Despite the overall decline in the incidence of violent behavior during the past decade, youth violence remains a significant societal concern. The widely publicized violent outbursts by youth in schools and other public settings in recent years have piqued national interest concerning the causes and prevention of adolescent violence. The large-scale infusion of funds by the federal government to support research under the aegis of the Centers for Disease Control and Prevention, National Institutes of Health, and Department of Education underscores recognition of this public health problem.
A daunting challenge pertains to identifying youth who are at high risk for violent behavior, especially considering the large number and complexity of predisposing factors and manifold variations. For example, twin studies directed at elucidating the genetic contribution to variation in physical aggression have yielded heritability estimates as high as 0.58 in adults
(1) and 0.32 in adolescents
(2). In this latter study, aggression was defined as interpersonal violence involving 1) physical fighting that caused serious injury to another person, 2) use of or threat of using weapons, or 3) participation in gang fights. Gross morphological disturbances in the brain, particularly the prefrontal cortex, have been reported in homicidal adults
(3). Neuroanatomical studies have not yet been conducted on youth; however, it should be noted that youth at high risk for violence have low executive cognitive capacity
(4). This multidimensional capacity—encompassing abstracting, problem solving, working memory, and attentional control—is consensually recognized to be subserved by the prefrontal cortex and subcortical connections
(5). Biochemical mechanisms that have been implicated to predispose to violence include low serotonin level
(6), low cortisol reactivity
(7), and high testosterone level
(8).
A variety of psychosocial factors have also been implicated as associated with a heightened risk for adolescent violence. These factors include a deficiency in social skills required for resolving incipient violent encounters
(9), the belief that it is acceptable to behave violently
(10), incapacity to manage feelings of anger
(11), misinterpretation of the intentions of others
(12), hopelessness about the future
(13), and low self-esteem
(14). Unsurprising is the fact that violence potential (e.g., carrying a weapon) and its overt expression (e.g., using a knife to injure someone) are related to an aggressive dispositional style
(10).
The opportunity for violence is also strongly contingent on social contextual factors. As youth disengage from parental supervision, the friendship network exerts an increasingly powerful influence on behavior. Adolescents who are delinquent and aggressive affiliate with peers who are similarly aggressive and delinquent
(15). Notably, members of socially nonnormative peer groups become more similar in attitudes and behavior over time
(16). As stated by Harris, “In-group favoritism and out-group hostility widen differences between groups or create differences if there were none to begin with”
(16, p. 467). Thus, children with dispositional aggressive tendencies may experience a significantly higher likelihood of engaging in violence if their peer group is characterized by delinquency or externalizing behavior. A strong association between a socially nonnormative friendship group and violent behavior has been documented
(17).
One of the strongest correlates of violent behavior in youth is substance use
(18). Even among nonviolent youth, the rate of psychoactive drug use is high. For example, the results of the 2000 national survey “Monitoring the Future”
(19) indicated 30-day prevalence rates for alcohol, cannabis, and amphetamine use of 22.5%, 10.2%, and 2.6%, respectively, among boys in the eighth grade. Of significance is the fact that high school students who use alcohol and illicit drugs have been reported to be over three times more likely than nonusers to engage in physical fights and are twice as likely to bring a weapon to school
(20).
Managing the child’s transition from childhood through adolescence to adulthood requires effective adult oversight, particularly ongoing awareness of the child’s friendship network. Parents who are either unable or not motivated to provide supervision of their child’s friendships during the transition from childhood to adolescence, either because of psychiatric illness or impairment from a substance use disorder, provide opportunities for their children to be exposed to high-risk social situations. Parental substance use disorder and psychiatric illness are commonly associated with an aversive and stressful home environment that, combined with parental dysfunction, promotes the child’s disengagement from the family. Furthermore, it is noteworthy that children of parents with substance use disorder more frequently manifest difficult temperament, externalizing disorders, and aggressivity
(21). Young children with these psychological features require more parenting resources and more intense parental involvement. These resources may not be available if a parent has a substance use disorder or another psychiatric disorder, thereby augmenting the child’s risk for violence outcome.
The purpose of this study was to determine the extent to which childhood characteristics (psychiatric history, substance use behavior) and parental characteristics (substance use and psychiatric disorder), in conjunction with the score on a newly derived instrument that encompasses the key social contextual factors of peer and school adjustment (the Violence Proneness Scale), predict violent behavior in young adulthood. The utility of these factors to identify youth who subsequently will exhibit violent behavior may provide an empirically substantiated basis for efficient population screening for violence prevention.
Method
Subjects
Probands were drawn from a pool of adult men (N=121) who either qualified for a lifetime DSM-III-R diagnosis of substance use disorder or had no substance use disorder or any adult axis I or II psychiatric disorder. Psychiatric comorbidity in the probands with substance use disorder was not an exclusionary factor, since this is highly common. The probands with no substance use disorder also had no adult psychiatric disorder so that the children would not be exposed to current paternal psychopathology.
Biological male offspring of the probands were first evaluated when the children were 12–14 years old; they were subsequently tracked to the age of 19 for follow-up evaluation. These boys have been involved in a long-term prospective investigation that began when they were 10–12 years old. However, because alcohol and drug use is infrequent in 10–12-year-old children, this study was conducted when they attained 12–14 years of age, at which time the rate of alcohol and drug use is sufficiently high to enable valid statistical analysis. Only one male child in each family was studied to avoid biased results inasmuch as children comprising a sibship are not independent subjects. The study was confined to boys because their higher rate of violence enabled the detection of predictors in this group of limited size.
Fifteen (12%) of the offspring were lost to follow-up after the baseline evaluation at ages 12–14, thereby reducing the study group size from 121 to 106. Comparisons between the dropouts and remaining subjects did not reveal significant differences in IQ or family socioeconomic status. In addition, the rate of lifetime psychiatric disturbance was similar between the dropouts and remaining subjects for the following diagnostic categories: attention deficit hyperactivity disorder (ADHD), conduct disorder, oppositional defiant disorder, anxiety disorder, and depression. There was no difference in attrition rate between the offspring of probands with and without substance use disorder (14.6% [N=7 of 48] and 11.0% [N=8 of 73], respectively; χ2=0.41, df=1, p=0.52). An additional seven families were excluded because of incomplete data. Thus, the study group was further reduced from 106 subjects to the final study group size of 99 subjects. The longitudinal analyses directed at predicting violence between ages 12–14 and 19 were conducted in this group of 38 boys whose fathers had a substance use disorder and 61 boys whose fathers had no adult psychopathology.
Multiple recruitment sources were used to minimize bias that could potentially occur if all of the probands were recruited from one source. Approximately 20% of the substance use disorder probands were derived from treatment facilities, whereas the remainder were recruited from the community through public service announcements and advertisements as well as by direct telephone contact conducted by a market research firm. The inclusion of men with substance use disorder who recently completed treatment or were in aftercare was based on the rationale that their disorder may be more severe than that of men not in treatment. Hence, combining treatment and nontreatment substance use disorder probands encompasses a broad spectrum of substance use disorder severity. Psychosis, mental retardation, and neurological injury or disease were exclusionary criteria for participation of the family. Recruitment of probands with no adult psychopathology was conducted through advertisements, public service announcements, and the same market research firm used to locate the substance use disorder probands.
Procedure
After complete description of the study to the subjects, written informed consent was obtained. Parents provided informed consent for their minor children (age 12–14). The boys provided informed consent at the age 19 follow-up evaluation. Each family member was individually administered the research protocol in a private room by a different clinical associate who was not given any information about the subject’s medical, psychiatric, and legal history. The diagnostic interviews were conducted by a staff of four experienced clinical associates. Training the clinical associates involved observation of several interviews and conducting joint interviews in the presence of an experienced interviewer.
Each biological parent was administered the Structured Clinical Interview for DSM-III-R (SCID)
(22) to document lifetime abuse/dependence for all categories of compounds that have such liability. The interview was administered by master’s-level clinical associates. The clinical associates underwent extensive training, including ongoing oversight by a board-certified psychiatrist. At the outset of this research program in 1989, the training procedures were found to produce interrater reliabilities exceeding 0.80 for all major diagnostic categories.
Diagnoses were formulated by using the best-estimate procedure
(23). The SCID results, in conjunction with all available pertinent medical records and social and legal history, were reviewed in a clinical case conference chaired by a board-certified psychiatrist and consisting of another psychiatrist or psychologist along with the clinical associate who conducted the interview. DSM-III-R criteria were applied to derive lifetime diagnoses, since this research was initiated before the advent of DSM-IV. The aforementioned procedures were also used to characterize lifetime psychopathology other than substance use disorder.
Alcohol, tobacco, and marijuana use frequency were documented in the offspring of the probands at age 12–14 by using section 1A of the Drug Use Screening Inventory
(24,
25). The past-month average frequency of consumption for these compounds was the score used to index level of drug involvement. Other drugs were not included because the rate of consumption at age 12–14 was too low to enable statistical analysis.
Offspring psychopathology was assessed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (K-SADS-E)
(26); both the child and a parent (typically the mother) served as informants. The aforementioned best-estimate procedure was used to formulate lifetime psychiatric disorders that were based on the results of both parent and child K-SADS-E reports in conjunction with available medical, legal, and social history information.
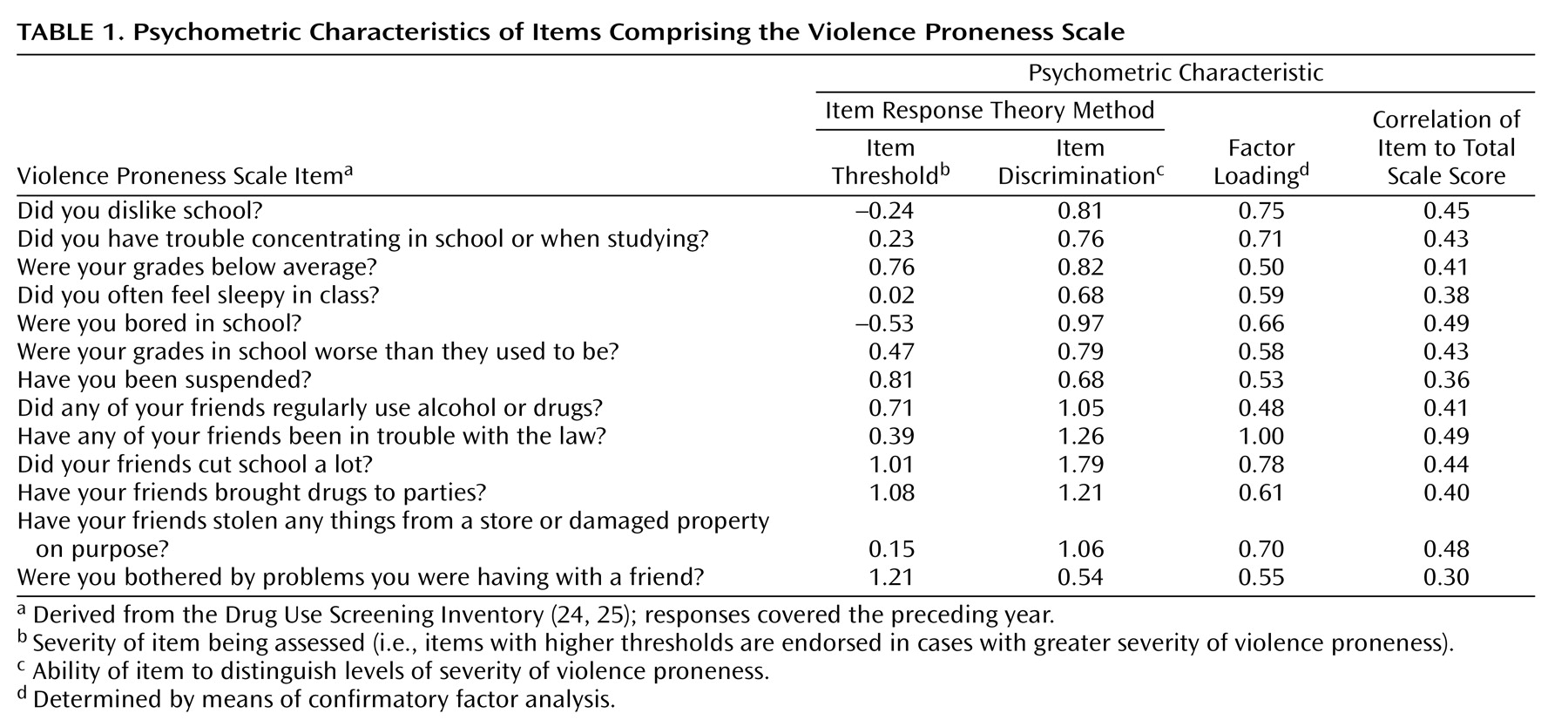
Violence Proneness Scale
A provisional scale to assess the offspring’s proneness to commit an act of violence was developed in a series of iterative analyses by using items from the revised Drug Use Screening Inventory. Scale construction and subsequent confirmation of its psychometric properties, consisting of six stages, were conducted within a group of 417 boys between 12–14 years of age. First, to narrow the relevant domains, the 10 domain scores of the Drug Use Screening Inventory were correlated with the total score on the Andrew Severity and History of Offenses Scale
(27). Only two scale scores, school adjustment (r=0.42, df=415, p<0.001) and peer relations (r=0.45, df=415, p<0.001), demonstrated significant association. Second, to identify the specific items in these two scales that potentially were most predictive of violence, each item was correlated with the Andrew Scale total score by using point biserial correlation. A total of 20 Drug Use Screening Inventory items significantly correlated with violence outcome at age 19. Items having a low correlation (r<0.25) were eliminated, which resulted in one of the items being deleted from the item pool. The third stage involved testing the unidimensionality of the remaining 19 items by using confirmatory factor analysis. This procedure resulted in deletion of one item that had a nonsignificant factor loading. In the fourth stage of scale development, item response theory methods
(28) were used to assess item quality by determining the item threshold and discrimination parameters of the remaining 18 items. Item threshold characterizes the severity of the property being assessed; that is, items having a higher threshold are endorsed in more severe cases. Item discrimination refers to the ability of an item to distinguish levels of severity on the trait, which in this study is violence proneness. Items having a discrimination of 0.40 or less were discarded. This analysis yielded a final set of 13 items with an average item discrimination of 0.96 (SD=0.33) and average item threshold of 0.47 (SD=0.53). These 13 items did not overlap with the items from section 1A of the Drug Use Screening Inventory used to document alcohol, tobacco, and marijuana use frequency. The unidimensionality of the Violence Proneness Scale was also established by using confirmatory factor analysis (χ
2=26.39, df=21, p<0.20; root mean square error of approximation=0.025; goodness-of-fit index=0.99; adjusted goodness-of-fit index=0.96; nonnormed fit index=0.99). Last, the psychometric properties of the Violence Proneness Scale were documented. The coefficient of internal consistency (Cronbach’s alpha=0.79) and the average correlation of item and total test score (r=0.42) indicate that the Violence Proneness Scale has satisfactory reliability. The items comprising the Violence Proneness Scale and their psychometric characteristics are presented in
Table 1.
The dependent variable, violent behavior, was assessed at age 19 with the Andrew Severity and History of Offenses Scale
(27). This scale was used because it focuses on discrete behaviors rather than traits such as aggressivity. From a set of 65 items ranked according to severity, 13 items pertain to violent behavior. Although the range of violent behaviors is diverse, the manifest consequence is the same: the potential for intentional physical injury of another person. The questionnaire was completed as a self-report and subsequently reviewed by the research associate for accuracy and completeness. Questions or uncertainties about the purpose of the questionnaire as well as any other issues were addressed by the research associate. Significantly, this questionnaire documents discrete events that have face validity for documenting type and severity of violent behaviors and not dispositional behavior, personality, or psychopathology.
Statistical Analysis
Because the data were binary, multivariate logistic regression analysis was conducted
(29). This analysis determined the odds ratio for prediction of presence or absence of violent outcomes between ages 12–14 and 19. The predictor variables were the Violence Proneness Scale score, presence/absence of parental substance use disorder (with the exception of nicotine), offspring’s frequency of past month substance use, and presence of psychiatric disorder in the offspring. IQ and socioeconomic status were controlled in computing the odds ratios.
Results
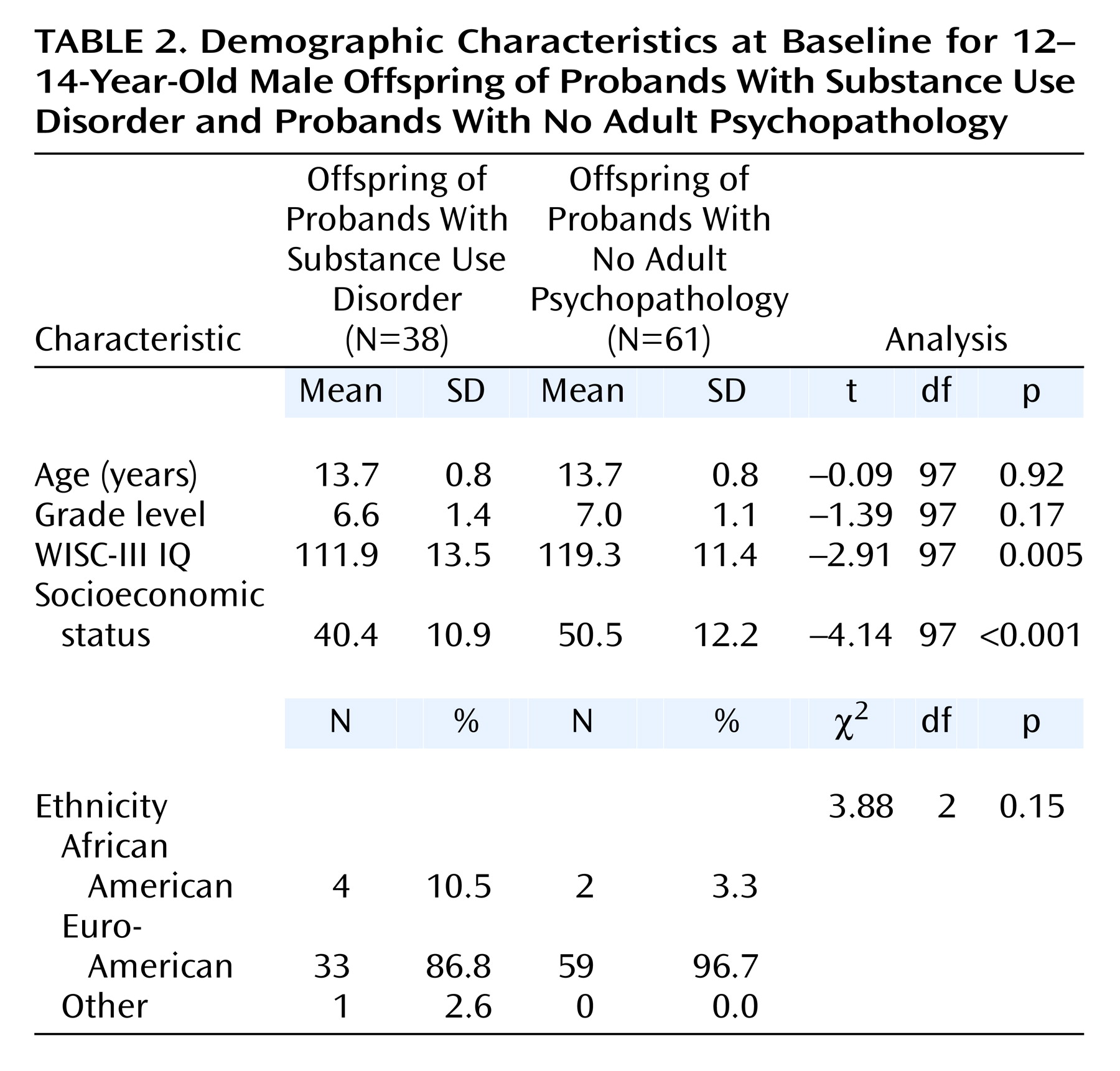
Table 2 summarizes the characteristics of the study group. Consistent with the downward social mobility that accompanies paternal substance use disorder, family socioeconomic status was significantly lower in the families of probands with substance use disorder than in the families of the psychiatrically normal probands. In addition, the children of probands with substance use disorder obtained lower WISC-III IQ scores; however, both groups scored in the normal range. Because socioeconomic status and IQ were lower in the children of probands with substance use disorder, these variables were controlled in the statistical analyses. Age and grade level did not differ between the offspring of the probands with substance use disorder and the offspring of probands with no adult psychopathology. The groups did not differ with respect to ethnicity distribution.
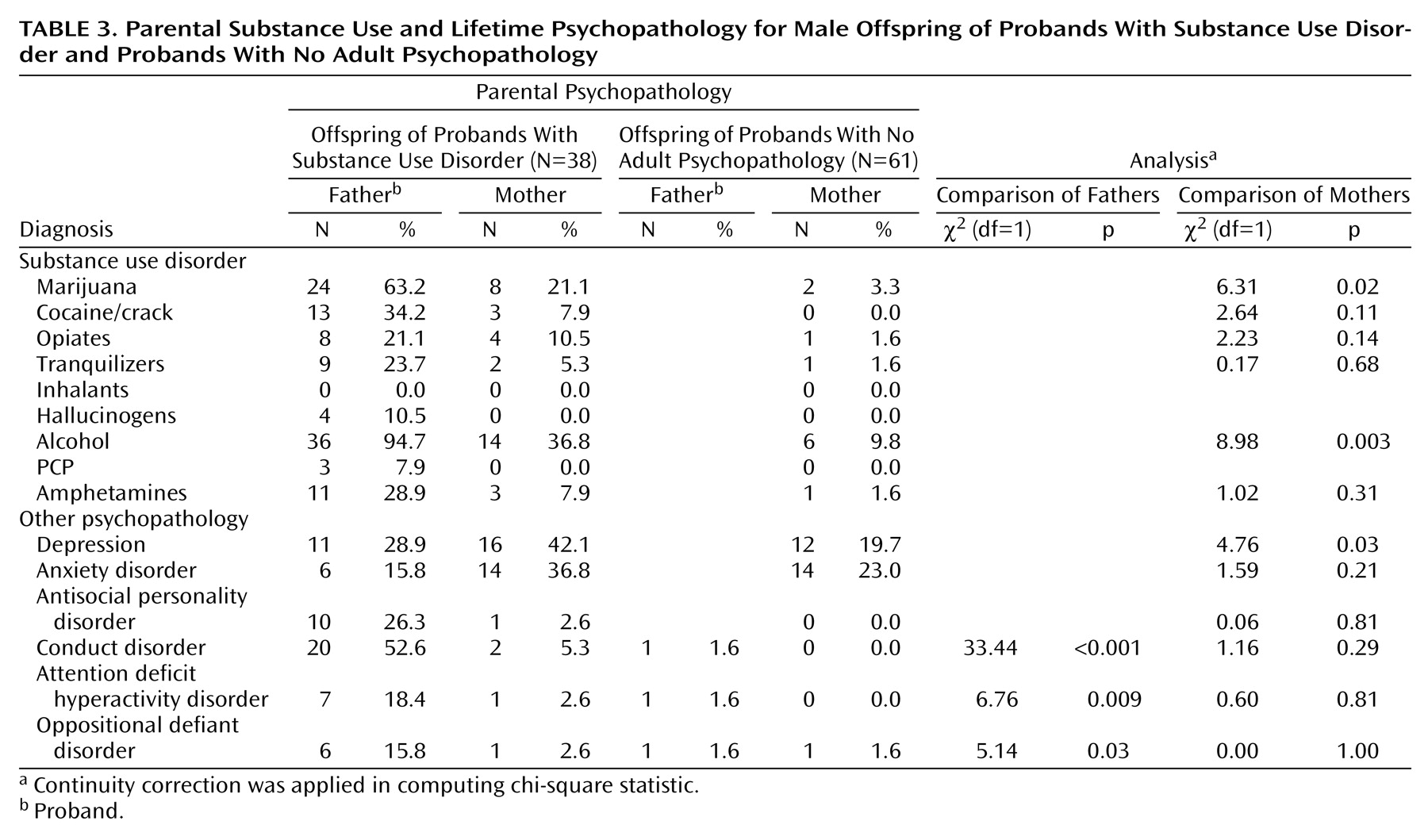
As can be seen in
Table 3, alcohol, marijuana, crack/cocaine, and amphetamines were the most common substance use disorder diagnoses in the parents of the offspring followed in this study. The spouses of the probands with substance use disorder had significantly higher abuse/dependence rates for alcohol and marijuana than did spouses of probands with no adult psychopathology.
Table 3 also summarizes the distribution of psychiatric diagnoses in the probands and spouses in the two groups. As children, probands with substance use disorder had a higher rate of conduct disorder, ADHD, and oppositional defiant disorder than did the probands with no adult psychopathology. The spouses of probands with substance use disorder had a higher rate of depression than did spouses of probands with no adult psychopathology.
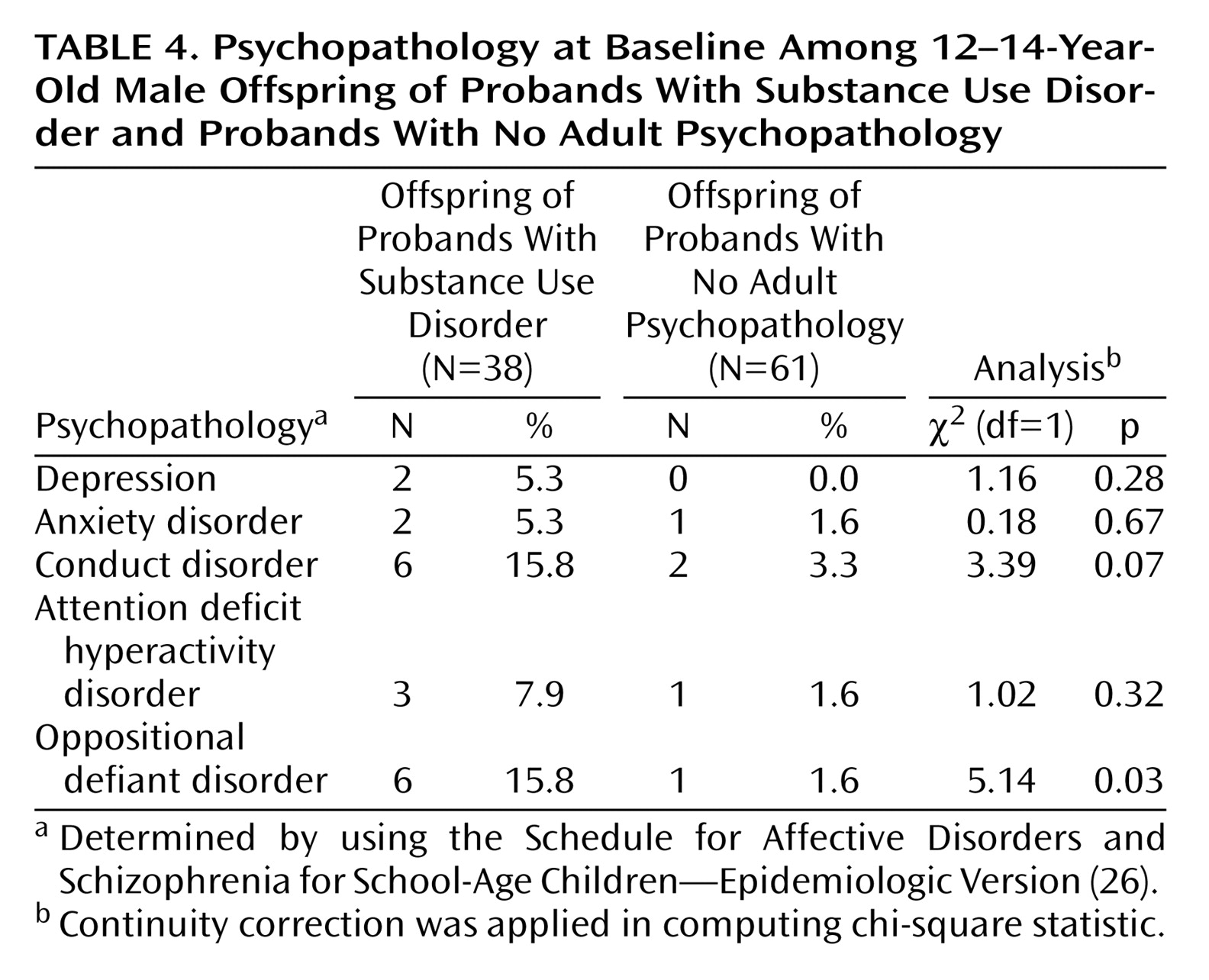
Table 4 documents the rate of offspring psychiatric diagnoses. The offspring of probands with substance use disorder had a significantly higher rate of oppositional defiant disorder compared with the children of probands with no psychopathology and exhibited a higher rate of conduct disorder that did not reach statistical significance.
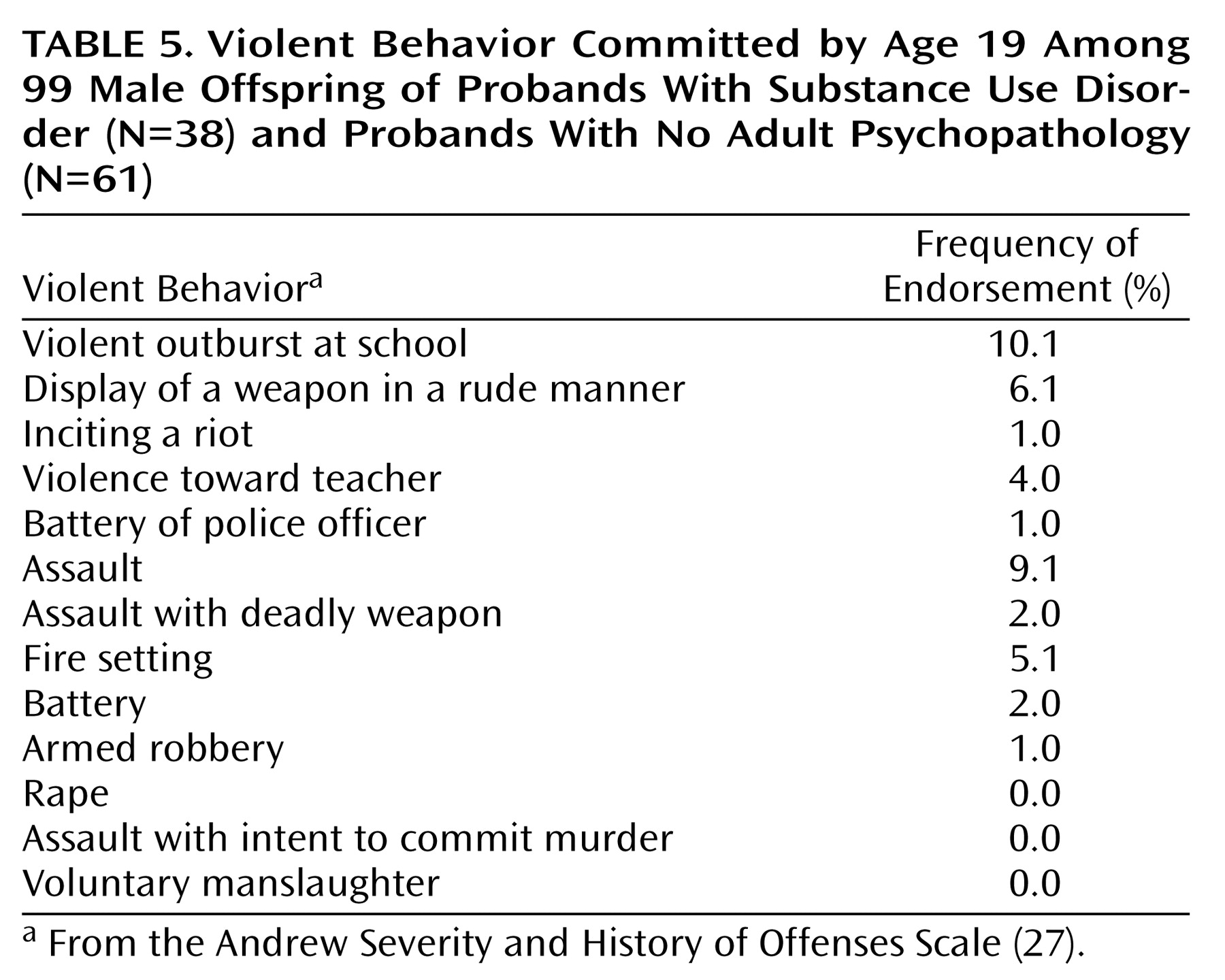
Endorsement of any item from the Andrew Severity and History of Offenses Scale
(27) at 19 years of age was operationally defined as a violent outcome; this was reported in 16% of the subjects. As can be seen in
Table 5, the most common manifestations were violent outburst in school, assault, and displaying a weapon in a rude or offensive manner.
Employing the Cox and Snell test for binary data
(29), it was found that the variables measured at ages 12–14 predicted violent behavior at age 19 (R
2=0.23; χ
2=25.25, df=9, p=0.002).
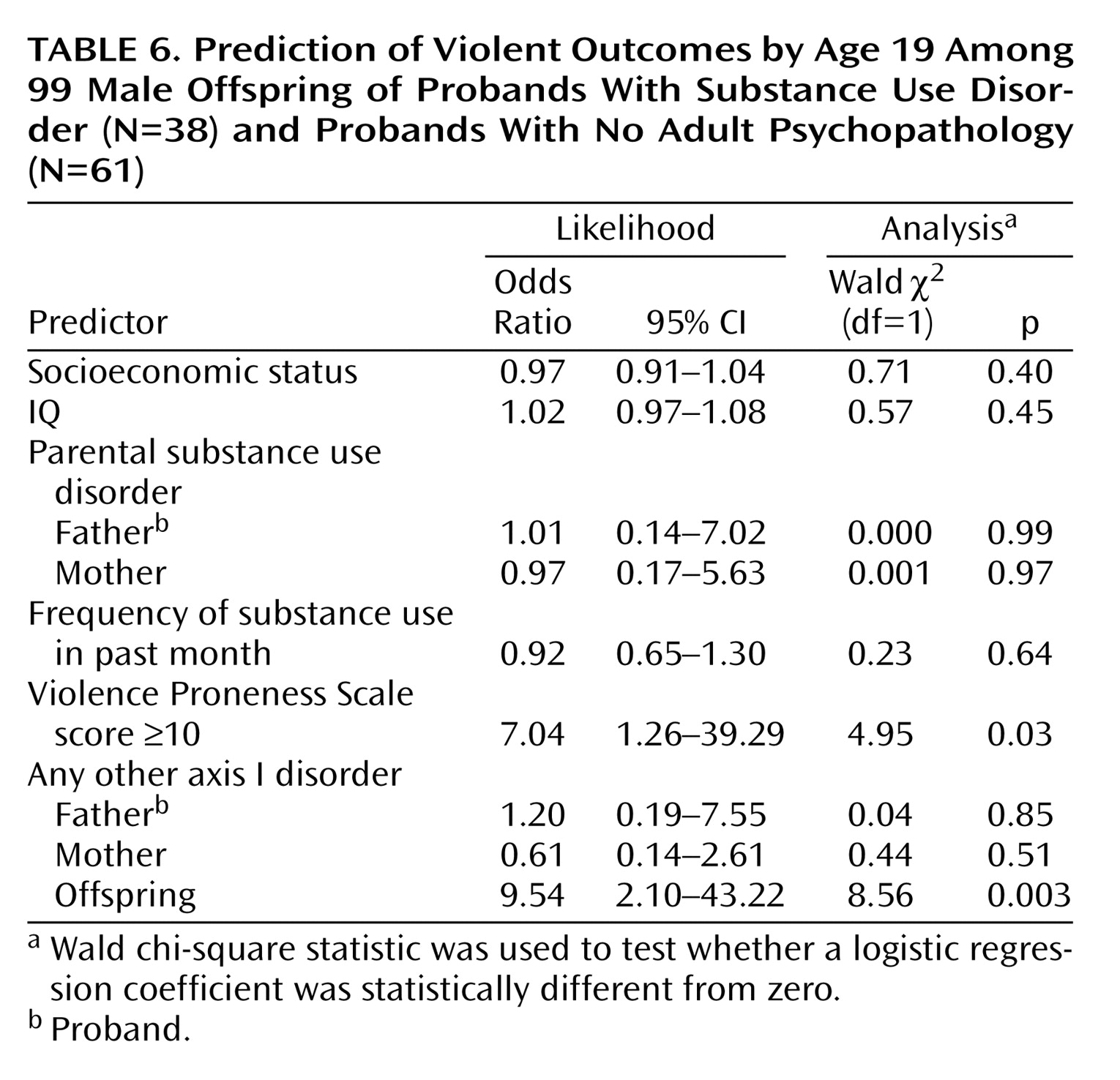
Table 6 summarizes the key findings of the logistic regression analyses. A Violence Proneness Scale score of 10 or higher and an axis I psychiatric disorder in a boy predicted the occurrence of a violent outcome (endorsement of any item in
Table 5) with an overall accuracy of 77% (76/99). Sensitivity was 81% (N=13 of 16), and specificity was 76% (N=63 of 83). The positive predictive value was 39% (N=13 of 33), and the negative predictive value was 95% (N=63 of 66). It should be noted that classification accuracy did not appear to be biased by subjects lost to attrition. A similar proportion of dropouts and remaining subjects (55.1% versus 51.4%) had Violence Proneness Scale scores above the cutoff score of 10 (χ
2=0.43, df=1, p=0.51). The presence of substance use disorder in either parent did not contribute to prediction of violent outcome in their children. In addition, substance use in the prior month among the offspring did not contribute to violence prediction.
Discussion
The main purpose of this study was to determine whether it is feasible to implement an efficient screening method to detect youth who may be at high risk for committing a violent act. Toward this objective, it was observed that a score of 10 or higher on the Violence Proneness Scale significantly predicted violence. Its predictive utility was demonstrated in a 5–7-year follow-up. Overall classification accuracy was 77% when the Violence Proneness Scale was used as a predictor in conjunction with childhood psychiatric history. Substance use disorder in the parents and level of the adolescent’s recent substance use did not significantly predict a violent outcome.
Although overall classification accuracy was good, considering the low prevalence of violence in the population, the more important finding is the capacity of the two significant predictors to identify the true positives, that is, youth who will subsequently commit a violent act. A sensitivity of 81% illustrates the potential of developing an efficient and accurate screening procedure for the detection of youth at high risk for violence.
The three most frequently endorsed items on the Andrew Severity and History of Offenses Scale were “violent outbursts in school” (10.1%), “assault” (9.1%), and “display of a weapon in a rude manner” (6.1%). Thus, the manifestations of violence observed in this study were not merely reflections of social deviancy or disruptive behavior. Rather, the results indicate discrete events that involved actual or potential harm to another person. These outcomes were, however, not independent of childhood psychopathology. The main finding of this study was that psychopathology in conjunction with quality of adjustment in school and with peers resulted in better predictive accuracy than either childhood psychopathology or school and peer contextual factors alone.
It is also noteworthy that the Violence Proneness Scale derived in this study does not directly assess violence inasmuch as the items endorsed do not reflect violence propensity. Rather, as can be seen in
Table 1, the items reflect maladjustment in school and affiliation with deviant peers. The observation that future violence was conjointly predicted by a history of childhood psychiatric disorder indicates that nonnormative behavior and emotion regulation also comprises a salient risk factor for future violence. Of significance is the fact that the manifest psychiatric disorders consisted of both externalizing and internalizing types; these two broad categories of disorders are commonly comorbid. Unfortunately, the study group size was too small to determine whether each type of violence outcome is differentially related to a particular childhood psychiatric disorder. However, it is noteworthy that the findings concur with the results of a recently reported study
(30) demonstrating the importance of academic underperformance, delinquent peers, and externalizing behavior as predictors of adolescent violence. From a large panel of putative risk factors, Herrenskohl et al. observed that youth having five or more risk factors were sevenfold more likely to manifest violence by age 20.
It is important to note that the findings are not based on a random sample of boys but rather youth ascertained from proband fathers who either had substance use disorder or no axis I or axis II psychopathology. This recruitment strategy enabled elucidating the impact of parental substance use disorder and other psychiatric disorders on violence outcome in their offspring. Thus, while the sensitivity and overall classification accuracy of the predictor variables point to the viability of screening youth who may be at high risk for violence, it is nonetheless important to conduct cross-validation on a representative sample of youth before the Violence Proneness Scale can be recommended for routine use.
From the perspectives of both research and prevention practice, it is notable that previous findings have indicated that the school context moderates the genetic predisposition to aggression
(2). Clarifying the quality of interaction between the individual and various facets of the social environment affords the opportunity to design innovative interventions. In this study, psychiatric history and adjustment in the school and peer environment appear to enable superior prediction of violence between early adolescence and young adulthood. It is noteworthy that biobehavioral dysregulation in early childhood is an integral risk factor for subsequent maladjustment
(21). The extent to which this trait, in the context of neighborhood and community environmental factors, predisposes to violence remains to be empirically determined, particularly as it may inform the design of focused preventions for targeted populations.