An extensive literature exists on the significant relationship between childhood disruptive behavior and the development of alcoholism as an adult. Examples of this literature include studies by Robins
(1,
2), who demonstrated that juvenile delinquency was associated with childhood conduct disorder on the one hand and a variety of adult psychopathology (including alcoholism and substance abuse) on the other. Rydelius
(3), in his study of Swedish adolescents, found that adolescents who displayed aggressive acting out behavior, poor impulse control, restlessness, and difficulties concentrating were more likely as adults to have an alcohol-related diagnosis. McCord
(4) first reviewed the records of 203 boys who were participants in a delinquency prevention program and then interviewed them when they were between 43 and 53 years of age. One of the key factors that predicted the development of adult alcoholism was a mother’s inability to control her son’s disruptive/disinhibited behavior. Caspi et al.
(5) reported on a group of children who were followed beginning at age 3 for 18 years. During the initial screening process, the children were classified into one of five different groups on the basis of behavior during the testing situation: undercontrolled (impulsive, restless, distractible), inhibited (shy, fearful, easily upset), well adjusted (exhibited normal behavior for age), confident (enthusiastic, eager, adjusted to new situations quickly), and reserved (timid and uncomfortable, although able to perform tasks). At age 21, male, but not female, subjects in the undercontrolled category were most likely to have a DSM-III-R diagnosis of alcohol dependence.
A second, emergent literature has described the relationship between early first use of alcohol and the development of alcoholism as an adult. Grant and Dawson
(6) reported that 40% of young adults (age=18–29 years) who initiated drinking before the age of 15 were classified as alcohol dependent, whereas the rate of alcohol dependence was approximately 20% among those who began drinking after the age of 21.
Similar relationships of childhood disruptive behavior and early alcohol use to the development of adolescent alcoholism are just beginning to be reported
(7). The present study is designed to further explore the chronological relationships among the onset of specified childhood disruptive behavior diagnoses, first use of alcohol, and the development of adolescent alcoholism. The subjects in this study were taken from a group of adolescents studied as part of the Collaborative Study on the Genetics of Alcoholism. This cohort, along with their biological families, was comprehensively studied to obtain the clinical data necessary to establish whether the subjects had a disruptive behavior diagnosis as well as the age when they first used various substances.
Method
The Collaborative Study on the Genetics of Alcoholism was designed to study potential causes of alcoholism through collection of demographic data, laboratory analyses, and psychiatric assessments. Institutional review boards at all participating sites independently approved the study and all components. Parents provided informed consent and adolescents informed assent for participation in this study. Ascertainment rules and procedures have been well described by Begleiter et al.
(8). In brief, approximately 70% of the families recruited for the study were extended pedigrees at high genetic risk for alcohol dependence (i.e., the families contained an adult proband and at least two adult first-degree relatives who met DSM-III-R criteria for alcohol dependence and Feighner criteria
[9] for definite alcoholism). This recruitment strategy resulted in a large number of nuclear families with adolescent children in which most, but not all, contained at least one parent with a diagnosis of alcohol dependence. The remaining families were comparison subjects from the community who were recruited from dental and family practice clinics, businesses, churches, and driver’s license renewal lists. Comparison families were not excluded if family members had a psychiatric disorder, including alcohol dependence. The comparison families were gathered to allow assessment of familial, psychiatric, and biological variables that might contribute to a higher risk for alcohol-related problems. In this study, these variables were used only to determine whether enough differences existed to prohibit the combining of alcohol-dependent adolescents from both family types
The subset of subjects reported here included all adolescents (age=13–17 years) for whom interview data were available on themselves and on both biological parents. The Semi-Structured Assessment for the Genetics of Alcoholism
(10) was used to interview all adults and was the basis for adult psychiatric diagnoses. Each adolescent was directly interviewed with the Child Semi-Structured Assessment for the Genetics of Alcoholism—Adolescent Form, which is derived in part from the Diagnostic Interview for Children and Adolescents
(11). A similar matching interview also was obtained from one of the adolescent’s parents (usually the mother) with the Child Semi-Structured Assessment for the Genetics of Alcoholism—Parent Form. All interviews were given by research assistants and subjected to rigorous quality control. First, interviewers from all sites of the Collaborative Study on the Genetics of Alcoholism took part in intensive, multiday sessions that incorporated both live and videotaped child and adult subjects as part of training. Second, interviews were systematically edited and, if necessary, subjects were recontacted before data entry. Finally, interviewers and editors participated in a monthly conference call to review subject data and minimize interviewer and site-specific drift.
Adolescent psychiatric diagnoses of attention deficit hyperactivity disorder (ADHD), conduct disorder, oppositional defiant disorder, and alcohol dependence were made by combining information from both adolescent and parent interviews such that a positive endorsement for a particular question was given if answered affirmatively by either the adolescent or parent. This is the method most commonly used in child psychiatry epidemiological studies
(12,
13). A 1-week test-retest administration of the adolescent and parent forms of the Child Semi-Structured Assessment for the Genetics of Alcoholism resulted in an overall mean kappa of 0.67 (SD=0.15) for the three disruptive behavior diagnoses evaluated in this study. The alcohol section of the Child Semi-Structured Assessment for the Genetics of Alcoholism consists of detailed questions covering quantity and frequency of use of various types of alcohol, the age at onset of various alcohol-related symptoms, and the level of impairment associated with these symptoms. A diagnosis of alcohol dependence was made if at least three of the nine DSM-III-R dependence criteria were present and if these symptoms clustered for at least 1 month. On the basis of this procedure, the 1-week test-retest kappa for a diagnosis of alcohol dependence was 0.86.
The total pool of subjects consisted of 182 adolescents from 119 comparison families and 437 adolescents from 266 high-risk families. Comparison families averaged 1.5 adolescents per family, and high-risk families averaged 1.6 adolescents per family, a nonsignificant difference. Additional descriptions of these 619 subjects have been previously published
(7,
14). On the basis of data from the adolescent and parent forms of the Child Semi-Structured Assessment for the Genetics of Alcoholism, 54 adolescents had a DSM-III-R diagnosis of alcohol dependence: 42 from high-risk families and 12 from comparison families. There was no significant difference between the high-risk and the comparison families in the percentage of adolescents with a diagnosis of alcohol dependence (9.6% and 6.6%, respectively). The percentage of families with two alcohol-dependent adolescents did not differ in the high-risk and comparison families: two comparison families (20.0%) accounted for four adolescents with alcohol dependence, and nine high-risk families (27.2%) accounted for 18 adolescents with alcohol dependence. Both groups of alcohol-dependent adolescents were enrolled into the study at a similar average age of approximately 16 years. Family income was examined by dividing annual income into nine blocks ranging from less than $10,000 to over $150,000. The median income block for both family types was $30,000–$39,999.
As expected, one variable did distinguish the two family types. Within the high-risk family type, 78.0% (N=341) of the adolescents had at least one parent with a diagnosis of alcohol dependence versus 31.9% (N=58) of the comparison family adolescents (χ2=119.5, df=1, p<0.001). However, among the adolescents who actually had an alcohol dependence diagnosis, the percentage of adolescents from the high-risk and the comparison families with at least one alcohol-dependent parent did not significantly differ (85.7% [N=36] and 66.7% [N=8], respectively; χ2=2.2, df=1, p=0.13). On the basis of these analyses, alcohol-dependent adolescents from high-risk and comparison families were grouped together for the remaining analyses.
Ages at onset for ADHD and oppositional defiant disorder were derived from the relevant diagnostic sections of the Child Semi-Structured Assessment for the Genetics of Alcoholism in which a global question (“How old were you [was your adolescent] the first time that you [he/she] had any of these things like…?”) was followed by the positive symptoms of the diagnoses. The age chosen to score this question was the younger of two ages, if they differed, from the child and parent interviews. In contrast, the Child Semi-Structured Assessment for the Genetics of Alcoholism contained an age-at-onset question for each specific symptom of conduct disorder, so the average age of all positive symptoms was used to calculate the age at onset. The age at onset for alcohol dependence was set as the age of first occurrence of symptoms determined through a series of 29 questions selected because they indicated actual impairment due to problematic alcohol use rather than mere alcohol experimentation (e.g., drinking considered excessive by other people; missed school at least three times because of drinking; quit school activity, job, or doing things with friends because of drinking; took a substance to relieve or avoid withdrawal symptoms of alcohol).
Additionally, since previous work
(7) has demonstrated an association between adolescent alcohol dependence and early use of alcohol, tobacco, marijuana, and other street drugs (amphetamines, cocaine, opiates, hallucinogens, or sedatives/hypnotics), these items also were explored. Because it was felt that adolescents often initiate the use of a substance without parental knowledge, the age of first use of a substance was derived solely from the adolescent form of the Child Semi-Structured Assessment for the Genetics of Alcoholism. A similar question existed for each substance and consisted of the phrase “What was the age when you first used [alcohol, tobacco, marijuana, or other street drugs]?” The age of first use for “other street drugs” was set as the age at which any one of the specified substances in this category was first tried.
Student’s t tests, chi-square analyses, and Fisher’s exact tests were performed on age and frequency variables. Comparisons of age at onset of the disruptive behavior diagnoses, age at first use of the four substance use categories, and age at onset of alcohol dependence were performed by using paired t tests. Because of the number of comparisons made, only those that resulted in a p value <0.01 were considered statistically significant.
Results
The initial analyses consisted of determining the rates of ADHD, oppositional defiant disorder, and conduct disorder in the entire cohort of 619 adolescents to determine whether there existed a relationship between these diagnoses and that of alcohol dependence. A diagnosis of ADHD was established in 61 of the adolescents. The rate of alcohol dependence was higher in children with ADHD; 14 (23.0%) of 61 children with ADHD also had a diagnosis of alcohol dependence versus 40 (7.2%) of 558 adolescents who did not have a diagnosis of ADHD (χ2=20.6, df=1, p<0.001). A similar relationship was seen between conduct disorder and alcohol dependence: 38 (31.4%) of the 121 adolescents with conduct disorder had the additional diagnosis of alcohol dependence versus 16 (3.2%) of the 498 adolescents who did not have a diagnosis of conduct disorder (χ2=97.2, df=1, p<0.001). There did not appear to be any relationship between having a diagnosis of oppositional defiant disorder and alcohol dependence. Of the 35 adolescents with oppositional defiant disorder, only two (5.7%) also had a diagnosis of alcohol dependence versus 52 (8.9%) of the 584 adolescents without this diagnosis. Therefore, further analyses involving oppositional defiant disorder and alcohol dependence will not be presented here.
The age at onset of alcohol dependence in the 54 adolescents was 14.0 years (SD=1.9). Thirty-nine (72.2%) of the alcohol-dependent adolescents had a diagnosis of ADHD (N=1), conduct disorder (N=24), or both (N=14). In all cases, the age at onset of alcohol dependence was significantly later than the age at onset of ADHD (mean age difference=7.9 years [SD=3.1]; t=7.9, df=14, p<0.001) or conduct disorder (mean age difference=5.5 years [SD=3.0]; t=11.3, df=37, p<0.001). Although the onset of ADHD occurred at an earlier age than conduct disorder in approximately 80% of the individuals with both diagnoses (mean age difference=2.0 years, SD=3.5), this was not significantly different.
Fifty-three adolescents used at least one other substance in addition to alcohol. Nine had tried just one other substance: tobacco (N=7) or marijuana (N=2). Twenty adolescents had tried at least two other substances: tobacco and marijuana (N=19) or tobacco and other street drugs (N=1). Twenty-four adolescents had tried all three classes of substances in addition to alcohol.
The ages of first use of tobacco or marijuana both occurred earlier than the age at onset of alcohol dependence, although this was only significant for first use of tobacco (mean age difference=1.4 years [SD=1.9]; t=5.3, df=50, p<0.001). Of the 25 adolescents who used other street drugs, 56.0% (N=14) initiated their use before the onset of alcohol dependence, but the average age difference of 0.4 years (SD=0.3) was not significant.
There was no significant difference in age at first use between alcohol and tobacco or between tobacco and marijuana. Alcohol use preceded marijuana use in 40 (88.9%) of the 45 adolescents who used both (mean age difference=1.2 years [SD=1.9]; t=4.3, df=44, p<0.001), and alcohol use preceded other street drug use in 24 (96.0%) of the 25 individuals who used both (mean age difference=2.1 years [SD=2.1]; t=5.0, df=24, p<0.001). First use of other street drugs occurred after first use of tobacco in 17 (68.0%) of 25 adolescents who used both (mean age difference=1.7 years [SD=1.9]; t=4.6, df=24, p<0.001). Similarly, first use of marijuana preceded other street drug use in 19 (79.2%) of the 24 adolescents who used both (mean age difference=1.3 years [SD=0.4]; t=3.4, df=23, p<0.001).
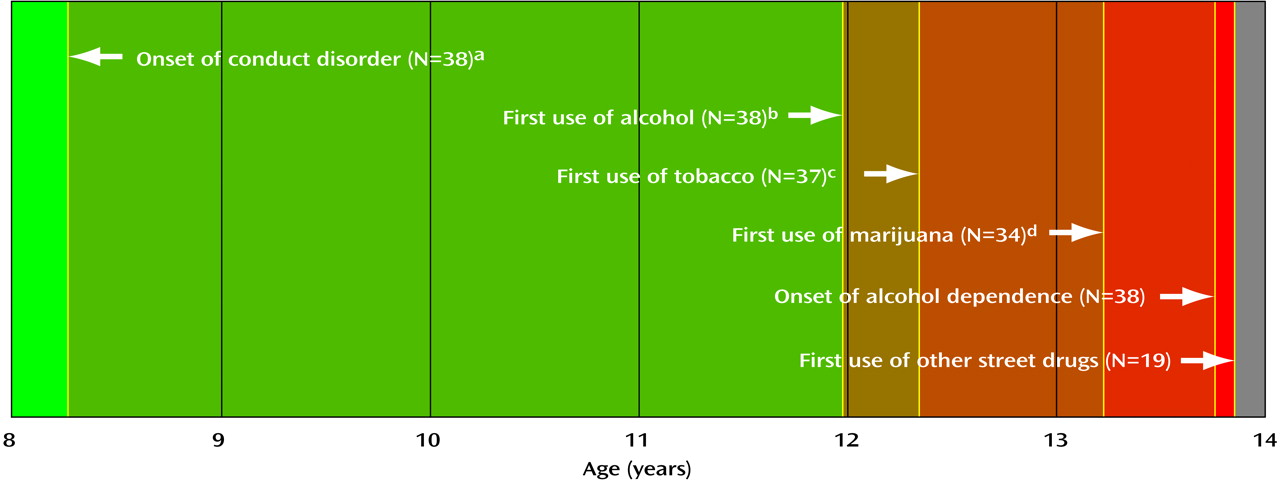
Among the 38 adolescents with the comorbid diagnoses of conduct disorder and alcohol dependence, there appeared to be a chronological progression (
Figure 1). The mean differences between the ages at onset of conduct disorder and onset of alcohol use (3.7 years, SD=3.0), tobacco use (4.0 years, SD=2.6), marijuana use (5.0 years, SD=3.3), alcohol dependence (5.5 years, SD=3.0), and other street drug use (5.5 years, SD=3.1) were all significant. In addition, onset of alcohol use occurred significantly earlier than onset of marijuana and other street drug use as well as the onset of alcohol dependence. First use of tobacco occurred significantly earlier than the onset of alcohol dependence and other street drug use. Finally, the first use of marijuana occurred significantly earlier than the onset of other street drug use (
Figure 1).
Discussion
There are several strengths to this study. First, it examined a large number of alcohol-dependent adolescents, drawn from multiple sites. Second, highly trained research assistants carefully interviewed both the adolescent and his or her parents with semistructured assessment instruments. Finally, disruptive disorder diagnoses were made in the manner used by most child psychiatry epidemiological studies in that data were combined from child and parent interviews.
This study is unique in that it examined the onset of various disruptive behavior disorders in alcohol-dependent children while simultaneously investigating first use of other substances. Most other investigations have studied adults with alcohol dependence and retrospectively established the presence of childhood disruptive behavior disorders. The co-occurrence of a disruptive behavior disorder and alcohol dependence is not surprising. DSM-III-R suggested that among children with a diagnosis of conduct disorder, “regular use of tobacco, liquor, or nonprescribed drugs…that begins unusually early” is common and that the disorder is more common in children of adults with antisocial personality disorder and alcohol dependence.
In addition to supporting the hypothesis that conduct disorder is associated with adolescent alcohol dependence, the data here support the hypothesis of Kandel
(15) of a progressive nature to substance use; alcohol use typically occurs first, followed by use of cigarettes, marijuana, and other illicit drugs. The data also support Werch and Anzalone
(16) in suggesting that the vast majority of adolescents with alcohol dependence also use cigarettes, with no difference in the age at first use of either.
There are several limitations to this study. The first is that it is retrospective in nature and relies on the historical report of symptoms and their ages at onset as recalled by the adolescents and their parents. However, the research assistants were carefully trained both on how to ask the original question and to probe for further details. Furthermore, the data collected were less retrospective in nature than those of similar studies performed on adults with alcohol dependence.
A second limitation is that there was no independent verification of each adolescent’s alcohol-related symptoms. While this is true of most studies on adolescent alcohol use, the research assistants were trained to explore inconsistencies in the responses to the Child Semi-Structured Assessment for the Genetics of Alcoholism. If these inconsistencies were not resolved, a conservative approach was used: the interview item was scored as indeterminate and was not used to establish the diagnosis of alcohol dependence.
Third, the version of the semistructured interview used was based on DSM-III-R criteria, and the diagnosis of alcohol dependence may be less restrictive with this diagnostic scheme than with DSM-IV or ICD-10. DSM-III-R is biased in terms of the number of symptoms (a minimum of three out of nine) needed to fulfill criteria for the diagnosis of alcohol dependence. Actual impairment associated with these symptoms is vaguely defined with key descriptive terms being “often,” “a great deal,” “frequent,” and “important.” A fundamental aspect of the DSM-III-R criteria is the need for some symptoms to persist for at least 1 month. Training for the administration of the Child Semi-Structured Assessment for the Genetics of Alcoholism stressed that age at onset and duration be explored for all symptoms. To help delineate problematic drinking from a DSM-III-R diagnosis of alcohol dependence, this diagnosis was only used if, at a minimum, three criterion items were present at the same time and that all three were present during the same 1-month minimal period.
A fourth limitation is that the study may be biased because of the study group used. Seventy percent of the adolescents in this study came from families that contained multiple adults with a diagnosis of alcohol dependence. The remaining 30% came from nonselected community families. Outside of a more common family history of alcohol dependence in the high-risk families, the comparison families did not differ significantly in the variables examined in this study. However, it is important to remember that one-third of the community families also contained at least one alcohol-dependent parent, and the exact effect of parental alcohol dependence on the variables studied is unknown.
Despite these caveats, the study provides information that suggests a common developmental progression, in at least some adolescents, from conduct disorder to use of alcohol, tobacco, marijuana, and finally severe alcohol-related problems as defined by the diagnosis of alcohol dependence. However, the study cannot establish a causative role to any single symptom or cluster of symptoms (i.e., diagnosis). For example, impulsive behavior is common to both ADHD and conduct disorder, and it may also be associated with a wide variety of life stressors (e.g., poor relationships or poor academic performance) as well as difficulties with alcohol use. Therefore, impulsive behavior by itself may be a primary cause of alcohol dependence or a partial cause of alcohol dependence. Alternatively, impulsive behavior and alcohol dependence may be associated, but not causally related, because of other variables. Furthermore, the etiology of impulsive behavior, which is not clarified by this study, may reflect genetic transmission, early parental influences, or the combination of both. An actual answer to why some of these children develop substance use disorders while others do not will require a large number of children with specific disruptive behavior disorders to determine naturalistic as well as treatment-influenced outcome.
Acknowledgments
Collection, analysis, or storage of data for the Collaborative Study on the Genetics of Alcoholism (H. Begleiter, principal investigator; T. Reich, co-principal investigator) was conducted at nine centers by the following investigators: T.-K. Li, J. Nurnberger, Jr., P.M. Conneally, and H. Edenberg (Indiana University, Bloomington); R. Crowe and S. Kuperman (University of Iowa, Iowa City); M. Schuckit (University of California—San Diego, La Jolla); V. Hesselbrock (University of Connecticut, Storrs); B. Porjesz and H. Begleiter (State University of New York Health Sciences Center at Brooklyn); T. Reich, C.R. Cloninger, J. Rice, and A. Goate (Washington University, St. Louis); R. Taylor (Howard University, Washington, D.C.); J. Tischfield (Rutgers University, New Brunswick, N.J.); L. Almasy (Southwest Foundation for Biomedical Research, San Antonio, Tex.).