Over the past hundred years, alcohol-related problems have been described through an estimated 30 or more evolving diagnostic schemes
(1,
2). Most of these rubrics focused on a unitary disorder, without distinguishing between potential subgroups
(3–
5). Then, in 1980, DSM-III subdivided alcoholism into the two categories of abuse and dependence, with the latter requiring evidence of tolerance or withdrawal
(5–
7). DSM-III-R continued this categorical approach, while broadening the concept of dependence, after which DSM-IV took steps to increase even further the distinction between abuse and dependence
(3,
5–
9).
Several studies have evaluated the possible clinical implications of the DSM-III-R alcohol abuse and dependence criteria
(8,
10). Fewer investigations, however, have adequately addressed the meaning of the DSM-IV criteria for abuse and dependence, which is a reflection of the more recent publication of DSM-IV. A field trial tested the criterion items from DSM-III-R and other systems in more than 1,000 general- and treatment-population subjects; the results indicated the clustering together of seven items into what might be called dependence and, separately, four items into what might be called abuse
(3,
11). The latter category focused on substance-related social, occupational, interpersonal, and legal problems. Several other studies have supported separate factor loadings for items used for abuse and dependence
(12–
16). However, not all studies have been in agreement
(17–
19), including at least one that questioned the existence of a single dimension within dependence
(20).
Other investigations have evaluated the DSM-IV scheme in comparison with other diagnostic systems in the proportions of individuals diagnosed with abuse or dependence. The requirement of having three of seven items for a diagnosis of DSM-IV dependence resulted in slightly fewer people being labeled dependent than when DSM-III-R criteria were used, although the DSM-IV rates were more comparable to those obtained with the use of DSM-III and ICD-10 criteria
(3,
8). The level of agreement (kappa) between DSM-IV and both DSM-III-R and ICD-10 for the diagnosis of dependence has been reported to be about 0.80, whereas the reported level of agreement between DSM-IV and DSM-III was 0.60
(8). The retest reliability of the DSM-IV dependence diagnosis was of similar magnitude
(21). For the diagnosis of abuse, however, the less restrictive requirement of having any one of four possible areas of problems resulted in more people fulfilling DSM-IV abuse criteria than was seen for any of the three other diagnostic systems, with the kappa for agreement between DSM-IV and DSM-III-R diagnoses of abuse ranging from less than 0.50 to as high as 0.62
(8,
12,
15,
21).
An issue related to coverage and agreement across systems is the relative prevalence of abuse versus dependence. In DSM-III-R, with the listing of only two criterion items for abuse, several studies reported much lower rates of abuse than dependence
(8,
22). In DSM-IV, however, the divergence might not be as great
(4,
8,
9,
12). In viewing these results, it is important to remember that the relative rates of abuse and dependence often do not take into account the diagnostic algorithms used in which the large majority of people with alcohol dependence would also meet criteria for abuse.
Another approach for evaluating the clinical implications of the DSM-IV diagnoses of alcohol abuse and alcohol dependence is to determine how each label relates to a series of characteristics, or clinical validators, of people who meet criteria for the disorders. In this context, several surveys have reported relatively clear differences between individuals with alcohol dependence and those with no alcohol diagnosis
(9,
15,
23–
25). These included high levels of alcohol consumption, higher rates of several nondiagnostic alcohol problems (e.g., blackouts), and more frequent histories of treatment for those with dependence. Most evaluations also reported differences between subjects with alcohol abuse and subjects with no diagnosis, although the distinction on these variables between people with abuse and dependence were less dramatic.
Perhaps the most clinically relevant evaluation occurs when longitudinal studies are used to determine the prognostic significance of the diagnoses
(26,
27). Similar to studies that evaluated DSM-III-R criteria
(4), evaluations of the DSM-IV criteria have shown significantly different patterns of alcohol-related problems over time for subjects in the general population with alcohol abuse, dependence, and no alcohol diagnosis. A study of heavier drinkers (people who had consumed five or more drinks in an evening the prior year) found that during a 1-year follow-up of men and women with alcohol dependence, 71% continued to endorse one or more of the 11 DSM-IV abuse/dependence criterion items
(23,
28). For the subjects who reported alcohol abuse at study entry, only 6% went on to fulfill criteria for dependence at follow-up, whereas 33% continued to meet criteria for abuse, and 61% experienced no problems with alcohol. The 1-year rate of new cases among the people with no alcohol diagnosis at study entry was 7% for dependence and 4% for abuse. Distinctions in the clinical course between abuse and dependence were also supported by differences reported at a 3-month follow-up in the average and maximum number of drinks per day
(11).
In short, to our knowledge, there are few relatively long-term longitudinal evaluations of the clinical course of subjects with DSM-IV alcohol abuse or dependence. This report uses data from a 5-year follow-up of 435 high-functioning men to evaluate the rates of onset and cessation of alcohol-related problems associated with DSM-IV abuse and dependence.
Method
Subjects were 435 men who were originally part of a 10-year prospective study of 453 sons of alcoholics and comparison subjects
(29) who had given written informed consent to participate in a 5-year follow-up evaluation (approximately 15 years after study entry). Two of the subjects had died during years 10–15, but data were obtained from resource persons and death records. Four additional individuals were not yet available for their follow-up interview because, for example, they lived outside the United States. Of the remaining 14 individuals, two had died during the first 10-year follow-up period, and no further follow-up had been done. Thus, only 12 people (2.6%) appropriate for follow-up refused to cooperate.
The original subjects were initially selected from the approximately 70% of men, 18 to 25 years old, who each year between 1978 and 1988 responded to random mailings to nonacademic staff or students at the University of California, San Diego
(29,
30). The initial questionnaire, which was followed by a structured personal interview, identified drinking, but not alcohol-dependent, individuals who were physically healthy, had experience with alcohol, and did not have bipolar manic depressive disease or schizophrenia. The subjects were Caucasian and Hispanic men who had an alcoholic biological father (positive family history of alcoholism); those with a negative family history were included as comparison subjects. All men included in the follow-up also participated in one of several alcohol challenge paradigms, which have been reported elsewhere
(29).
All 453 initial subjects were successfully located almost 10 years after their initial laboratory evaluation
(29). Data gathered at the 10-year follow-up assessment, when the subjects were approximately age 30, were used to establish the alcohol-related diagnoses reported here. Personal interviews were carried out with subjects and additional informants (usually the spouse), and blood samples along with urine drug toxicology screening results were obtained for state markers of heavy drinking at this 10-year assessment. A structured face-to-face interview, based on the Schedule of Affective Disorders and Schizophrenia
(31), was used to evaluate the clinical course of subjects over the preceding decade. Prior reports from this study group used the criteria of DSM-III-R
(29,
30), but data were also gathered that were relevant to DSM-IV criteria. Thus, in the current analyses, the diagnostic categories of alcohol abuse and alcohol dependence were recomputed according to DSM-IV criteria.
All men who were alive at the time of the 10-year follow-up assessment and who gave informed consent for continued study were located and contacted on the approximate 5-year anniversary of their 10-year evaluation. This assessment, carried out approximately 15 years after initial testing, gathered data regarding the most recent 5-year history of substance use disorders and additional psychiatric diagnoses from personal interviews with subjects and resource persons as described for the 10-year assessment. Following the diagnostic algorithm in DSM-IV, an emphasis was placed on the occurrence pattern of the seven dependence and four abuse items (11 items overall).
In this study, we compared the 5-year clinical course of subjects who, at year 10 when they were about age 30, fulfilled criteria for alcohol dependence (N=63, 93.7% of whom also met criteria for abuse) or alcohol abuse (N=79) or had no alcohol use disorder (N=293). The 5 years that led to the 15-year assessment for individuals in each of these diagnostic groups were compared regarding the pattern of the 11 DSM-IV abuse/dependence criterion items. Then, the characteristics at the 10-year assessment that predicted the patterns of alcohol-related problems over the next 5 years were established. Statistical evaluations for comparisons across groups used analyses of variance for continuous variables. Categorical data were compared across groups by using chi-square tests along with appropriate post hoc evaluations. Finally, to facilitate interpretation of these descriptive data, a logistic regression analysis was used to determine the optimal combination of characteristics at the 10-year assessment that predicted problems during the subsequent 5 years.
Results
At the 10-year assessment, the 435 men reported here were a mean of 31.3 years of age (SD=2.9), had an average of 15.9 years of education (SD=1.5), and had a median annual income of $37,992. By the time of the 15-year assessment, they had been followed an average of 13.7 years (SD=2.0). The group was predominantly Caucasian (96.6%, N=420), with the remainder primarily Hispanic, which was a reflection of the original selection criteria
(29,
30). At the 10-year follow-up assessment, 59.3% (N=258) were married, 4.6% (N=20) were separated or divorced, and 36.1% (N=157) were single (never married). Two hundred thirty-three subjects (53.6%) had an alcohol-dependent first-degree relative, which exceeded the rate of the original study (50.0%) because over the years some of the comparison subjects (who by definition had a negative family history of alcoholism) had a close relative develop an alcohol-related diagnosis.
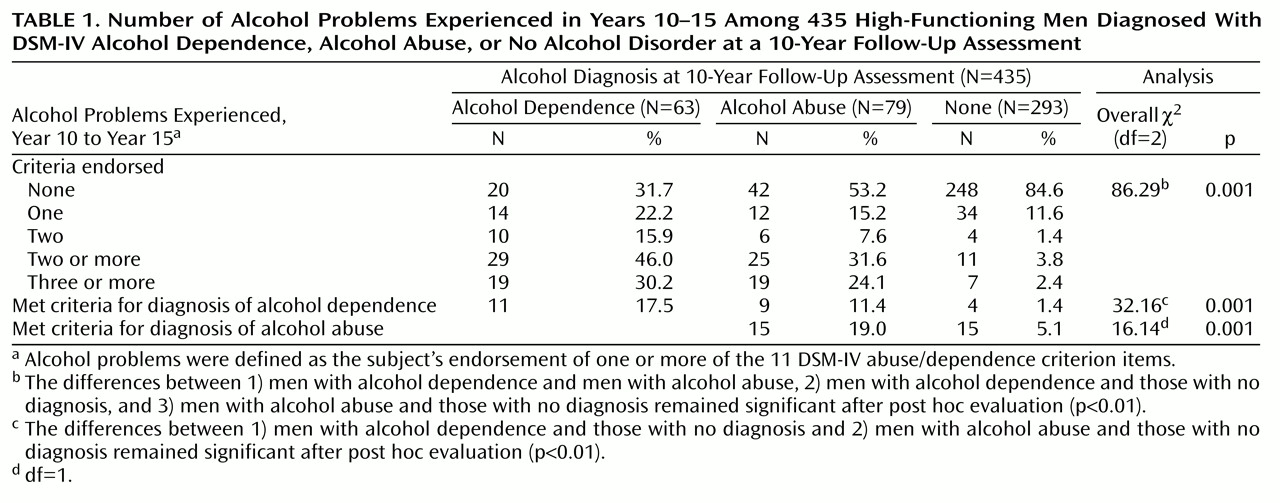
As shown in
Table 1, during the 5 years after the 10-year follow-up assessment, men diagnosed with alcohol abuse, alcohol dependence, or no alcohol disorder differed significantly on the appearance pattern of the 11 DSM-IV abuse/dependence criterion items. Those diagnosed with alcohol dependence at the 10-year assessment were the least likely to have had no alcohol problems during years 10–15, the most likely to have had two or more difficulties, and had the highest proportion who endorsed three or more of the 11 DSM-IV abuse/dependence criterion items at the 15-year assessment. Fewer than one in five men with alcohol dependence at year 10 maintained this diagnosis at year 15, but the rate was significantly higher than that of the other groups (
Table 1).
At the other extreme, 84.6% of the men who had no alcohol-related diagnosis at the 10-year assessment remained free of the 11 alcohol problems during years 10–15; only 5.1% reported alcohol abuse, and 1.4% developed dependence. The 79 men who reported alcohol abuse at the 10-year assessment demonstrated a course that was intermediate between those for the other two groups: at the 15-year assessment, 53.2% (N=42) had experienced no problems, 31.6% (N=25) reported two or more difficulties, and 11.4% (N=9) went on to develop alcohol dependence. While not shown in
Table 1, when the data were evaluated separately for subjects with and without a family history of alcoholism, the results were similar. Furthermore, the general conclusions did not change when subjects who received treatment during years 10–15 or those who were abstinent at the 10-year assessment were excluded.
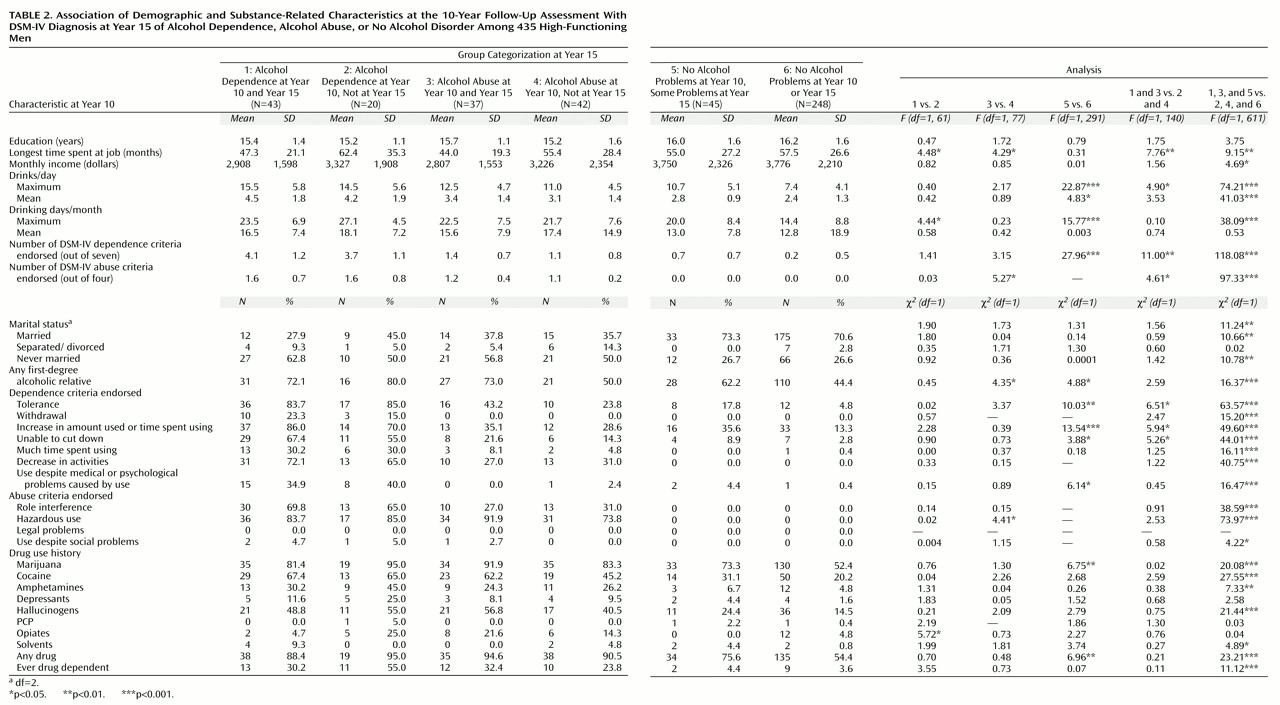
Table 2 examines the characteristics at the 10-year assessment that were associated with the occurrence of one or more of the 11 DSM-IV abuse/dependence criterion items in years 10–15 for each of the groups in
Table 1. The overarching question is the manner in which men who went on to experience alcohol-related problems (groups 1, 3, and 5) differed at the 10-year assessment from those men who did not develop such difficulties (groups 2, 4, and 6). Those who experienced alcohol problems during years 10–15 were less likely to have been married, were more likely to have been single, had held their longest job for a shorter period of time, and reported a lower monthly income at the time of the 10-year assessment. These subjects more often had an alcoholic first-degree relative. During the decade before the 10-year follow-up evaluation, these subjects reported higher maximum quantities and frequencies of drinking and were more likely to have endorsed most of the alcohol dependence problems. The men with a higher risk for subsequent alcohol problems were also more likely to have used many of the categories of drugs of abuse, and there were differences regarding the proportion who had ever been drug dependent. However, the direction of these relationships to drug items was inconsistent across groups.
Perhaps reflecting the relatively small group sizes, fewer differences in outcome reached significance when evaluated within those diagnosed with alcohol dependence (group 1 versus group 2), alcohol abuse (group 3 versus group 4), or no alcohol disorder diagnosis (group 5 versus group 6). However, many of the aforementioned characteristics applied across these groups, although there were several exceptions. The largest number of these subgroup differences that predicted future problems was seen for those who went on to develop problems but who had no alcohol diagnosis at year 10.
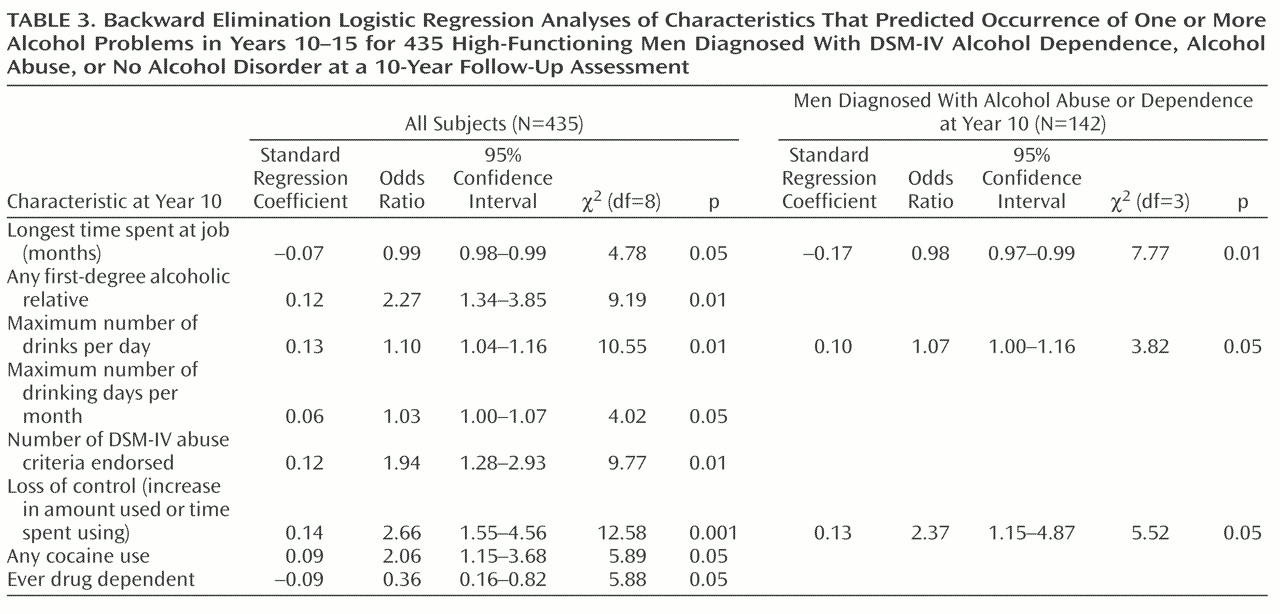
The results in
Table 2 do not evaluate which of the characteristics at year 10 predicted outcome when examined in the context of the other predictors. Thus, to facilitate interpretation of the descriptive data and to compensate for the large number of statistical comparisons in
Table 2,
Table 3 reports the results of entering all items in
Table 2 into a backward elimination logistic regression procedure to predict occurrence of one or more future alcohol problems. The dependent variable here is whether any of the 11 possible alcohol problems were reported during the year 15 follow-up. We first calculated the results when appropriate variables were used to predict the occurrence among all 435 subjects of one or more of the 11 alcohol problems during years 10–15 (i.e., groups 1, 3, and 5). Eight items entered the equation (overall χ
2=130.00, df=8, p<0.00001). Variables from the 10-year assessment that contributed significantly included a shorter maximum period spent at any one job, the presence of an alcoholic relative, higher maximum alcohol quantities and greater drinking frequencies over the first 10 years, the number of the four abuse items endorsed, and endorsement of having used alcohol longer or in higher amounts than intended. Two drug-related items also predicted problems, including ever having used cocaine and any drug dependence diagnosis, although, perhaps as a reflection of the performance of the latter among men with alcohol dependence in
Table 2, the relationship was negative. A simultaneous-entry logistic regression was also significant (χ
2=151.05, df=30, p<0.00001), with contributions from the presence of alcoholic relatives, the maximum quantity of alcohol intake, cocaine use, and any drug dependence diagnosis.
Using similar procedures, we then limited the subjects to those diagnosed with alcohol abuse or dependence at the 10-year assessment (
Table 3). The backward elimination approach revealed that the predictors of alcohol problems (χ
2=18.26, df=3, p=0.0004) included a shorter period at the longest job, a greater number of drinks per day, and endorsement of having used alcohol longer or in greater amounts than intended. The simultaneous-entry procedure (χ
2=45.01, df=30, p<0.04) identified only one significant item: ever having used cocaine.
While not the major focus of this study, it was possible to compare how well the abuse/dependence labels at the 10-year assessment predicted the development of the 11 DSM-IV abuse/dependence criterion items as compared to a simple count of the DSM-IV items endorsed at year 10. The correlation between the abuse/dependence diagnostic approach and the occurrence of one or more problems during years 10–15 was significant (r=0.42, df=433, p<0.0001) as was the correlation for the number of the 11 problems at year 10 and the subsequent course (r=0.48, df=433, p<0.0001). Significant correlations were also seen between the total number of problems during years 10–15 and both diagnostic label at year 10 (r=0.44, df=433, p<0.0001) and number of criterion items endorsed at year 10 (r=0.50, df=433, p<0.0001).
Discussion
This study presents information on the 5-year rate of occurrence of the 11 DSM-IV alcohol abuse/dependence criterion items in 435 high-functioning men (97.3% of the 447 men appropriate for this study). The initial 10-year follow-up evaluation of these subjects, half of whom had an alcoholic close relative, revealed that one-third met criteria for an alcohol-related disorder, either alcohol abuse (18.2%) or alcohol dependence (14.5%). The subsequent follow-up of subjects at year 15 revealed a significantly different clinical course for men diagnosed with alcohol dependence, alcohol abuse, or no alcohol disorder, such as the occurrence of one or more of the 11 possible alcohol problems (endorsed by 68.3%, 46.8%, and 15.4%, respectively).
Overall, the greatest differences in the 5-year course after the 10-year follow-up assessment were seen for those subjects with alcohol abuse or dependence compared to those with no diagnosis. There were fewer distinctions in the number of problems reported for those with dependence versus those with abuse. These results are similar to those reported for the 1–3-year follow-ups of individuals with DSM-III-R or DSM-IV abuse and dependence
(4,
23). Consistent with an earlier study
(23), the current analyses followed the DSM-IV guidelines of noting a continuation of dependence whenever one or more of the 11 criterion items was reported during the follow-up period and applied similar criteria for abuse. As has been demonstrated in additional evaluations
(32,
33), the present results are also consistent with the conclusion that the course of alcohol abuse or dependence involves fluctuations between levels of problems, with only a minority of individuals maintaining the full syndrome during a follow-up interval.
Only 11.4% of the 79 men who reported alcohol abuse at the 10-year assessment developed alcohol dependence during years 10–15. While this figure was significantly higher than the 1.4% of the 293 people with no initial alcohol diagnosis who went on to develop dependence, the results indicate that the majority of people with abuse do not evolve into a full dependence syndrome. Finally, with regard to the 5-year course of problems, 6.5% of even this high-functioning group of men developed their first onset of abuse (5.1%) or dependence (1.4%) between the ages of about 30 and 35. Of course, these results might reflect the fact that one-half of the original subjects had an alcoholic close relative, and figures for highly educated men in the general population might be lower.
The relative rates of alcohol abuse and alcohol dependence in this group are also of interest. In all stages of the evaluation, more subjects met criteria for DSM-IV abuse than dependence. If one includes the almost 94% of men with dependence at the 10-year assessment who also met criteria for abuse, these data support the conclusion that the less-demanding diagnostic entity of DSM-IV abuse is, indeed, the more prevalent diagnosis.
The data in
Table 2 indicate that subjects were not equally vulnerable to alcohol-related problems during the 5 years between the 10-year and 15-year assessments. Even after entering relevant variables into a logistic regression analysis, characteristics noted at the 10-year assessment that independently predicted alcohol-related difficulties included 1) the presence of an alcoholic relative, 2) a shorter maximum period spent at any one job (an attribute associated with lower levels of life functioning), 3) evidence of higher quantities and greater frequencies of alcohol intake, 4) more alcohol-related problems (especially using alcohol in greater amounts or for longer periods than intended), and 5) several drug-related phenomena. Regarding the latter, for the dependence group there was some indication that those who used drugs (especially opioids) were less likely to develop future problems with alcohol. Perhaps these men moved on to develop dependence on these other drugs and decreased their problematic use of alcohol. However, in general, similar types of predictors of alcohol-related problems operated for people with or without alcohol-related diagnoses at the 10-year assessment. These results support the conclusion that even in this group of high-functioning men, evidence of less life stability and more intense involvement with alcohol at the 10-year assessment were related to a more severe course of alcohol problems in years 10–15.
The significance of the number of alcohol problems is important to note. The current study was not structured to compare the performance of DSM-IV alcohol abuse and dependence criteria to other categorical or dimensional approaches. The major finding is that the classification of abuse or dependence at the 10-year assessment strongly predicted classification at the 15-year assessment, but the results do not address the relative merits of categorical- and continuum-based diagnostic systems.
Finally, these results must be evaluated in the context of the methodologies used. While the current study group was moderately large, only 63 individuals had a diagnosis of alcohol dependence at the beginning of the current follow-up period, indicating that larger long-term follow-up studies are required before more definitive conclusions can be drawn. In addition, the data were gathered from high-functioning Caucasian men, half of whom had an alcoholic relative, and it cannot be certain if the present results apply equally to other groups of individuals. Also, the analyses were established to evaluate the onset and cessation of alcohol-related problems for men with DSM-IV diagnoses of dependence or abuse. Thus, the results do not shed light on whether alternative approaches to diagnosing alcohol use disorders might be superior to DSM-IV criteria.
In conclusion, the current data report the rate of development and resolution of the symptoms of alcohol abuse and dependence over time. The classification of abuse or dependence predicted classification 5 years later, even among relatively high-functioning men who were not chosen because of their participation in a treatment program. These two substance use disorders appear to be differentially related to the occurrence of one or more of the 11 DSM-IV abuse/dependence criterion items after 5 years of follow up. The results are consistent with the predictive importance of the 11 items but do not distinguish between a continuous liability or other cutoff points.