Body dysmorphic disorder (BDD), a distressing or impairing preoccupation with an imagined or slight defect in one’s physical appearance, is relatively common and associated with markedly poor functioning and quality of life
(1 –
5) . Seventy percent of individuals with BDD report a history of suicidal ideation attributed primarily to BDD, and 22%–24% have attempted suicide
(6,
7) . Despite evidence that BDD is a severe disorder, research is still limited. In particular, little is known about BDD’s course, and, to our knowledge, no prospective follow-up studies of its course have been performed. The course of illness is a fundamental aspect of psychopathology that has important implications for clinical practice
(8) .
One cross-sectional study (N=188)
(7) retrospectively assessed the past course of BDD symptoms over the subjects’ lifetime. This study found that BDD had a chronic course (i.e., less than 1 month of remission since illness onset) in a majority of cases (82%). The mean duration of BDD was 15.7 years (SD=11.9, range=1–69). However, all data about the course of the disorder were obtained retrospectively and were limited, and standard measures were not used to assess illness course.
To our knowledge, the only other study that has assessed the course of BDD is a chart review study
(9), which suggested that BDD may be less chronic than indicated by the cross-sectional study. This study contained 95 patients treated in a BDD specialty practice over 1.7 years (SD=1.1, range=0.5–6.4). Medical records were reviewed at 6-month intervals, with psychiatric status ratings from the reliable and valid Longitudinal Interval Follow-Up Evaluation
(10,
11) . When the authors allowed for censoring, lifetable analysis estimated that at 6 months and/or 12 months, 25% of the patients had achieved full remission from BDD and 58% had achieved partial or full remission. After 4 years of follow-up, 58% had achieved full remission and 84% had achieved partial or full remission at one or more 6-month assessment points. Of the subjects attaining partial or full remission, 29% subsequently relapsed. However, this study used retrospective chart review methods and assessed clinical status only every 6 months. In addition, all patients were treated in a BDD specialty program, potentially limiting the generalizability of the findings.
In the present study, which is, to our knowledge, the first prospective follow-up study of BDD’s course, we examined this disorder’s course over 1 year. Weekly BDD symptom status ratings with reliable measures were obtained for subjects recruited from a wide variety of sources . We hypothesized that BDD would usually be chronic, with BDD symptoms occurring more frequently than remission.
Method
Subjects
Two hundred subjects were enrolled in this ongoing single-site longitudinal study of the course of DSM-IV BDD. All subjects met the full criteria for lifetime (i.e., current or past) DSM-IV BDD or its delusional variant (delusional disorder, somatic type). Subjects with the delusional variant of BDD met full DSM-IV criteria for BDD; in addition, their beliefs about their perceived appearance flaws were of delusional intensity (as opposed to being nondelusional), as determined by the reliable and valid Brown Assessment of Beliefs Scale
(12) . DSM-IV allows BDD’s delusional and nondelusional variants to be double coded (i.e., individuals with delusional BDD may receive diagnoses of both BDD and delusional disorder), reflecting the likelihood that they are the same disorder. Indeed, previous studies have found that individuals with these variants of BDD have far more similarities than differences
(13) . Additional inclusion criteria were being age 12 or older and an ability to be interviewed in person. To maximize the generalizability of the study findings, the only exclusion criterion was the presence of a mental disorder (e.g., dementia) that would interfere with the collection of valid interview data. Subjects were obtained from a variety of sources: mental health professionals (46.0%), advertisements (38.6%), our program’s web site and brochures (10.2%), the subjects’ friends and relatives (3.4%), and nonpsychiatrist physicians (1.7%). This report presents data for the 183 subjects (91.5% of the intake group) for whom 12-month interview data were available. A subset of 161 subjects who met full DSM-IV criteria for BDD during the week before the intake interview and had 12-month interview data are included in analyses examining remission from BDD. The additional 22 subjects, who are included in analyses of relapse, had met full DSM-IV criteria for BDD in the past but were in partial (N=15) or full (N=7) remission from BDD at the time of the intake interview. The study was approved by Butler Hospital’s Institutional Review Board. After a complete description of the study to the subjects, written informed consent was obtained (assent plus parental consent for adolescents).
Assessments
The 200 subjects were comprehensively evaluated at intake with self-reports and interviewer-administered measures described in more detail elsewhere
(14) . Intake measures relevant to this report included the Structured Clinical Interview for DSM-IV Axis I Disorders—Non-Patient Edition
(15), which was used to disgnose BDD and comorbid axis I disorders. The BDD Form, a semistructured instrument (available from the first author) and used in previous BDD studies (e.g., references
1,
7), obtained data on demographic characteristics, cross-sectional/retrospective data on BDD’s clinical features (e.g., age at BDD onset and past course of BDD), and information on past and current treatment. Current BDD severity was assessed with the Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder
(16), a reliable and valid 12-item semistructured measure (scores range from 0 to 48). The Global Assessment of Functioning (GAF) Scale
(15) assessed global symptoms and functioning (scores range from 0–100, with lower scores indicating poorer functioning).
This article focuses on the first year of follow-up data from this ongoing longitudinal study. Follow-up interviews were conducted at 1 year for 183 subjects (91.5%) with the Longitudinal Interval Follow-Up Evaluation. This evaluation is a semistructured interview and rating system for assessing the longitudinal course of mental disorders
(10,
11) . It is based on an approach originally used in the National Institute of Mental Health Collaborative Depression Study
(17) and has been used in many other longitudinal studies to track the course of illness based on DSM criteria (e.g., references
11,
17) . The Longitudinal Interval Follow-Up Evaluation gathers information on symptom severity, diagnostic status, psychiatric treatment received, and classes of medication and doses. It tracks the course of illness with psychiatric status ratings, which are disorder specific and global 3- to 7-point ratings of disorder severity that have cutoff points for full DSM-IV criteria, partial remission, and full remission. Psychiatric status ratings have been shown to have good interrater reliability, test-retest reliability, and convergent validity
(11) . Individual psychiatric status ratings are assigned for each week of follow-up, providing summaries of course and allowing calculation of time to remission and relapse.
BDD psychiatric status ratings are the following:
Some concern about appearance but no distress or impairment in functioning due to BDD
Some concern about appearance, with either mild distress or mildly impaired functioning
Some concern about appearance, with both mild distress and mild impairment in functioning
Some concern about appearance present for at least 1 hour per day and either moderate distress or moderate functional impairment
Preoccupation about appearance causes significant distress and significant functional impairment
Concern about appearance causes severe or extreme distress and functional impairment
For example, thinking about one’s appearance “defects” for 2–3 hours a day accompanied by moderate distress, poor concentration at work, and missing 25% of social events because of BDD would receive a BDD psychiatric status rating of 5. Thinking about one’s appearance for 10–12 hours a day, extreme distress, and being housebound and unable to work because of BDD would receive a BDD psychiatric status rating of 7. A priori definitions pertaining to BDD’s course were defined as in studies of other disorders, courses: “continuous BDD symptoms” means meeting full DSM-IV criteria for BDD (psychiatric status ratings of 5–7) over the entire follow-up period; “partial remission” means meeting less than full criteria (a psychiatric status rating of 3 or 4) for at least 8 consecutive weeks; and “full remission” means minimal or no BDD symptoms (psychiatric status rating of 1 or 2) for at least 8 consecutive weeks. Relapse was defined as meeting full BDD criteria for at least 2 consecutive weeks after being in full or partial remission for at least 8 consecutive weeks.
Because this was an observational study, treatment was not controlled. With the Longitudinal Interval Follow-Up Evaluation, we examined whether subjects received mental health treatment (psychotropic medication or psychotherapy) over the 1-year period. We also examined types of pharmacotherapy that were received. Because serotonin reuptake inhibitors (SRIs) are currently considered the first-line pharmacotherapy for BDD
(18,
19), including delusional BDD, we classified SRI trials according to whether they were “minimally adequate” or “optimally adequate” based on previously suggested dosing and duration guidelines
(19,
20) . The reliable Psychosocial Treatments Inventory
(21) was administered to determine the subjects’ perceptions of the type of therapy modalities (e.g., behavior) received. The subjects were considered to have received a particular modality if they reported receiving at least two techniques characteristic of that modality for at least four sessions.
The majority of the interviews were conducted in person by experienced clinical interviewers who were closely supervised by the first author. Interviewers received careful and rigorous training, as in similar longitudinal studies (e.g., reference 22). This training included discussing videotapes, conducting mock interviews with experienced interviewers, and being closely supervised during training sessions and initial interviews. All interviews are thoroughly edited, both clinically and clerically, by senior staff. Shrout-Fleiss interrater reliabilities for the maximum and minimum BDD psychiatric status ratings during the first 8 weeks and the last 8 weeks of a year for each subject were calculated, as in previous studies
(11) . Eight-week spans were used because this time period corresponds to our definition of remission. Reliabilities ranged from 0.91 to 1.00, with a mean reliability of 0.96. The test-retest reliability for the BDD psychiatric status ratings over 1 year yielded a correlation for maximum BDD psychiatric status ratings of 0.79 (p<0.0001) and a correlation for minimum BDD psychiatric status ratings of 0.78 (p<0.0001).
Data Analysis
SAS version 8.0 (SAS Institute, Cary, N.C.) was used for data analysis. Between-group differences at intake were examined with the chi-square test or Fisher’s exact test for dichotomous variables and t tests for continuous variables. Effect size estimates for chi-square analyses or Fisher’s exact test were determined with the phi coefficient (Cramer’s Variance (V): V=0.1 is a small effect size, 0.3 is a medium effect size, and 0.5 is a large effect size). Longitudinal analyses used standard survival analysis methods. Kaplan-Meier life tables were constructed for time to remission and relapse. Cox proportional hazards regression
(23) was used to estimate relative hazards for predictor variables. Statistical tests were two-tailed; the alpha level was 0.05.
Results
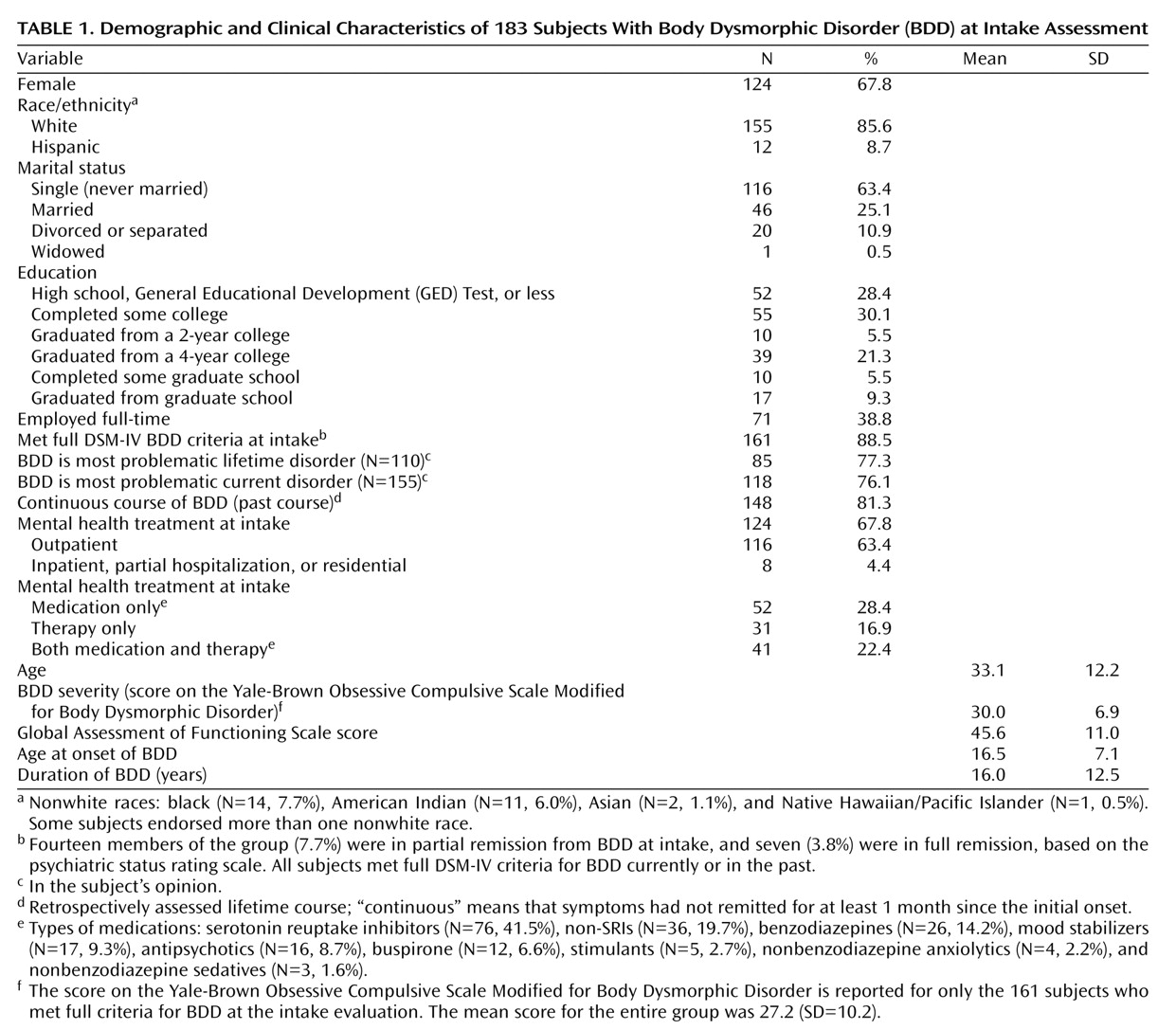
Table 1 presents demographic and clinical characteristics for the total group of 183 subjects at the intake assessment. Approximately two-thirds were female, a majority was single, mean BDD severity was in the moderate to severe range, and the mean GAF score reflected serious symptoms or serious impairment in functioning. The mean duration of BDD was 16.0 years, and 148 subjects retrospectively reported a continuous lifetime course of BDD. The 183 subjects with a 1-year evaluation did not significantly differ from the 17 subjects who had an intake evaluation but not a 1-year follow-up evaluation in terms of any characteristics shown in
Table 1, except that a higher proportion of those with follow-up data were receiving medication only at the time of the intake assessment (N=52 versus N=1, p<0.05, V=0.14).
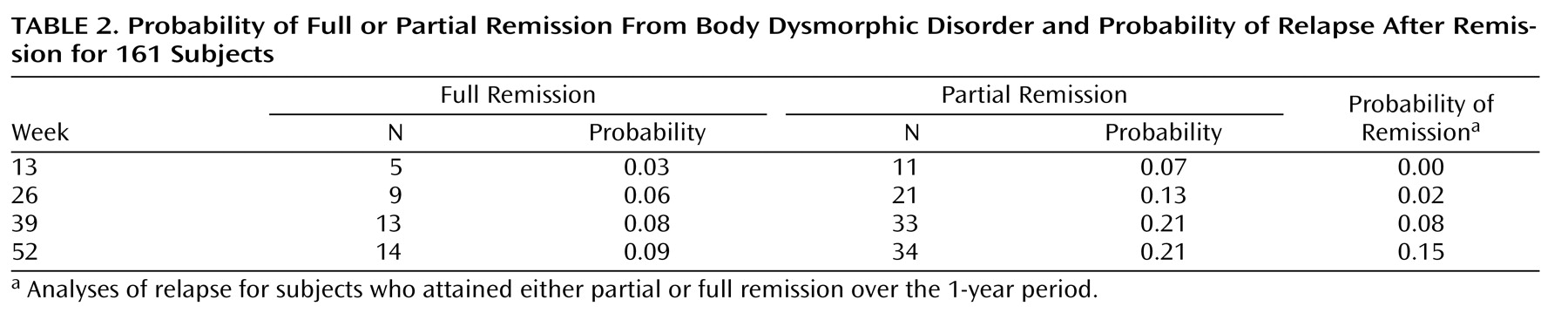
Table 2 shows remission and relapse probabilities at various points in time over the 12 months of follow-up for the 161 subjects who met full BDD criteria at intake. During the first 6 months, the probability of full remission was only 0.06 and the probability of partial remission was 0.13. After 1 year, the cumulative probability of full remission was only 0.09 and the cumulative probability of partial remission was 0.21. The mean BDD Psychiatric Status Rating over 1 year was 5.1 (SD=1.1), which reflects full BDD criteria. The mean proportion of time that the subjects met full BDD criteria during the 1-year period was 80.4% (SD=32.0). The probability of full or partial remission from BDD over 1 year was not significantly predicted by gender or race/ethnicity.
Relapse probabilities for the 48 subjects who met full criteria for BDD at intake and then fully or partially remitted from BDD (and were therefore eligible for relapse) are shown in the last column of
Table 2 . When we examined relapse, we combined subjects experiencing either full or partial remission over 1 year because so few subjects fully remitted and were therefore eligible for relapse. The probability of relapse over 6 months was 0.02, and over 1 year, it was 0.15. Additionally, we combined these 48 subjects with the 22 subjects who were already in partial or full remission at intake (and for at least 8 subsequent consecutive weeks) and were also eligible for relapse. The cumulative probability of relapse for the combined group (N=70) was similar to that for the subset of 48 subjects who met full BDD criteria at intake: 0.00 after 3 months, 0.03 after 6 months, 0.07 after 9 months, and 0.12 after 1 year.
A total of 154 subjects (84.2%) reported receiving mental health treatment during the 1 year of follow-up; 87 (47.5%) reported receiving mental health treatment focused specifically on their BDD symptoms. A total of 142 subjects (77.6%) reported receiving psychotropic medication, most commonly SRIs (N=107, 58.5%), followed by non-SRI antidepressants (N=50, 27.3%) and benzodiazepines (N=41, 22.4%). A total of 30 subjects (16.4%) received at least one SRI trial considered optimally adequate for BDD, and an additional 21 (11.5%) received a minimally adequate SRI trial. Of the 161 subjects who met full BDD criteria at intake, those who received an SRI during the 1-year follow-up period were not more likely to remit from BDD than those who did not receive an SRI (hazard ratio=0.999, p=0.56). Subjects who received at least a minimally adequate SRI trial during the follow-up period were nonsignificantly less likely to remit from BDD than those who did not (hazard ratio=0.728, p=0.44).
A total of 108 subjects (59.0%) reported receiving psychotherapy. Eighty (43.7%) reported receiving supportive or psychodynamic techniques, and 41 (22.4%) received behavior techniques. Fifty-one (27.9%) received cognitive techniques focusing specifically on BDD, and 43 (23.5%) received behavior techniques focusing specifically on BDD; of these subjects, 40 (21.9%) received both cognitive and behavior techniques focusing on BDD. The subjects who received cognitive or behavior techniques focusing on BDD were nonsignificantly less likely to remit from BDD during the follow-up period (hazard ratio=0.598, p=0.14).
Discussion
This study found that BDD is usually chronic, as hypothesized. Only 9% of the subjects experienced full remission, and only 21% experienced partial remission from BDD over 1 year of follow-up. The mean proportion of time that the subjects met full BDD criteria during the 1-year period was 80%. This was the case even though a majority of the subjects received mental health treatment during the follow-up period.
The remission probabilities found in this study are lower than those for most other disorders in studies of illness course with nearly identical methods to ours (e.g., the same measures and definitions of remission and a similar proportion of the subjects receiving treatment). In contrast to our 1-year full remission probability of 0.09, 1-year full remission probabilities for mood disorders have ranged from 0.63 (for mixed bipolar disorder) to 0.90 (for mania)
(24,
25) . For anxiety disorders, full remission probabilities after 1 year in studies similar to ours were 0.40 for panic disorder, 0.17 for panic disorder with agoraphobia, and 0.16 for generalized anxiety disorder
(26) . Social phobia is one disorder that appears as chronic as BDD (with a full remission probability of 0.07)
(26) . BDD appears even more chronic than axis II disorders, for which 1-year full remission probabilities have ranged from 0.19 (for schizotypal personality disorder) to 0.38 (for obsessive-compulsive personality disorder)
(27) . BDD’s chronicity is particularly problematic because individuals with BDD have unusually poor functioning and quality of life, with more severe BDD symptoms significantly associated with poorer functioning and quality of life
(5) .
The present study’s findings that after 1 year only 9% of the subjects had fully remitted from BDD and only 21% had partially remitted differ considerably from the only previous study of BDD’s course, which found that by 1 year, 25% of the patients had fully remitted from BDD and 33% had partially remitted
(9) . A possible explanation for these different findings is that all subjects in the previous study were treated in a BDD specialty program and received treatment that was specifically focused on the symptoms of BDD, in contrast to the present study. In the present study, only 47.5% of the subjects reported receiving mental health treatment focused on their BDD symptoms, and only 16.4% reported receiving an “optimally adequate” SRI trial. This may be a reason, at least in part, for the present study’s far lower remission rates than in the previous retrospective chart review study
(9) or in pharmacotherapy efficacy trials over several months
(19,
28,
29) . However, it must be emphasized that a causal relationship between treatment received and course of illness cannot be established in an observational study such as this. Factors other than treatment may have contributed to the low remission rates observed in this study. For example, the subjects may have been more severely ill than the subjects in treatment efficacy trials, which have strict inclusion and exclusion criteria and thus may exclude more severely ill patients (e.g., those with a current substance use disorder or clinically significant suicidality).
In the present study, 15% of the remitting subjects subsequently relapsed. However, the probability of relapse at 1 year is not well estimated because few subjects remitted early and were followed for relapse for the remainder of the year. For example, the subjects who partially or fully remitted from BDD at 6 months were eligible for relapse for only the remaining 6 months. Thus, it will be important to examine relapse rates in studies with longer follow-up periods.
This study has a number of limitations. Because a majority of the subjects received mental health treatment during the follow-up period, it is unclear how generalizable the results are to untreated individuals in the community. In addition, data on treatment received or the extent to which treatment actually focused on BDD were not confirmed by medical records review; also, we did not gather data on the receipt of cognitive therapy that was not focused on BDD. Furthermore, course data were obtained for only 1 year, and studies over longer follow-up periods are needed, especially to determine relapse probabilities. Such studies will also increase the power to examine the relationship of treatment to illness course and take into account characteristics associated with receiving treatment and even more intensive treatment. The present study is ongoing and will extend the results reported here. Because so few subjects experience full remission of their illness, relapse probabilities were not calculated separately for full remitters and partial remitters. An important question for future studies is whether relapse probabilities differ in these two groups. The strengths of this study include a broader study group than in most previous BDD studies (inclusion/exclusion criteria were broad; one-third of the subjects were not receiving mental health treatment at intake, and most subjects were not treated in a BDD specialty setting). In addition, the subjects received careful diagnostic and weekly symptom evaluations with measures with strong psychometric properties.