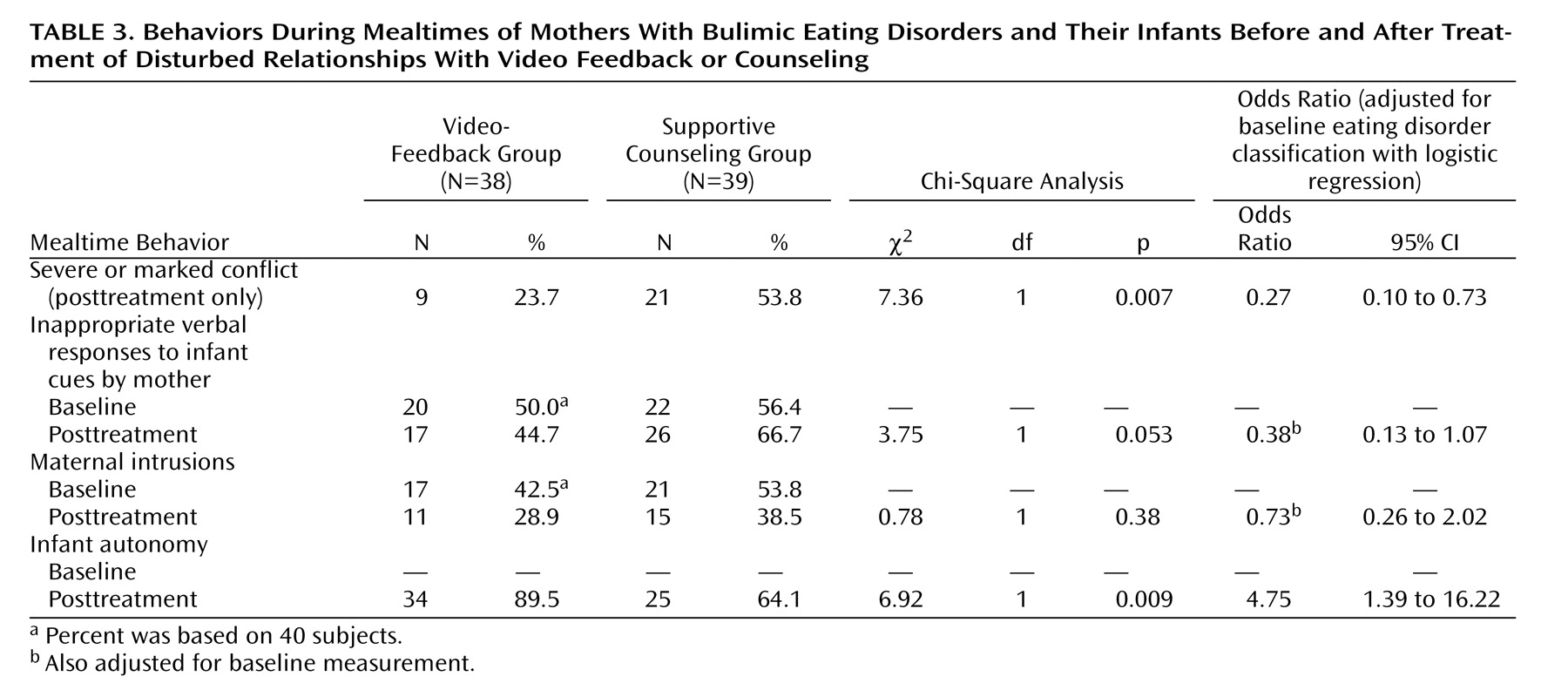
Table 2 ). Episodes of marked or severe conflict were observed for 23.7% of the mother-infant pairs in the video-feedback group and 53.8% of those in the control group (
Table 3 ). The odds ratio of 0.27 corresponds to an estimated 73% reduction in the odds of a marked or severe conflict episode (95% CI, 27% to 90%) in the video-feedback group when compared with the control group.
Further benefits of video feedback included the child’s significantly greater autonomy during mealtimes (
Table 3 ). There was also evidence of greater maternal facilitation of the infants and a higher level of appropriate nonverbal responses to infant cues in the video-feedback group (
Table 2 ). There was weaker evidence that the mothers receiving video feedback were less likely to use inappropriate verbal responses to infant cues than mothers in the control group (
Table 3 ), but there was no difference between the groups in appropriate verbal responses to cues (
Table 2 ). There was also no difference between the groups in terms of maternal intrusiveness, with reductions in both groups of around 30% (
Table 3 ).
Infant Weight
At follow-up, when the infants were 13 months old, the mean z scores (standardized) for infant weight were 0.11 (SD=1.10) for the video-feedback group and 0.23 (SD=0.93) for the counseling group. While we observed a slight imbalance at baseline favoring the counseling group (
Table 1 ), the mean adjusted difference in standardized infant weight at 13 months was 0.03 (95% CI, –0.38 to 0.32, p=0.85); i.e., there was no significant difference between the groups in (standardized) infant weight.
There was a nonsignificant positive correlation between poorer weight gain from pretreatment to age 13 months and the conflict rating at 13 months (r s =0.16, N=77, p=0.16).
Maternal Eating Disorder Psychopathology
There were no significant differences between the groups in maternal eating disorder psychopathology at follow-up (
Table 2 ), and both groups’ scores on the Eating Disorder Examination improved significantly over the course of the treatment; the mean change across the groups was 1.32 points (95% CI, 1.06 to 1.57). Eleven (29.7%) of 37 mothers in the video-feedback group and 12 (30.8%) of the 39 in the control group still fulfilled the diagnostic criteria for an eating disorder. There were no differences between the groups in depressive symptoms (
Table 2 ), but there were overall improvements in both groups; the mean change across groups in the score on the Edinburgh Postnatal Depression Scale was 2.71 (95% CI, 1.32 to 4.10).
Post hoc multiple regression analysis was used to examine the influences of change in eating disorder score, change in depressive symptoms, and the treatment group (video feedback versus supportive counseling) on conflict outcome. Only the treatment group variable was significant (multiple linear regression, t=–2.29, p=0.03).
Maternal Expectations and Perceptions of Treatment
There were no differences between the groups in their expectations of treatment; the median scores, on a scale of 1 (not at all helpful) to 5 (very helpful), were 4 for the video-feedback group (range=2–5) and 5 for the counseling group (range=3–5) (adjusted variance=7475.35, p=0.67). At the end of treatment, the women in the video-feedback group perceived themselves to be significantly more helped than the control group with their relationships with their infants (
Table 2 ), notably with “the way my baby and I get on at mealtimes,” but there were no differences between groups in scores on the other subscales. Both groups perceived themselves to be considerably helped with their eating disorder and with their own feelings and self-esteem.
Discussion
We found that a video-feedback treatment directed specifically at mother-infant interaction led to greater improvements in outcome than did a counseling treatment focused on the mother. In particular, the index treatment was associated with less conflict, better maternal facilitation and appropriate nonverbal responses to infant cues, fewer inappropriate verbal responses to cues by the mother, and greater child autonomy during mealtimes. To our knowledge, this is the first time that a treatment in the context of postnatal psychiatric disorder has been shown to lead to key improvements in mother-child interaction in a controlled trial.
The estimated 73% reduction in the odds of a marked or severe conflict episode in the video-feedback group, compared to the control group, is striking as even the lower limit of the 95% confidence interval, which corresponds to a 27% reduction, is likely to be clinically relevant. These findings are important because of the central role of mealtime interaction in the mother-infant relationship
(20), especially in the context of maternal eating disorder. Mother-infant conflict and the associated damping of infant initiatives and autonomy have the potential to make mealtimes an aversive experience for the infant with lasting negative associations around food. Such conflict is especially likely to occur between mothers with eating disorders and their infants, and it can be seen as an index of the extent to which the infant gets embroiled in the mother’s eating psychopathology. Hence, the amelioration of these parenting deficits has the potential to mitigate their impact on the infant and may play a role in halting the intergenerational transmission of this form of psychiatric disturbance.
Both groups maintained infant weight at the end of the study; the mean weight of infants in each group was a little over the population mean, and there were no differences between the groups. Thus, although video feedback did not lead to a significant between-group difference in infant weight, it is reassuring that there was no falloff in weight in either group. While a relationship between conflict and lower weight has previously been demonstrated
(5), in this study the association between poorer infant weight gain and conflict at age 13 months was small and nonsignificant. Many factors influence weight gain, and this requires further investigation.
There were also no significant differences between the treatment groups in maternal intrusions or appropriate verbal responses to cues. Both groups showed considerable improvement in maternal eating disorder psychopathology. There was also a high level of depressive symptoms at baseline, which also improved in both groups. The differences in conflict outcome were found to be due to the specific treatment each group received, rather than change in either eating disorder psychopathology or depression symptoms. Conflict was not related to infant weight at follow-up.
The strengths of this study were 1) two active treatments were compared, one targeted at mother-child interaction and the other targeted at the mother, 2) in contrast to many psychological treatment studies, the principal outcomes were assessed by using videotape, ensuring that the raters remained blind to group status, and 3) treatment was carried out in the mothers’ homes, which provided ecological validity and contributed to the low dropout rate. The weaknesses of this study were 1) the relatively small number of subjects, necessitating a larger study, and 2) mothers in both groups received guided self-help for their eating disorder, since it is ethically problematic to leave an identified disorder untreated. We were therefore unable to ascertain how necessary guided self-help was in supporting video feedback in reducing conflict.
To our knowledge, this is the first treatment trial to target mother-infant interaction in the context of maternal eating disorders. Related studies have attempted to treat mothers with postnatal depression and their infants and have indicated that, while it is possible to improve maternal psychological state, it is more difficult to improve significantly the mother-child interaction and child outcome
(8) . While these studies used treatments to help with mother-child interaction, they did not use video feedback, which provides direct access to mother-child interaction. This study has shown that by providing such access to mother-child interaction, this interaction can be improved.
One of the reasons that video feedback is particularly suited to eating disorders, and possibly to postnatal depression, is that these disorders are characterized by a narrowed focus of attention to issues germane to the disorder (body shape, weight, and eating in the case of eating disorders). This in turn is likely to impair the mother’s responsiveness to the environment, particularly her infant’s communication. Video-feedback treatment focuses the mother away from her eating preoccupations onto the infant. It helps her to notice and interpret her infant’s behavior and highlights where she can encourage her infant. Further follow-up is necessary to ascertain whether these improvements are maintained and the children’s longer-term outcome improved.
In terms of generalizability, it should be noted that relatively broad inclusion criteria were used and most subjects were diagnosed with eating disorder not otherwise specified. Strict impairment criteria ensured that only women with clinically significant levels of disorder were included, and the baseline scores on the Eating Disorder Examination were comparable to those of patients included in treatment trials for bulimia nervosa
(12) . It should be noted that although guided self-help is a relatively limited treatment, there was considerable improvement in eating disorder psychopathology as well as in depressive symptoms.
In conclusion, psychiatric disorders, including eating disorders, occur commonly among women of childbearing age and raise the risk of adverse effects on mother-child interaction and child development. This study indicates that a targeted treatment conducted in the community in the postnatal period can have significant benefits for mothers with eating disorders and their infants. The low dropout rate indicates that the treatment is both feasible and acceptable to parents. If these findings are replicated, video feedback holds promise as a treatment for a range of postnatal psychiatric disorders.