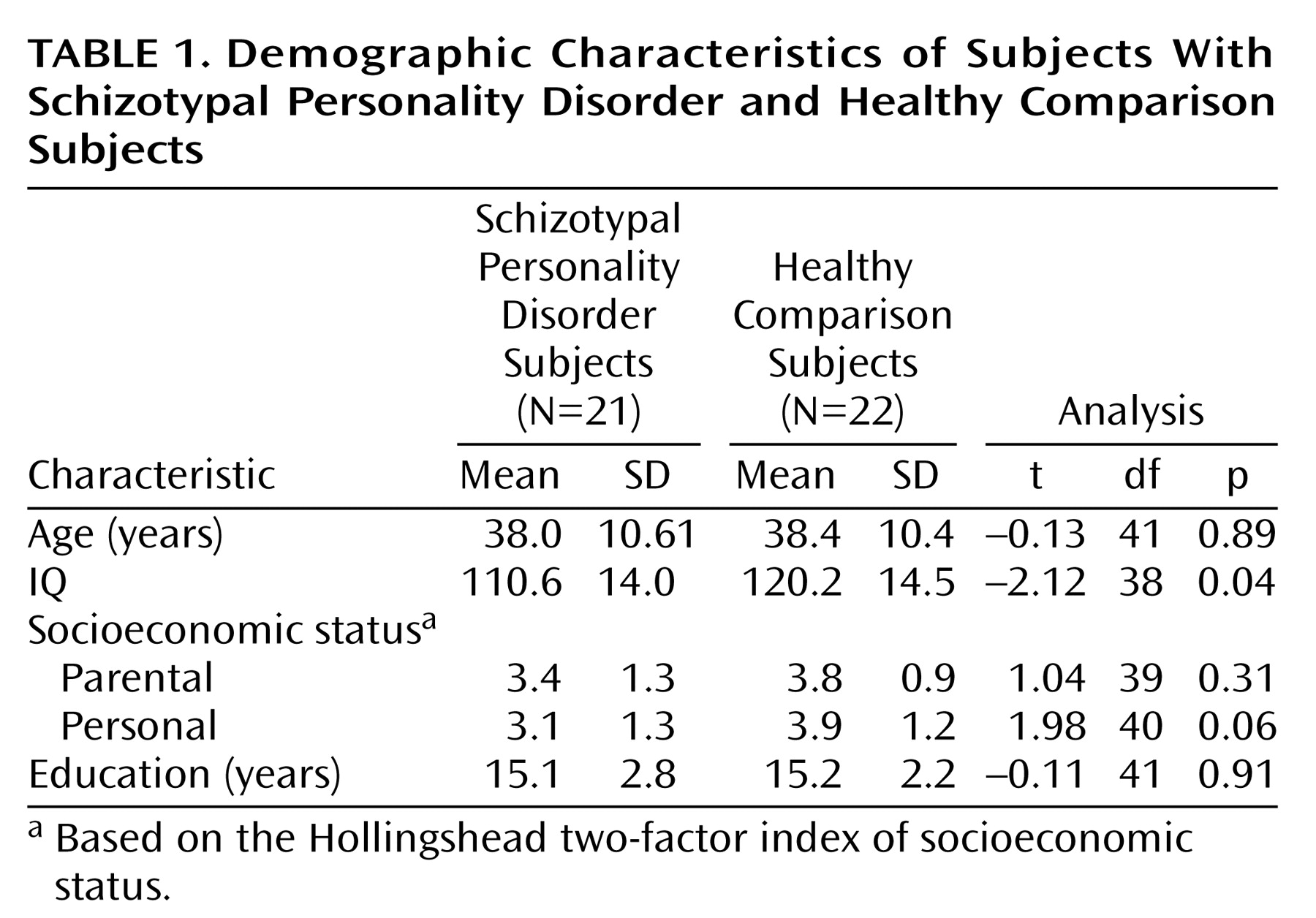
Schizotypal personality disorder is considered part of the schizophrenia spectrum
(1) because it shares a common genetic diathesis with schizophrenia
(2–
4) and because individuals diagnosed with schizotypal personality disorder evince many of the biological features that are observed in schizophrenia, albeit in milder form. These include higher homovanillic acid levels, aberrant eye tracking, cognitive deficits, and electrophysiological abnormalities
(5–
12). Of note, however, persons with schizotypal personality disorder are not psychotic and generally have not been prescribed neuroleptic medications. Thus, schizotypal personality disorder affords researchers a unique opportunity to study the schizophrenia spectrum without the potential confounding factors of neuroleptic usage, repeated hospitalizations, and chronicity.
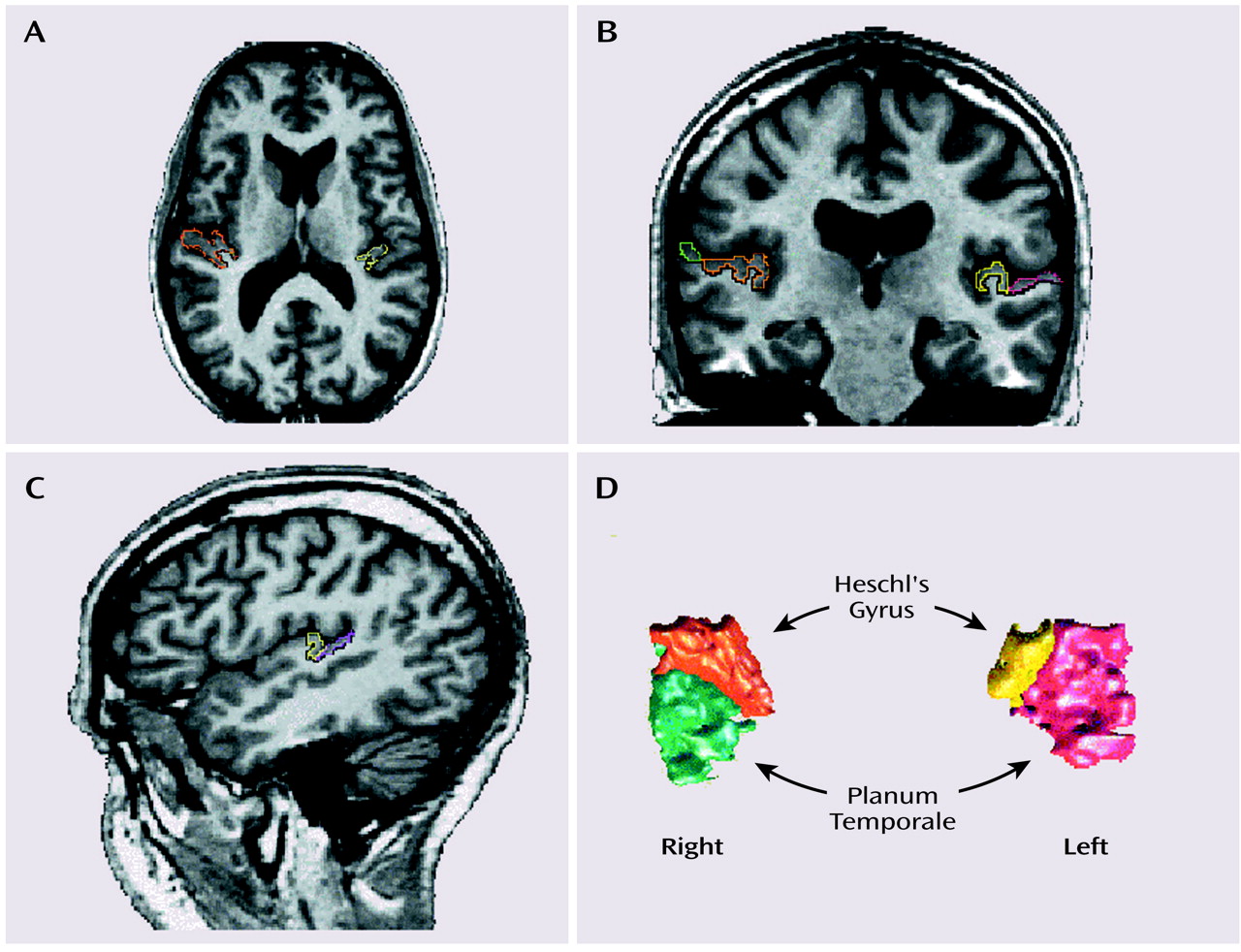
Our laboratory’s work has focused mainly on the temporal lobe, in particular the gray matter of the superior temporal gyrus. The superior plane of the superior temporal gyrus consists of three regions (moving posteriorly): the temporal pole (which has sensory-limbic integrative functions
[19]), Heschl’s gyrus (responsible for processing of pure tones), and the planum temporale (which may be involved in phonemic processing). Of note, gray matter abnormalities in the superior temporal gyrus are the most robust finding in schizophrenia (all 12 of the studies examining gray matter have found abnormalities
[20]). In our initial investigation of the temporal lobe in subjects with schizotypal personality disorder, we found the gray matter volume of the left superior temporal gyrus to be smaller and also found a higher rate of thought disorder in the subjects with schizotypal personality disorder
(21). This finding was similar to what our laboratory
(22) and other laboratories have shown in schizophrenia
(23–
25) (for review, see references
20,
26).
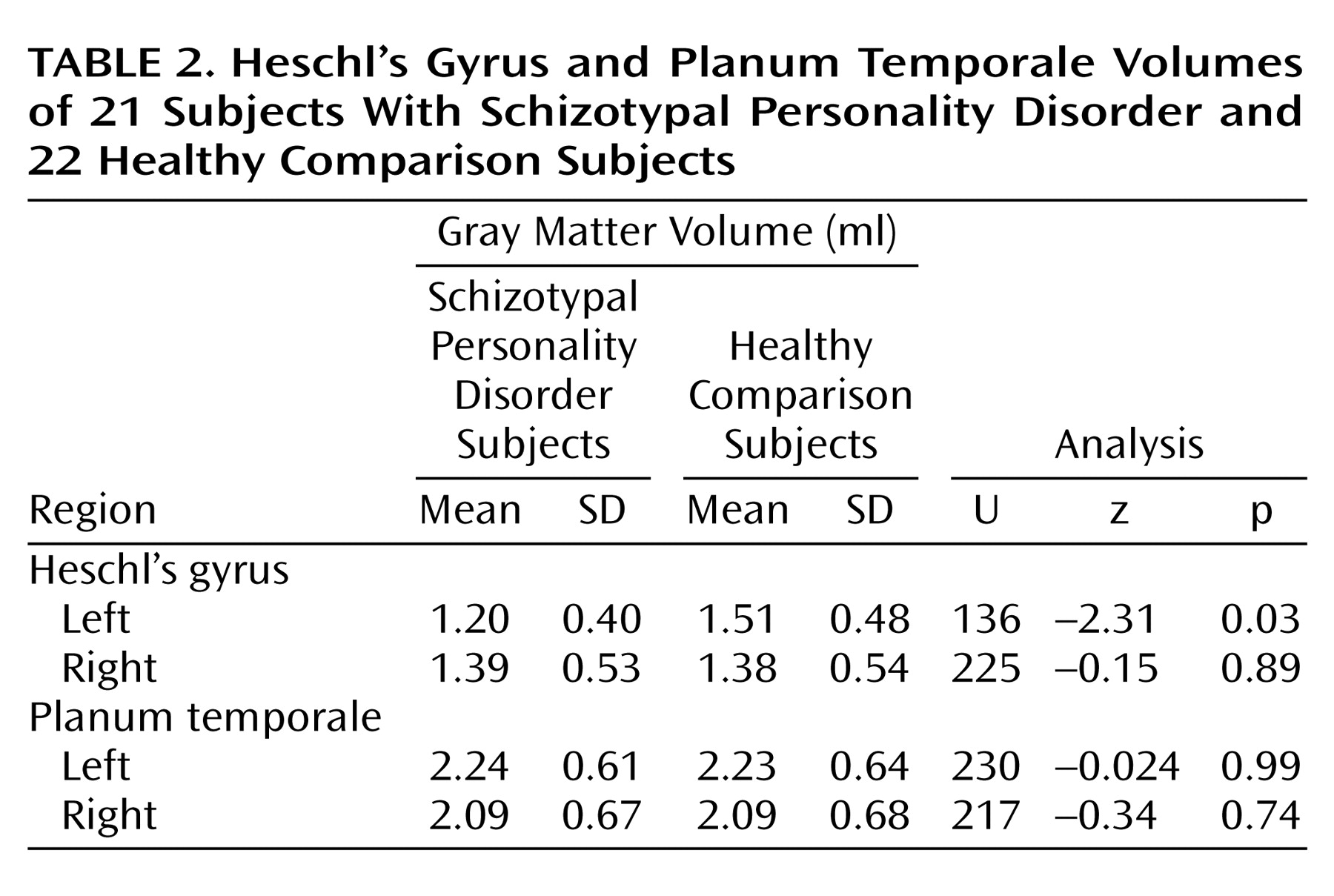
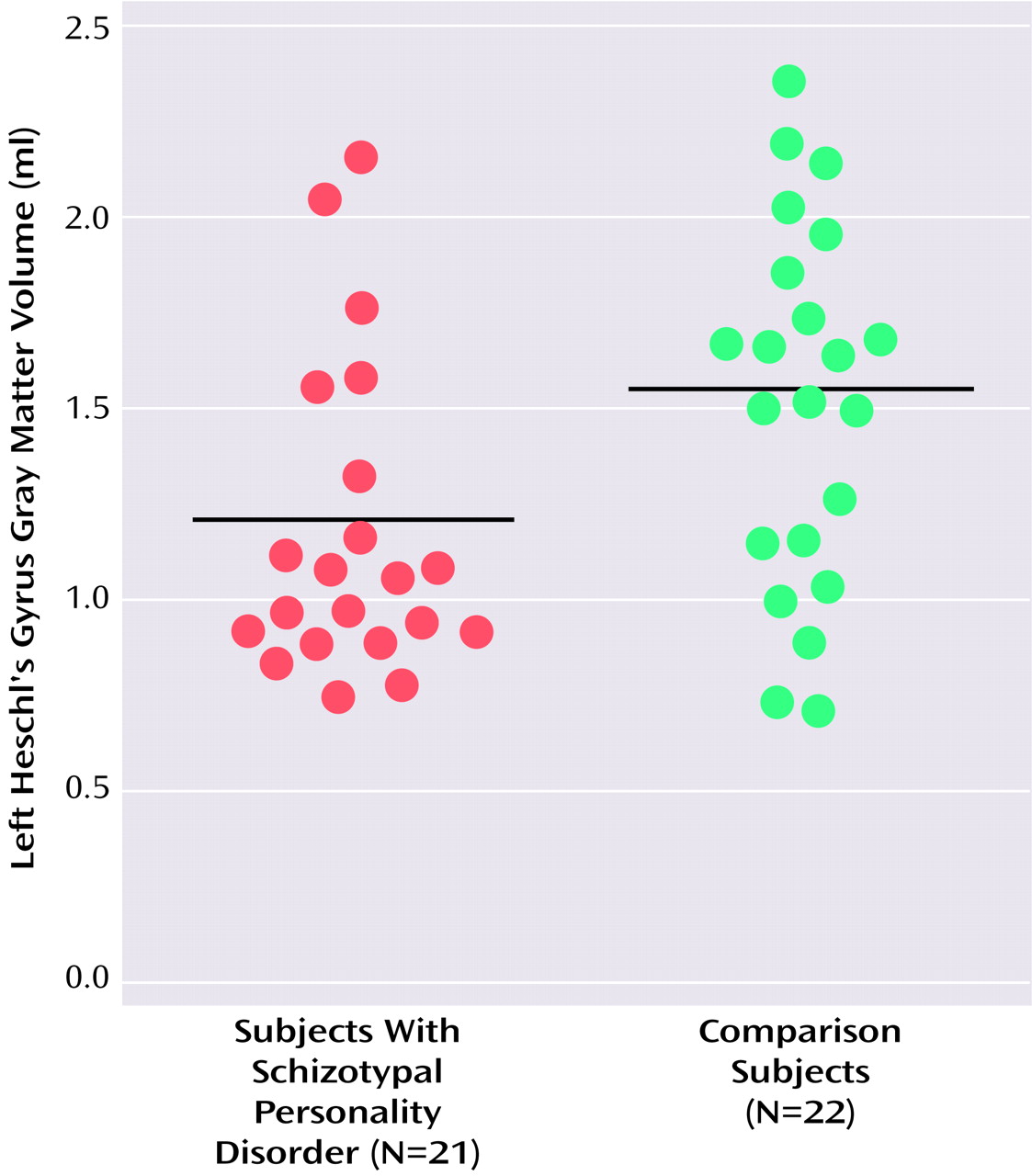
Discussion
We found smaller left Heschl’s gyrus gray matter volume in right-handed male subjects with schizotypal personality disorder relative to that of comparison subjects. To our knowledge, no other study has examined this structure in subjects with schizotypal personality disorder. This finding was a further refinement of our previous report of smaller gray matter volume in the left superior temporal gyrus
(21).
In the comparison subjects there was a positive correlation between Heschl’s gyrus and planum temporale gray matter volume not found in the schizotypal personality disorder subjects. This lack of correlation was likely due to the 21% smaller left Heschl’s gray matter volume and the normal planum temporale volumes in the schizotypal personality disorder subjects rather than due to a difference in the variability of the data between the two groups. This reinforces the notion that the abnormality in subjects with schizotypal personality disorder is restricted to left Heschl’s gyrus.
This result is similar to our previous finding of smaller volumes of Heschl’s gyri (total volume) and left planum temporale in patients with first-episode schizophrenia
(27). In chronic schizophrenia patients it was the left planum temporale, not left Heschl’s gyrus, that was smaller
(28). The discrepancy between superior temporal gyrus findings is most likely due to subject or other methodological differences. For example, although schizotypal personality disorder and comparison subjects within this study had comparable education levels, the schizotypal personality disorder subjects had a lower IQ than did their counterparts. It may be that the disease or genetic liability of schizotypal personality disorder affects some measures of IQ. In a study of schizophrenic relatives, for example, Faraone et al.
(34) noted deficits in the realms of abstraction, verbal memory, and auditory attention that were not attributable to educational level attained or parental socioeconomic status. It may be that subjects with schizotypal personality disorder have similar genetic loci affecting scores on neuropsychological measures as do the relatives
(34). In addition, this report used fairly functional subjects recruited from the community, not patients, whereas a similar study of clinic-based schizotypal personality disorder subjects may demonstrate more extensive abnormalities. Therefore, how groups are matched may play a role in subtle differences in volume findings. The other factor that may account for the slightly diverging reports may be minimal differences in methodology. For example, in the present study, images were realigned, reformatted, and the anterior/posterior boundaries were extended compared with Kwon et al.
(28). Also, despite good interrater reliability, different people were manually drawing the region of interest. Finally, in patients with chronic schizophrenia it is possible that with neuroleptic usage, the volume of the superior temporal gyrus may change over time
(35) and that those effects would not be seen in these neuroleptic-naive schizotypal personality disorder subjects. Nonetheless, this report employed the same methodology as did Hirayasu et al.
(27), thus strengthening the interpretation of finding a more constricted abnormality in schizotypal personality disorder than in schizophrenia (smaller left gray matter volume in left Heschl’s gyrus alone as contrasted with smaller volumes in both Heschl’s gyri and left planum).
The finding of smaller left Heschl’s gyrus gray matter volume in subjects with schizotypal personality disorder was a further specification of our previous finding of smaller left superior temporal gyrus volume and may have more precisely indicated a key area of abnormality in the schizophrenia spectrum. This may suggest that the less affected planum temporale may attenuate the language abnormalities seen in patients with schizophrenia. For example, schizotypal personality disorder subjects have thought disorder as measured by the Thought Disorder Index, but it was less severe than what has been shown in patients with schizophrenia
(21).
The superior temporal gyrus consists of three components (anterior to posterior): the temporal pole, Heschl’s gyrus, and planum temporale. Receptive auditory processing is now considered to be hierarchical—not unlike the visual system—with highly specialized Heschl’s gyrus (primary auditory cortex) at the core and a surrounding belt region in the auditory cortex of the superior temporal plane with more integrative functions
(36,
37). Heschl’s gyrus receives auditory sensory inputs via the thalamic medial geniculate nucleus and provides preattentive processing of pure tones
(38,
39) in posterior and medial portions, while more extensive regions of this gyrus respond to band-passed noise
(37).
In functional MRI (fMRI) studies, voice-selective regions have been located ventral to the belt region in the upper bank of the superior temporal sulcus, an area that receives direct inputs from the more dorsal surface of the superior temporal gyrus
(36,
40) and is possibly analogous to the face recognition areas in the fusiform gyrus
(41). The next stage of language processing, phonemic processing, which may be viewed as a fusing of multiple sound features, has been reported to occur in the auditory association cortex located in the superior temporal sulcus
(40), although other reports place phonemic processing in the planum temporale and Wernicke’s area
(32,
42), including the angular and supramarginal gyrus of the parietal lobe
(43)—regions also found to be abnormal in schizophrenia
(44–
46).
The highest level of processing, that of semantic features, is the most highly left-lateralized and is thought to occur inferior to the superior temporal gyrus in the middle and inferior temporal gyri and in the temporal pole—areas less thoroughly explored in schizophrenia
(40). Semantic processing also extends posteriorly to the angular gyrus
(40).
Recent work has suggested a dual processing stream for auditory percepts
(47), not unlike the dorsal and ventral pathways of the visual system. From the auditory core, located in A1 or Heschl’s gyrus, two parallel streams emerge: a ventral one dedicated to processing auditory patterns (“what”) located on the lateral belt of the superior temporal cortex, and a second dorsal pathway specific for processing spatial information of auditory inputs (“where”) that extends into the parietal region
(39). According to this model, both streams converge with visual information in the prefrontal cortex in order to provide multimodal, integrative processing that can in turn be linked with the ability to abstract
(39).
How these downstream language processes may be affected by an abnormality in the superior temporal gyrus or, more specifically, in Heschl’s gyrus is still uncertain. Moreover, the effect of pathology, such as that occurring in schizophrenia or schizotypal personality disorder, on the functional anatomy of these key language processing areas is just beginning to be explored. For example, using fMRI, Wible et al.
(48) showed in schizophrenic subjects abnormal Heschl’s and posterior superior temporal gyrus activation to “mismatched” or unattended discordant tones, an example of an early perceptual processing abnormality in patients known to have abnormalities of language production. An increase in fMRI activation in Heschl’s gyrus during auditory hallucinations has also been reported
(49) (although it has been suggested that the result might have been due to a shift of auditory attention as opposed to the hallucinations themselves
[50]). Other data suggest that the superior temporal gyrus may be involved in the production of hallucinations
(51,
52), and smaller superior temporal gyrus volume has been associated with both the severity of hallucinations
(23,
53) and greater thought disorder
(22,
25).
Our laboratory has previously shown that schizotypal personality disorder subjects, relative to comparison subjects, have language deficits
(11,
12), thought disorder
(21), verbal memory impairments
(11), and, using event-related potentials, N400 abnormalities while processing normal sentences
(54). In the present group of schizotypal personality disorder subjects, there was no correlation between any region of interest and thought disorder, as measured by total score on the Thought Disorder Index, or verbal learning, as measured by the California Verbal Learning Test. There was, however, a correlation between delayed recall, as measured by the Wechsler Memory Scale—Revised, and left Heschl’s gyrus volume that requires further study.
A potential limitation of this study was the inclusion of schizotypal personality disorder subjects with histories of nonpsychotic comorbid disorders. However, one would predict that inclusion would have diluted the results. For example, it may be that left planum temporale gray matter would have been similarly reduced, not unlike what was shown in patients with first-episode schizophrenia
(27), had there not been comorbidity. Much remains to be learned about the seemingly high prevalence of comorbidity in this population (approximately one-half had axis I disorders and three-quarters had other personality disorders) and its impact on fundamental neuroanatomy.
The main finding of this study was the localization of deficits in the left superior temporal gyrus to Heschl’s gyrus, primary auditory cortex. This region operates early in the auditory processing stream and is important for processing of tones
(37,
39,
40). Whether this volume deficit is directly associated with primary auditory processing problems and, downstream, contributes to language comprehension problems is not yet known. However, evidence of early processing problems in schizophrenia, such as mismatch abnormalities (structurally localized in or near Heschl’s gyrus), suggests that a focus on both structural and functional features associated with early auditory processing in schizotypal personality disorder may be a promising avenue of investigation.