Obsessive-compulsive disorder (OCD) is a psychiatric condition with a lifetime prevalence of up to 3%
(1). The etiology of OCD is unknown, but data from challenge studies
(2) and from pharmacological trials
(3) have supported the involvement of the serotonergic system. Genetic studies have investigated possible variants of serotonergic system genes: the serotonin (5-HT) receptor gene variants 5-HT
2A and 5-HT
2C were found not to be associated to OCD
(4,
5), while mixed results were found for the serotonin transporter gene
(6,
7). The 5-HT
1Dβ receptor appears to be particularly interesting. It is a terminal autoreceptor, and challenge studies with nonselective ligands (e.g., m-CPP)
(2) showed an acute worsening of obsessive-compulsive symptoms. In addition, a worsening of OCD symptoms has been reported following acute administration of sumatriptan, a selective agonist of the 5-HT
1Dβ receptor
(2). On the other hand, in OCD patients resistant to conventional pharmacotherapy, improvements have been reported with chronic administration of sumatriptan
(8).
Method
Sixty-seven OCD probands were selected. All patients were administered the Structured Clinical Interview for DSM-IV (SCID) and the Yale-Brown Obsessive Compulsive Scale
(10). To be eligible for the study, patients had to have either both biological parents or at least one sibling living and willing to participate. The supposedly unaffected siblings were also administered the SCID, and those with any psychiatric disorders were excluded. Patients with a history of neurological or metabolic diseases, bipolar disorder, schizophrenia, or schizoaffective disorder, or with a positive history of substance dependence, were excluded. Written informed consent to participate in the study was obtained from all subjects. Genomic DNA was extracted from whole blood
(11), and genotyping of the G861 variant of the gene was performed by means of standard procedures
(9).
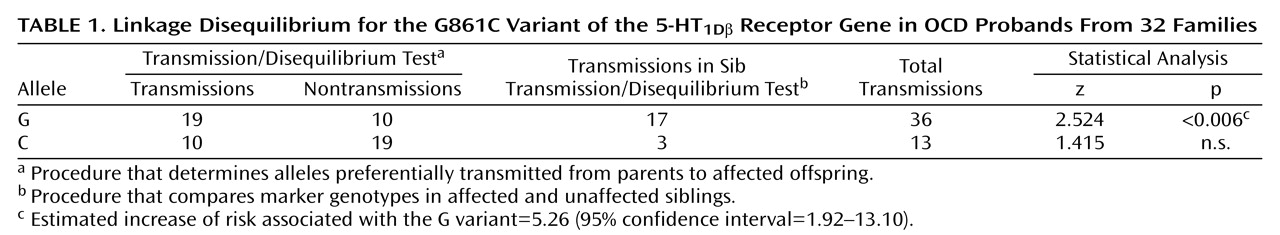
We tested for the presence of linkage disequilibrium between the 5-HT
1Dβ; receptor gene G861C polymorphism and OCD with the Transmission Disequilibrium Test/sib-Transmission Disequilibrium Test analyses
(12). This procedure combines the Transmission Disequilibrium Test, which examines alleles preferentially transmitted from the parents to the affected offspring, with the sib-Transmission Disequilibrium Test, which compares the marker genotypes in affected and unaffected siblings. We specifically tested for excess of transmissions to the affected siblings by using the z test statistic, one-tailed
(12).
Discussion
Our results indicate a significant linkage disequilibrium between the G861C variant of the 5-HT
1Dβ receptor gene and OCD, with preferential transmission of the G allele to the affected subjects. Despite the fact that the silent G861C variant has been claimed to not directly affect the function of the receptor, there are several other possibilities to explain the role of this polymorphism in the pathogenesis of OCD. First, as it has been hypothesized for other serotonin receptor genes (e.g., 5-HT
2A)
(13), one of the variants of the G861C polymorphism could induce different mRNA secondary structure, thereby affecting the efficiency of translation. Second, other polymorphisms may exist in the gene that could be in linkage disequilibrium with the G861C variant and be functionally relevant. Further investigations should focus on additional markers in the area and other possible variants of the gene. As seen with other complex disorders, more than one gene is expected to be involved in the etiology of OCD in a model in which each gene per se has a relatively small effect in increasing the risk for the disease. In our case, the estimated increase of risk to develop OCD, as an effect of the presence of the G variant, was equal to 5.26 (
Table 1). The possibility that the C variant may play a protective role in the development of OCD is also possible.
The OCD phenotype is heterogeneous, as suggested by the variability in the response to medications in both acute and chronic administrations
(2,
14). The investigation of the distribution of this and other 5-HT
1Dβ receptor gene polymorphisms in OCD patients designated as responsive versus nonresponsive to medication will be useful.
Finally, even though it is impossible at this time to define more precisely the role of the 5-HT1Dβ receptor gene in OCD, the magnitude of the effect that we observed deserves further investigations. Only a combined strategy, which implies an exhaustive exploration of the OCD phenotype and a more extended knowledge of the genetic complexity of the 5-HT1Dβ gene, will be able to shed light on this potential component of the etiology of OCD.