Exposure to nutritional deficiency during fetal life may be a risk factor for developing schizophrenia. A relation with nutritional deficiency has been suggested by a twofold increase in the incidence of schizophrenia in a birth cohort in which the first 2 months of fetal development occurred between February and April 1945
(1). These months at the end of World War II corresponded with the most severe period of the Dutch Hunger Winter. Moreover, prenatal exposure to famine during the first trimester has been reported to result in an increase in the prevalence of central nervous system anomalies
(2).
The subtle brain abnormalities found in schizophrenia have been attributed to neurodevelopmental factors that occur early in life
(3). However, it is not known whether prenatal events contribute to structural brain abnormalities in schizophrenia. We tested the hypothesis that first-trimester exposure to the Dutch Hunger Winter was associated with specific brain abnormalities in schizophrenia.
Method
Five male and four female patients with schizophrenia completed the magnetic resonance imaging (MRI) procedure and interviews. The patients had been admitted for schizophrenia at least once between 1970 and 1992. They were born between October 15 and December 31, 1945, and were thus exposed to the most severe period of the Dutch Hunger Winter during their first trimester of gestation. Despite profound efforts to trace and include all 27 patients from a previous report
(1), these nine schizophrenic patients with prenatal famine exposure were those ultimately assessed for this study. Their mothers had been exposed to very low food rations from February to April 1945
(4). The presence of DSM-IV schizophrenia was determined by using the Comprehensive Assessment of Symptoms and History
(5) and the Schedule for Affective Disorders and Schizophrenia—Lifetime Version
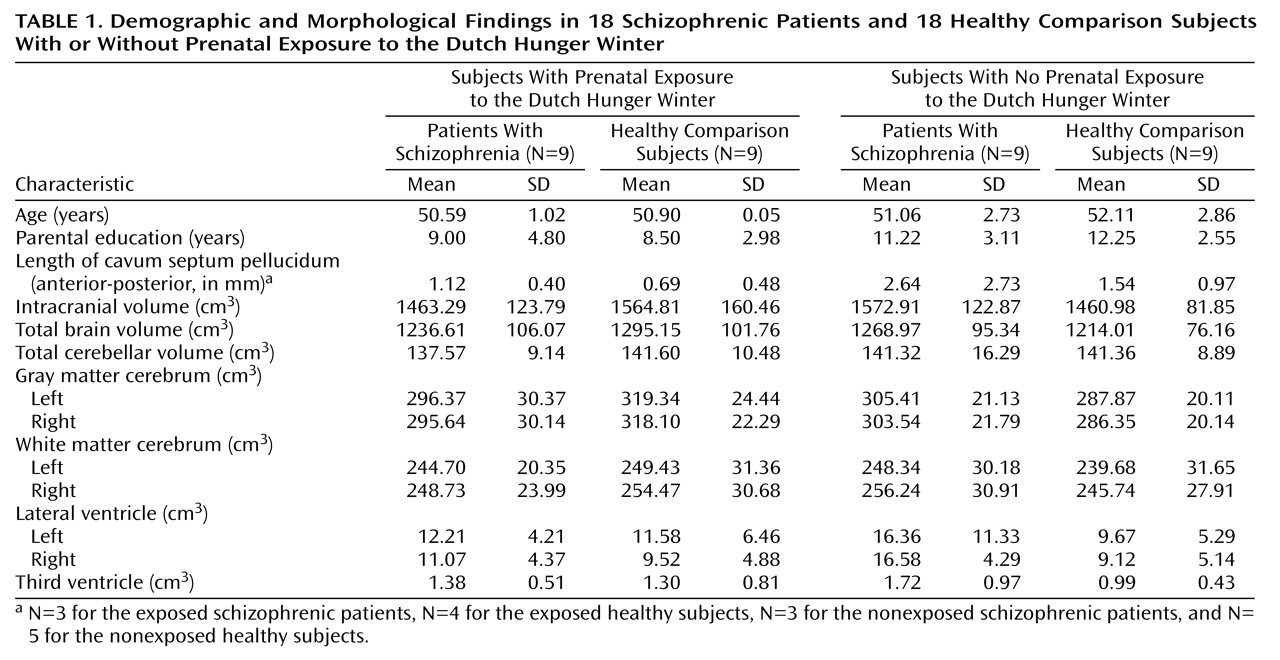
(6), which were administered by a psychiatrist or psychologist. Subjects with DSM-IV-defined alcohol and drug abuse or dependence were excluded. Five male and four female healthy subjects who met the same criteria for prenatal exposure to the Dutch Hunger Winter as the schizophrenic patients were recruited by advertisements in national newspapers. For comparison, seven male and two female patients with schizophrenia and seven male and two female healthy subjects, all with no prenatal exposure during the first trimester of gestation to the Dutch Hunger Winter (i.e., born between October 15 and December 31 during the years 1941–1944 or 1946–1949), underwent the same procedure. The four groups did not differ with respect to age (F=0.95, df=3, 32, p=0.43) or years of parental education (F=2.26, df=3, 26, p=0.11) (
Table 1). All subjects provided written informed consent before participation.
Magnetic resonance images of the whole head were acquired on a Philips NT scanner operating at 1.5 T. A T1-weighted coronal three-dimensional fast field echo (TE=4.6 msec, TR=30 msec, flip angle=30˚, field of view=256 × 256 mm2, thickness=1.2 mm) and a T2-weighted coronal dual echo turbo spin echo (TE1=14 msec, TE2=80 msec, TR=6350 msec, field of view=256 ≥256 mm2, thickness=1.6 mm) were used for the quantitative measurements. A T2-weighted axial dual echo turbo spin echo (TE1=9 msec, TE2=100 msec, TR=2200 msec, field of view=250 ≥250 mm2, thickness=5.0 mm, gap=1.2 mm) was acquired for clinical neurodiagnostic consensus evaluation of brain abnormalities (e.g., focal white matter hyperintensities and lacunar infarcts but excluding brain atrophy) performed by two neuroradiologists.
Postprocessing was done on Hewlett Packard 9000 series workstations. Images were coded, transformed into Talairach frame, and corrected for scanner nonuniformity
(7). The incidence (interrater reliability kappa=0.83) and length (intraclass correlation coefficient=0.86) of the cavum septum pellucidum was determined with the three-dimensional fast field echo. Brain region volumes were segmented with the use of fully automated computer programs on the basis of histogram analyses, mathematical morphological operations for the dual echo turbo spin echo (intracranial volume) and three-dimensional fast field echo (other structures), and by (automatic) anatomical decision rules (ventricles and cerebellum) that used the foramen magnum as inferior boundary. All images were checked after the measurements and corrected manually if necessary. High interrater reliability, determined from measurements of 10 brains, was found for intracranial volume (0.99) and the volume measures for total brain (0.99), cerebellum (0.95), lateral ventricles (0.99), and the third ventricle (0.95).
Analysis of variance was performed for intracranial volume, and repeated measures analysis of covariance was performed for total brain, cerebellum, gray and white cerebral matter, and lateral and third ventricle volumes. Group (schizophrenic patients, healthy subjects) and prenatal Hunger Winter exposure (exposed, not exposed) were between-subject factors and, if applicable, side (left, right) and matter (gray, white) were within-subject factors, with intracranial volume as covariant. Effects of prenatal Hunger Winter exposure or group on the incidence and length of cavum septum pellucidum were evaluated by using chi-square analysis and Mann-Whitney U nonparametric tests (corrected for ties). Incidences of brain abnormalities determined during the neurodiagnostic exam were evaluated by using one-tailed Fisher’s exact tests.
Results
Among the subjects with prenatal Hunger Winter exposure, brain abnormalities were found in four of the schizophrenic patients and two of the healthy subjects. Of those without prenatal Hunger Winter exposure, none of the schizophrenic patients and one healthy subject had such abnormalities. Analysis revealed an effect of prenatal Hunger Winter exposure (p=0.04, Fisher’s exact test) but not of schizophrenia (p=0.50, Fisher’s exact test) on the incidence of brain abnormalities, of which five included focal white matter hyperintensities. No group or exposure effects were found for the incidence or length of cavum septum pellucidum.
Morphological results are shown in
Table 1. There were no main effects of Hunger Winter exposure or group for intracranial volume. An interaction effect of schizophrenia with prenatal Hunger Winter exposure for intracranial volume was found (F=6.52, df=1, 32, p=0.02). The mean intracranial volume of schizophrenic patients with prenatal famine exposure was smaller than that of schizophrenic patients without such exposure. In addition, the intracranial volume of healthy subjects with prenatal famine exposure was larger than that of healthy patients without such exposure. No main effects of prenatal Hunger Winter exposure or schizophrenia for total brain volume were revealed. There were no interaction effects with matter and side. Cerebellar, lateral, and third ventricular volume did not show effects. Finally, there was no effect of sex on the incidence of brain abnormalities or on the interaction effect of schizophrenia with Hunger Winter exposure for intracranial volume.
Discussion
This study found that exposure during the first trimester of fetal development to the Dutch Hunger Winter of 1945 was associated with an increase in the incidence of brain abnormalities, in particular of focal white matter hyperintensities. Moreover, in patients with schizophrenia, prenatal Hunger Winter exposure was associated with decreased intracranial volume.
The increased incidence of brain abnormalities in schizophrenic patients with prenatal famine exposure suggests that environmental factors that influence early brain development increase the risk for white matter hyperintensities and other focal brain abnormalities. Although white matter hyperintensities were also found in healthy subjects with prenatal famine exposure, these abnormalities may nonetheless be related to schizophrenia (i.e., more common in exposed patients), since statistical power was insufficient to assess an interaction between exposure and schizophrenia. Although the precise pathophysiology of white matter hyperintensities is unknown, white matter hyperintensities have been related to an inadequate supply of nutrients necessary to sustain and replace normally catabolized myelin, with loss of myelin leading to reactive gliosis
(8). Moreover, prenatal micronutrient deficiencies, probably implicated in the Hunger Winter
(9), have been reported to cause defects of the central nervous system
(10). The white matter hyperintensities in the schizophrenic patients and healthy subjects with prenatal famine exposure could therefore conceivably be the result of nutritional deficiency early in (fetal) life.
The finding that intracranial volume was decreased in patients with schizophrenia who had been exposed to the Hunger Winter as compared to schizophrenic patients without such exposure suggests that stunted early brain development may be a risk factor for developing schizophrenia, since early in (fetal) life intracranial volume is largely dependent on brain growth
(11). This neurodevelopmental aberration could be a result of an interaction between a genetic predisposition and environmental factors. Specifically, one could hypothesize that the genetic predisposition is either expressed or elicited by prenatal nutritional deficiencies. An interaction between prenatal Hunger Winter exposure and genetic risk appears plausible, since schizophrenic patients without prenatal Hunger Winter exposure (but assumed to carry genes that increase the risk of schizophrenia) failed in this study to show a decreased intracranial volume. Indeed, multiple risk factors appear to be implicated in schizophrenia that result in decreased intracranial volumes in some, but not all, schizophrenic patients.
There are a number of qualifications to add to our conclusions. Factors not related to nutrition such as psychosocial stressors may have contributed to the aberrant brain development in subjects with prenatal famine exposure. However, it is unlikely that psychosocial stressors explain the findings, since psychosocial stressors played a role throughout World War II
(12) and were not limited to the circumstances during the Dutch Hunger Winter. Moreover, the results have to be considered as preliminary, since only a limited number of individuals with prenatal famine exposure could eventually be included in the MRI study, which restricted its statistical power.