Childhood-onset neuropsychiatric disorders—which include attention deficit hyperactivity disorder (ADHD), autism spectrum disorders, tic disorders, and learning disabilities—are defined by operational criteria targeting behaviors and deficits in abilities such as attention, empathy, communication, flexibility, and IQ
(1) . Research during the 1990s showed that these disorders are more frequent than previously assumed
(2 –
5), with severe variants affecting at least 5% of all children and milder phenotypal expressions or “shadow syndromes” frequent in relatives of affected children
(6 –
11) . Hypothetically, neuropsychiatric diagnoses designate dysfunctional extremes of normally distributed abilities, such as attention and impulse control; adaptive decision-making strategies; adequate perception and control of voice, posture, mimicry, and interpersonal skills; and mentalizing. The variation in such abilities is partly constitutional and may influence personality development to a greater extent than recognized in current personality theory. Patients afflicted by such dysfunctions describe themselves in terms applicable to personality disorders
(12,
13) . Subjects with personality disorders demonstrate neurocognitive problems
(14 –
16), and personality disorders are common in follow-up studies of subjects with neuropsychiatric disorders
(17,
18) . These observations suggest that deficits in neurocognitive development during childhood may often lead to personality disorders during adulthood. In other words, certain childhood temperament profiles may impair healthy character development, producing personality disorders in adulthood.
In the DSM system, personality disorders are assessed on a separate axis from the “major mental disorders” and, analogous with the ICD system, are defined categorically. Both principles are controversial and disputed by most experts, since empirical data lend no support for a sharp delineation of personality disorders from other mental disorders or for a categorical structure for personality traits
(19) . Although the validity of DSM-IV personality disorders seems weak, reliability in assessments by means of structured interviews such as the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) has been demonstrated
(20) .
Cloninger’s biopsychosocial theory of personality
(21) is based on the assumption that personality involves four temperament dimensions and three character dimensions. The four dimensions of temperament measure individual differences in basic emotional drives: harm avoidance (i.e., pessimistic and anxious versus optimistic and risk-taking); novelty seeking (i.e., impulsive and irritable versus rigid and stoical); reward dependence (i.e., sociable and warm versus aloof and cold); and persistence (i.e., persevering and ambitious versus easily discouraged and lazy). The three character dimensions measure individual differences in higher cognitive processes that define a person’s style of mental self-government: self-directedness (i.e., responsible and resourceful versus blaming and inept), cooperativeness (i.e., helpful and principled versus hostile and opportunistic), and self-transcendence (i.e., intuitive and insightful versus concrete and conventional). This model can serve as a tool for disentangling personality problems or disorders in subjects with neuropsychiatric disorders
(12) . A 238-item self-rating instrument, the Temperament and Character Inventory
(21) has been developed to measure the model’s seven personality dimensions. Presence of a personality disorder is indicated by presence of character immaturity (especially by low self-directedness and/or cooperativeness) and type of disorder by the temperament configuration
(22,
23) . The least frequent answers from each Temperament and Character Inventory dimension form a rarity scale, generally used for validation purposes. In this study, rarity is also used as a reflection of mental health problems and distorted ideas, since rarity scores have been shown to differ considerably between subjects in the general population (who generally have very low rarity scores) and subjects with mental disorders (who have much higher scores)
(24) .
This article presents patterns of self-rated personality traits measured by the Temperament and Character Inventory and current personality disorder symptoms measured according to DSM-IV in a relatively large group of adult neuropsychiatric outpatients with ADHD or autism spectrum disorders. We previously observed deficits in maturation of character in adult subjects with Asperger syndrome
(12), and we hypothesized that ADHD and autism spectrum disorders would be associated with 1) specific temperament profiles (particularly high novelty seeking in those with ADHD and low reward dependence in those with autism spectrum disorders), 2) deficits in character maturation (particularly low self-directedness and low cooperativeness), and 3) personality disorders as defined in DSM-IV.
Method
The Göteborg Child Neuropsychiatric Clinic is the only diagnostic center specifically focused on neuropsychiatric assessments of childhood-onset disorders in the city of Göteborg and has a nationwide responsibility for assessment of autism and related disorders. Between January 2001 and April 2003, an “Adults Project” was carried out at the clinic, offering specialized assessments of adult patients with possible childhood-onset neuropsychiatric disorders (ADHD, autism spectrum disorders, tic disorders, and various kinds of learning disorders). Many of these patients were self-referred or came from general practitioners, but 59% were secondary or tertiary referrals from specialists in adult psychiatry dealing with “hard-to-diagnose” in- and outpatients attending psychiatric clinics. Only a minority of the patients had been diagnosed in childhood. Thus, in most cases childhood developmental problems were assessed retrospectively. All assessments for the project were on an outpatient basis. Subjects provided clinical data and blood for genetic analyses within the Göteborg Neuro-Psychiatry Genetics Project, which aimed to establish large, well-characterized, clinical cohorts for genetic studies. The present study group consists of all subjects who gave informed consent to participate in the Neuro-Psychiatry Genetics Project (N=273) and completed the Temperament and Character Inventory within the stipulated time frame (N=240; 131 men, 109 women; median age=31.0 years, range=19–60).
DSM-IV diagnoses (including ADHD and autism spectrum disorders) were assigned in each case by two authors (H.A., M.R.) after consensus discussions. The individual diagnoses were based on all available information including clinical status of the patient, the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID), the Yale-Brown Obsessive Compulsive Scale, the Asperger Syndrome and High-Functioning Autism Screening Questionnaire
(25), the Asperger Syndrome Diagnostic Interview
(26), and DSM-IV criteria checklists, current and lifetime, for autism spectrum disorders, ADHD, tic disorders, impulse control disorders, and all other relevant axis I disorders not covered by the SCID. Reliability and validity for all these scales are good to excellent. In 209 of the 240 cases (87%), a semistructured collateral interview was performed with a relative who had known the index subject as a child. Clinical records were collected from pediatric and child psychiatry services and from school health services. For all disorders, DSM criteria that limited the possibility of assigning other comorbid psychiatric diagnoses were disregarded to allow a comprehensive recording of the pattern of comorbidity.
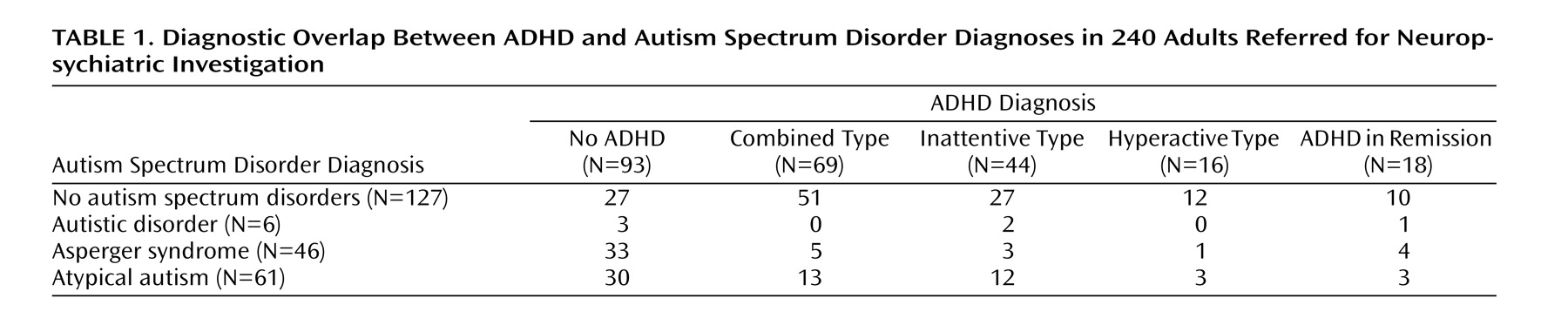
One hundred thirteen subjects had an autism spectrum disorder (autistic disorder [N=6], Asperger syndrome [N=46], or atypical autism [N=61]), while 147 had ADHD (combined type [N=69], inattentive type [N=44], hyperactive type [N=16], or ADHD in remission [N=18]). The diagnostic overlap between autism spectrum disorders and ADHD is shown in
Table 1 . Twenty-seven subjects (14 men, 13 women; median age=39.0 years, range=20–59) had neither a diagnosis of ADHD nor an autism spectrum disorder but other diagnoses (specific learning disorders/dyslexia [N=7], tic disorders [N=3], eating disorders [N=2]) and often subsyndromal ADHD or autistic traits. A subset of 159 (66%) of the 240 subjects (85 men, 74 women; median age=33.0 years, range=19–60) plus 15 subjects (10 men and five women; median age=32.0 years, range=19–46) who did not complete the Temperament and Character Inventory were assessed with the SCID-II. These interviews were performed by independent clinical psychologists with special expertise in test assessment and structured interviews.
Ethics
The Neuro-Psychiatry Genetics Project was approved by the ethics committee of Göteborg University. After complete description of the study to the subjects, written informed consent was obtained.
Statistical Method
Self-rating scales were administered in a standardized manner, and the Temperament and Character Inventory was scored comparing the raw scores for each dimension to sex- and age-matched norm groups to yield T scores with a defined mean of 50 (SD=10) using Swedish norms for the Temperament and Character Inventory. The T scores were compared to the expected mean of 50 in the general population by one-sample t tests. All statistics were calculated with the SPSS 11.0 software, using two-tailed p values.
Results
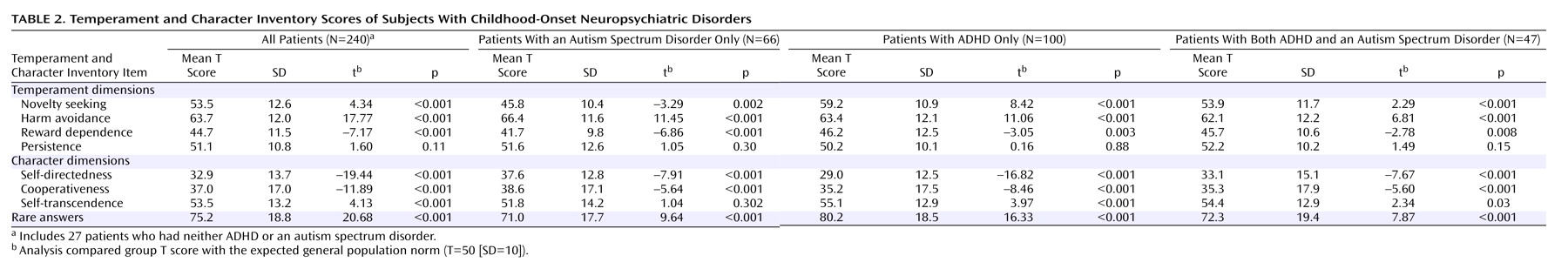
Self-rated personality traits in the cohort differed dramatically from those reported by subjects in the general population. The whole patient group had significantly higher scores for novelty seeking and harm avoidance and significantly lower scores for reward dependence (
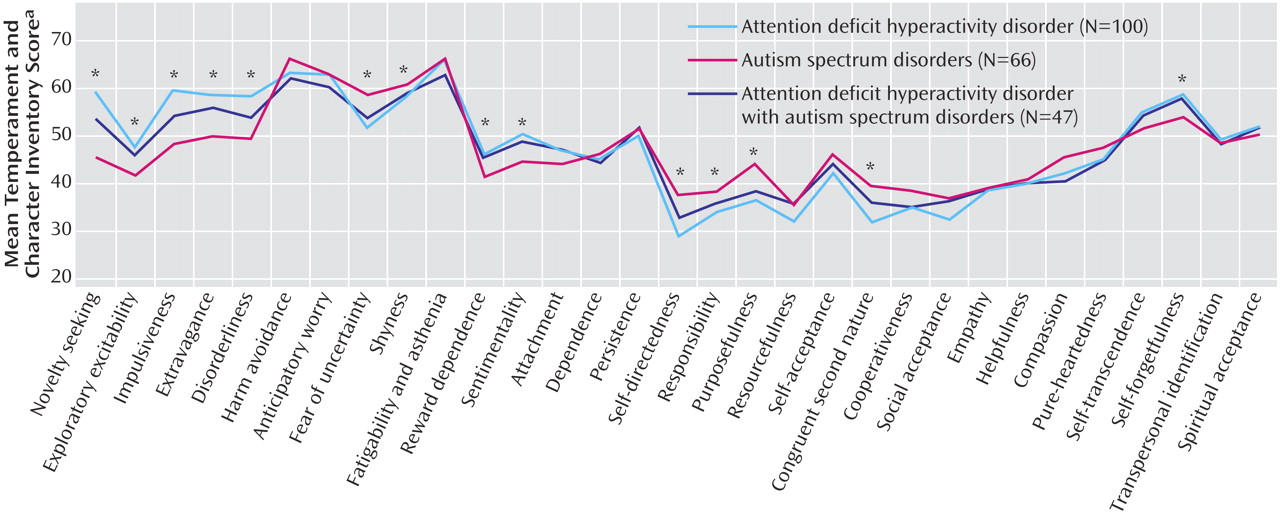
Table 2 ). Mean T scores for subjects with autism spectrum disorders only, ADHD only, and those with both disorders are illustrated for all Temperament and Character Inventory subscales in
Figure 1 .
Extremely low scores for self-directedness and cooperativeness were recorded, strongly indicating a high rate of clinically significant personality disorders
(24) . Only 35 subjects (15%) had a total raw score of 62 or more on these dimensions, i.e., the cutoff for “character maturity.” Subjects diagnosed with ADHD had even lower character scores than subjects with autism spectrum disorders. High harm avoidance scores, especially fatigability/asthenia and anticipatory worry, were also a prevalent finding in both groups. The different diagnostic groups had distinctive temperamental profiles: ADHD was mainly associated with high novelty seeking, while autism spectrum disorders were associated with low novelty seeking and low reward dependence, especially sentimentality and attachment. Patients who had both autism spectrum disorders and ADHD had more ADHD-like temperament and lower character scores than subjects with autism spectrum disorders only.
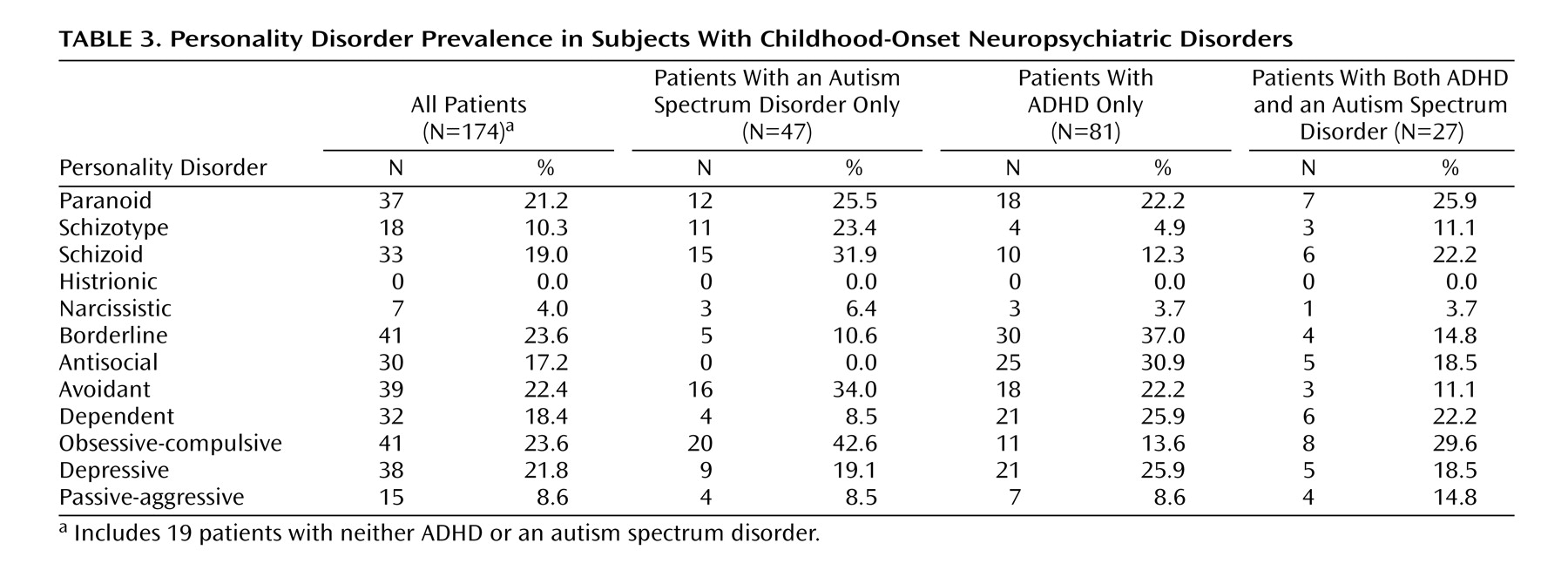
Subjects with both ADHD and autism spectrum disorders had high rates of categorical DSM-IV personality disorders, especially borderline personality disorder in ADHD patients and obsessive-compulsive personality disorder in autism spectrum disorder patients (
Table 3 ). A total of 130 (75%) of the 174 subjects for whom the SCID-II was completed met criteria for at least one personality disorder, and 80 fulfilled criteria for more than one category of personality disorder.
Discussion
In this group of adult patients with childhood-onset neuropsychiatric disorders, a personality disorder profile was described both according to self-ratings and clinical interviews in the vast majority of cases. The initial assumption that childhood-onset neuropsychiatric disorders would be reflected as “difficult temperaments,” deficits in character maturation, and personality disorders was confirmed. This is an important finding given that, depending on the theoretical framework and training of the psychiatrist, a patient with a childhood-onset neuropsychiatric disorder, particularly if previously undiagnosed, might well be diagnosed as having a “primary” personality disorder when assessed in adult age. Such a diagnosis is clearly “correct” according to the diagnostic manuals, but whether or not it contributes to furthering the understanding of the particular problems faced by the individual suffering from childhood-onset autism spectrum disorders or ADHD is arguable, with opinions differing according to whether one’s perspective focuses on childhood, adulthood, or covers the entire lifespan. The use of DSM-IV personality disorder criteria is difficult in such complex patients because of the frequent overlap between DSM-IV categories and the difficulty of making etiological judgments (e.g., “not better accounted for by ….”).
In Cloninger’s model, the childhood-onset neuropsychiatric disorders are associated with a severely compromised character maturation (i.e., personality disorder), with a “typical ADHD temperament” corresponding to the explosive/borderline type with high novelty seeking and harm avoidance in combination with low reward dependence, or a “typical autism temperament” with high harm avoidance and low reward dependence (but novelty seeking in the low to normal range), i.e., a methodical/obsessive temperament. Given that subjects with ADHD had lower character scores than those with autism spectrum disorders without ADHD, the neuropsychiatric disabilities associated with ADHD may constitute particularly important obstacles in character development. Attention problems leading to fragmented perceptions of the environment, together with deviant social perceptions, may lead to substantial neurocognitive problems that have been described as poor central coherence and disturbed mentalizing (i.e., self-monitoring) processes. Considering the high rate of clear-cut neuropsychiatric disorders in childhood, and considering the evidence for “broader phenotypes” or “shadow syndromes” of these disorders, a reasonable hypothesis would be that neurocognitive skills including attention, impulse control, empathy, and communication are of general importance in the development of “personality.” The development of mentalizing may depend on primary perceptual and communicative functions
(27,
28) and interact with self-containment and the development of executive functions to create meta-representational thinking about self and others
(29) . Meta-representation probably forms the core of mindfulness and self-awareness, which is the hallmark of mature personality and well-being
(30) .
The division of psychiatry into child and adolescent versus adult (with a demarcation line at age 18 years) has created a significant obstacle to a developmental understanding of personality in relation to biological and psychiatric factors. The diagnostic definitions for various disorders mainly diagnosed in different age spans overlap considerably. Empirical data on large cohorts of subjects show that patients may meet diagnostic criteria for different types of disorders at different ages. Adult psychiatrists need to be better informed about the childhood “origins” of adult personality disorders, and child psychiatrists need to be aware that their young dysfunctional patients may become adult psychiatric patients, albeit under different labels. It may also be useful to consider character development in the treatment of adolescents and adults with neuropsychiatric disorders in order to prevent the development of maladaptive attitudes and personality problems and to enhance mindfulness, as in dialectical behavioral therapy in borderline personality disorder patients
(31) .
Research on personality and personality disorders has to face a number of conceptual and theoretical problems. A study may focus either on clearly disordered subjects (the neo-Kraepelin approach) or on traits that vary across normal personality (the neo-Schneiderian approach). Diagnostic criteria (problem definitions) may alternatively describe features/properties, interpersonal or cognitive attitudes, and functions in various everyday-life settings and adaptive/reactive patterns
(19) . Further problems are inherent in the separation between major mental disorders (“diseases”) and personality disorders and in the need for a developmental perspective in addressing all questions on personality.
The limitations of the present study are obvious. First, developmental trajectories and diagnoses of childhood-onset neuropsychiatric disorders assessed in a cross-sectional study, even within a framework of having access to a wealth of retrospectively derived childhood information from medical/psychiatric records and relatives, must be cautiously interpreted. Second, studies involving patients undergoing highly specialized assessments may overselect nonspecific symptoms common to a wide variety of diagnostic “conditions.” Both in-depth clinical studies and large-scale, population-based, prospective cohorts are needed to further test the hypotheses presented in this article.