Epidemiological
(1) and clinical
(2) studies have demonstrated high comorbidity between posttraumatic stress disorder (PTSD) and psychotic symptoms. Despite this fact, there have been few studies of the etiology of this enigmatic disorder. This is because PTSD with psychosis is very heterogeneous; it may include patients with a primary psychotic disorder, or it may include patients with primary PTSD. We defined a homogeneous psychotic PTSD subtype consisting of patients with primary PTSD and secondary psychotic symptoms in which the onset of PTSD precedes the onset of psychosis. Because family history studies have revealed higher rates of depression and anxiety in relatives of PTSD probands
(3) and higher rates of psychosis in relatives of psychotic probands
(4), family data may be used to determine whether PTSD with secondary psychotic symptoms is more closely related to PTSD or to the psychotic disorders. The current study was intended to answer this question and to replicate earlier studies showing that PTSD is associated with familial depression.
Method
All PTSD veterans were recruited from PTSD treatment programs, and matched healthy comparison subjects were recruited from the housekeeping staff at New Orleans VA Medical Center. Written informed consent was obtained from the subjects after the study procedures had been explained to them. Probands were assigned to one of three groups on the basis of their score on the Structured Clinical Interview for DSM-IV (SCID): 1) DSM-IV PTSD with secondary psychotic symptoms (N=23), 2) DSM-IV PTSD without psychotic symptoms (N=16), or 3) healthy comparison subjects (N=15). Probands with PTSD with secondary psychotic symptoms were included only if the PTSD diagnosis preceded the onset of psychosis. Fourteen probands with PTSD with secondary psychotic symptoms met criteria for schizoaffective disorder, and four met criteria for major depression with psychotic features. Comparison subjects were excluded from the study if they showed symptoms of psychosis or PTSD. All subjects were excluded if they had current substance abuse, organic mental disorder, or mental retardation.
Information about each proband’s first-degree relatives was obtained through an interview with the proband with use of the Family Interview for Genetic Studies
(5) and by directly interviewing at least one first-degree relative from each family with the SCID. A second SCID interview was conducted in 13 (24.1%) of 54 families. Nonparticipation among relatives was due to lack of subject availability and was not related to psychiatric status. DSM-IV diagnoses of relatives were established by a blinded expert diagnostician (J.J.J.) using best-estimate methods.
Results
A total of 257 (90.5%) of the 284 first-degree relatives of the probands were diagnosed as part of the study. The remaining 9.5% could not be assigned a diagnosis because of a lack of diagnostic information. The three groups of relatives did not differ in terms of mean age or gender.
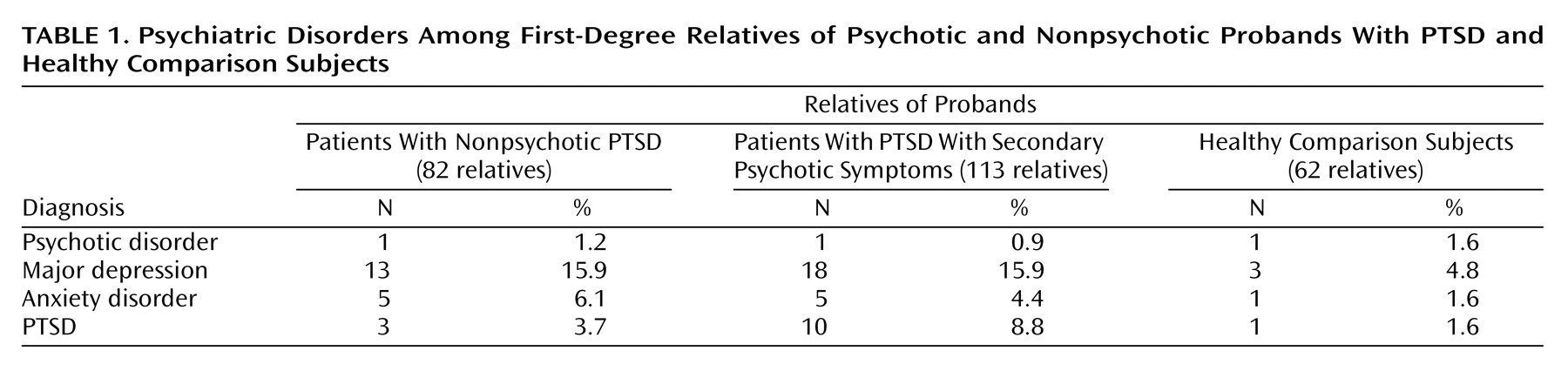
Table 1 shows the number of relatives in each of the three groups (nonpsychotic PTSD, PTSD with secondary psychotic symptoms, healthy comparison) that met criteria for major depression, anxiety disorder, psychotic disorder, or PTSD.
The first hypothesis stated that the relatives of the probands with PTSD (PTSD with secondary psychotic symptoms or nonpsychotic PTSD) would show higher rates of mental disorder than the relatives of the healthy comparison subjects. Psychiatric disorder in the relatives varied significantly depending on the presence of PTSD in the proband (χ2=7.16, df=2, N=257, p=0.03).
The second hypothesis stated that the relatives of probands with either psychotic or nonpsychotic PTSD would show levels of familial depression and PTSD that would exceed that shown by the relatives of the healthy comparison subjects. Depression was more likely to occur in the PTSD families (N=31, 15.9%) than in the healthy comparison families (N=3, 4.8%) (p=0.01, Fisher exact test). Anxiety (p=0.21, Fisher exact test), psychosis (p=0.57, Fisher exact test), and PTSD (p=0.11, Fisher exact test) were not diagnosed at a higher rate in the relatives of PTSD probands (N=10, 5.1%; N=2, 1.0%; N=13, 6.7%; respectively) than in the relatives of the healthy comparison probands (N=1, 1.6%; N=1, 1.6%; N=1, 1.6%; respectively).
In the third set of analyses, we compared the rates of major depression and psychotic disorder in the relatives of the probands with PTSD with secondary psychotic symptoms and the relatives of the healthy comparison probands. These analyses showed that the relatives of probands with PTSD with secondary psychotic symptoms showed higher levels of familial depression (p=0.02, Fisher exact test) than the relatives of the comparison probands and that the relatives of the psychotic PTSD probands showed levels of psychotic disorder that did not differ from that shown by the relatives of the comparison subjects (p=0.64, Fisher exact test).
The fourth set of analyses used the Fisher exact test to compare the number of families from each proband group that contained at least one psychiatric disorder for each of the four disorders being evaluated in this study. This allowed us to ascertain whether the previous results were influenced by a few families with a large number of affected family members. The results revealed that depression was more likely to occur in the PTSD families than in the comparison families (p=0.02, Fisher exact test) and the other disorders were distributed equally among the three groups.
Discussion
The findings from this study provide strong support for previous family studies of PTSD that have shown a strong familial relationship between PTSD and major depression
(3). Our data clearly show that the relatives of probands with PTSD show higher levels of familial depression than the relatives of healthy comparison subjects. PTSD was not associated with familial anxiety.
These findings also show that the psychosis that occurs in PTSD with secondary psychotic symptoms is familially different from schizophrenic symptoms; PTSD with secondary psychotic symptoms was not associated with the higher rates of familial psychosis that are normally associated with schizophrenia. However, PTSD with secondary psychotic symptoms was associated with the family history of depression that is normally associated with PTSD
(3). These data suggest familial similarity between PTSD and PTSD with secondary psychotic symptoms.
Because of the small size of this preliminary study, these results should be conservatively interpreted. A few families with a large number of affected relatives could have exerted a strong influence on the study findings. We accounted for this possibility by comparing the numbers of families with at least one affected relative for each of the diagnoses included in this study. These analyses yielded a similar pattern of results, indicating that the results of our other analyses are not likely to be due to the overrepresentation of families with a large number of affected family members. The finding that relatives of probands with PTSD with secondary psychotic symptoms show a paucity of familial psychosis could also be influenced by the small size of this study group. The results of this study must be replicated with a larger group.
This study indicates that PTSD with secondary psychotic symptoms is a PTSD subtype that is familially distinct from the psychotic disorders but is associated with a family history of depression. This suggests that chronic psychosis may occur independently of a genetic vulnerability to psychosis and may be associated with traumatic stress. This extends previous findings that psychotic symptoms are affected by stress
(6). More research needs to be conducted in this important but understudied area.