Depression is a common medical condition, and although it is eminently treatable, it is associated with significant social and functional impairment as well as high direct and indirect health care costs
(1,
2). Estimates of the prevalence of depression vary from 15% to 25% for lifetime prevalence and from 10% to 20% for 12-month prevalence
(3–
8). Depression has been reported to cause greater functional disability than diabetes, chronic lung disease, hypertension, or back pain
(9). The total direct and indirect costs of depression have been estimated to be $44 billion annually in the United States, with annual costs estimated at $5,400 per patient
(10,
11). Within the next 20 years, depression is predicted to become one of the leading causes of disability worldwide—second only to ischemic heart disease in terms of the total cost to society
(12,
13). Although cost estimates depend heavily on the researcher’s perspective, it is generally accepted that the indirect costs of depression outweigh direct costs by a ratio of as much as 7:1
(2,
9–
11,
14–17).
To improve delivery of care for patients with chronic illnesses, Wagner et al.
(26) proposed an evidence-based model that incorporates the following main components: use of evidence-based practice guidelines, practice reorganization to meet the needs of chronically ill patients, patient education, and expert systems or multidisciplinary approaches to care. Similarly, disease management programs included in this review had multiple components such as the use of an evidence-based guideline akin to the Wagner model. We defined disease management as an intervention to manage or prevent a chronic condition by using a systematic approach to care (i.e., evidence-based practice guidelines) and potentially employing multiple treatment modalities
(27). Several studies assessed the effect of single treatment modalities such as psychotherapy on outcomes of patients with depression. However, the effectiveness of multimodal disease management programs has rarely been demonstrated in rigorously designed evaluations, and few descriptions of programs with the goal of improving care for patients with depression have been published. Our study had two objectives: 1) to identify rigorously conducted studies of depression disease management programs and 2) to systematically evaluate the effectiveness of these programs.
Method
Literature Search and Review
We performed a systematic review of the published medical literature to identify studies evaluating the effectiveness of disease management programs in improving care or reducing costs for patients with a variety of common chronic conditions, including depression. In collaboration with a librarian with expertise in searching computerized bibliographic databases, we conducted a search of the MEDLINE, HealthSTAR, and Cochrane databases for English-language articles published between January 1987 and June 2001. The search used the following medical subject headings: patient care team, patient care planning, primary nursing care, case management, critical pathways, primary health care, continuity of patient care, guidelines, practice guidelines, disease management, comprehensive health care, ambulatory care, and the title words “disease state management” and “disease management.” We performed an additional search using the terms “depression” and “randomized controlled trial.” Hand searches of bibliographies from relevant articles and reviews as well as consultations with experts in the field yielded additional references.
Our working definition of disease management was as follows: an intervention designed to manage or prevent a chronic condition by using a systematic approach to care and potentially employing multiple treatment modalities
(27). We defined a systematic approach to care (or guideline) as a set of systematically developed statements to assist practitioners’ and patients’ decisions about appropriate health care for a specific clinical circumstance
(28). To determine if a program incorporated a systematic approach to care, we searched for keywords, including guidelines, protocols, algorithms, quality improvement programs, care plans, and standardized patient and provider education. We excluded programs exclusively evaluating single treatment modalities (e.g., psychotherapy or specific pharmacologic agents) or patients’ compliance with medication regimens. Articles were rejected if they included only pediatric cases, or if they were reviews, case reports, editorials, letters, or abstracts of meeting presentations. Articles were rejected if they did not use acceptable experimental or quasi-experimental study designs as defined by the criteria for acceptable study design of the Cochrane Effective Practice and Organization of Care Group
(29) or if they did not report sufficient information to allow for estimation of at least one measure of a program effect of interest and its variance. Failure to meet this criterion could be due to inadequate reporting of results or to the lack of an appropriate comparison group.
Based on these explicit inclusion and exclusion criteria for titles, abstracts, and articles, two reviewers trained in health services research and the principles of critical appraisal independently reviewed random samples of titles, abstracts, and articles. Interrater agreement was assessed by using the kappa statistic, and reviews were split between reviewers if a sufficient level of agreement was achieved (kappa >0.7). The findings from accepted articles reporting results for depression disease management programs were used to address study objectives.
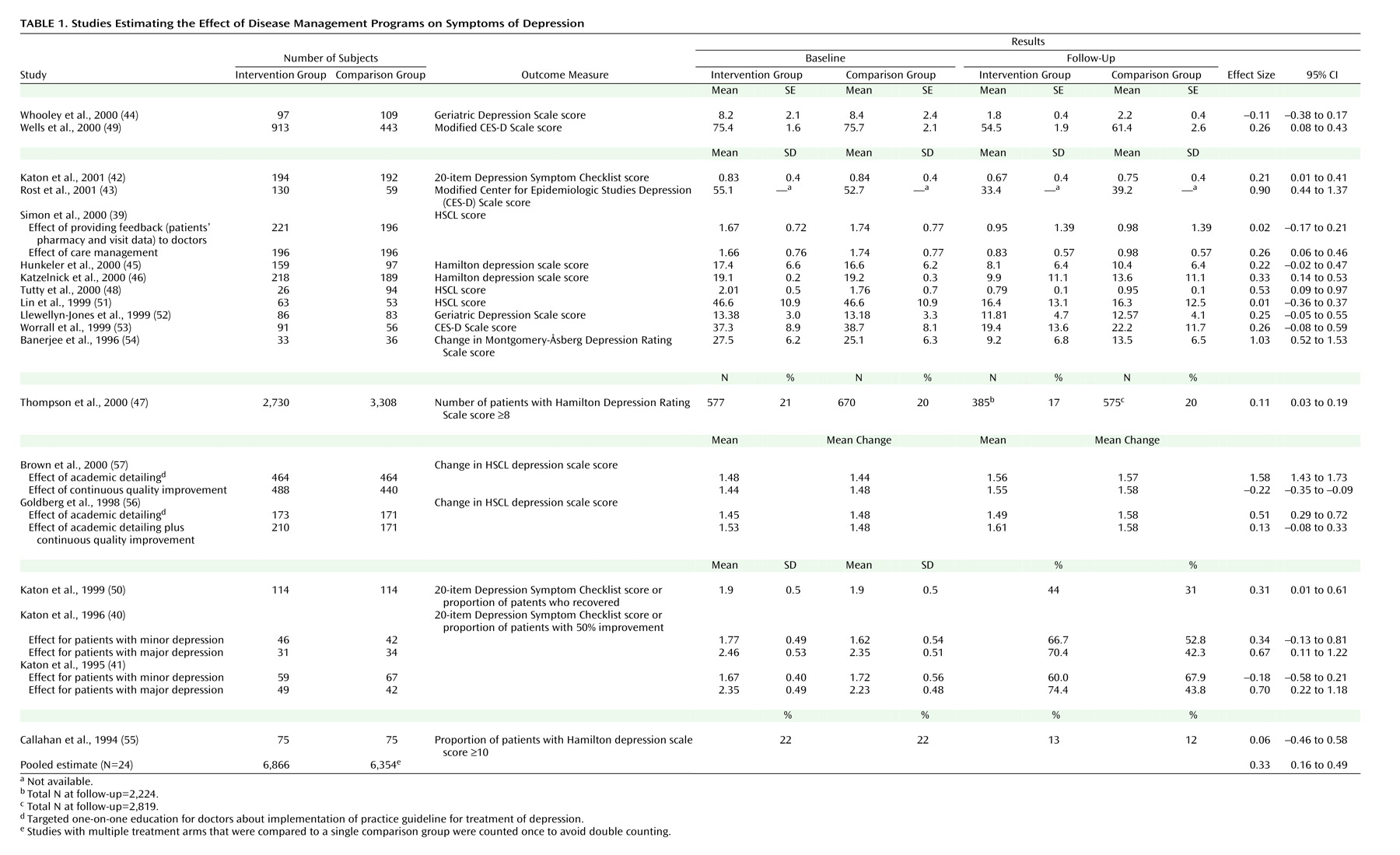
Extraction of Data
By using a standardized abstraction form, data describing study design, population characteristics, sample size, intervention strategies, and processes and outcomes of care were collected from unmasked articles that met the inclusion criteria. Multiple published reports from a single study were treated as a single program evaluation. Studies with multiple intervention arms contributed more than one observation, as did those reporting results in different subgroups of patients.
When appropriate, we used changes from baseline values as opposed to follow-up values in our analyses. Several studies did not report variances for changes from baseline values. In those cases we assumed that the variance for the change was equal to the average of the variances of the baseline and follow-up distributions, if both were given, or, if both were not given, to the variance of the follow-up distribution.
Conceptual Model for Analysis
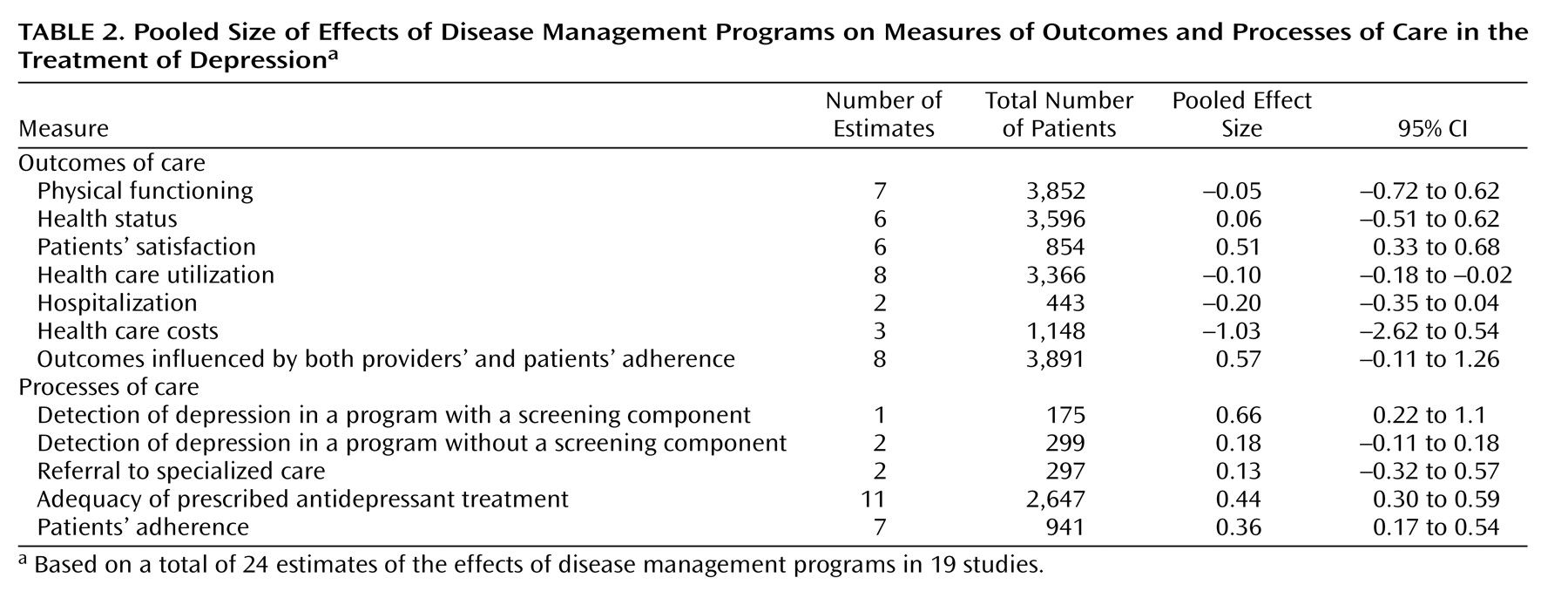
To guide our analysis, we developed a conceptual model of the processes and outcomes of care for patients with depression. We identified available assessments for various processes and outcomes of care by using the following framework: detection of depression → prescribed treatment → patients’ compliance with recommended treatment → treatment outcomes. Outcomes potentially affected by both practitioners’ adherence to guidelines and patients’ compliance (e.g., the proportion of patients taking antidepressant drugs) were analyzed in a separate category.
Meta-Analysis
Effect sizes, defined as a difference between the means of the treatment and control arms divided by the pooled estimate of the standard deviation (continuous variables) or the log odds ratio multiplied by a constant variance term (binary variables)
(30), were calculated for each study outcome to allow pooling of similar outcomes
(31–
35). Effect sizes were constructed such that positive numbers denote benefit.
We used the more conservative, random-effects, empirical Bayesian method of Hedges and Olkin to pool the estimated effects
(35,
36). We pooled results for each category defined by the conceptual model and the additional category reflecting effects influenced by both providers’ and patients’ adherence. When more than one process or outcome result within a category were reported for the same group of subjects, the one associated with the smallest effect size was used. Results are reported as the pooled effect size with the 95% confidence interval (CI) for each group of process/outcome variables.
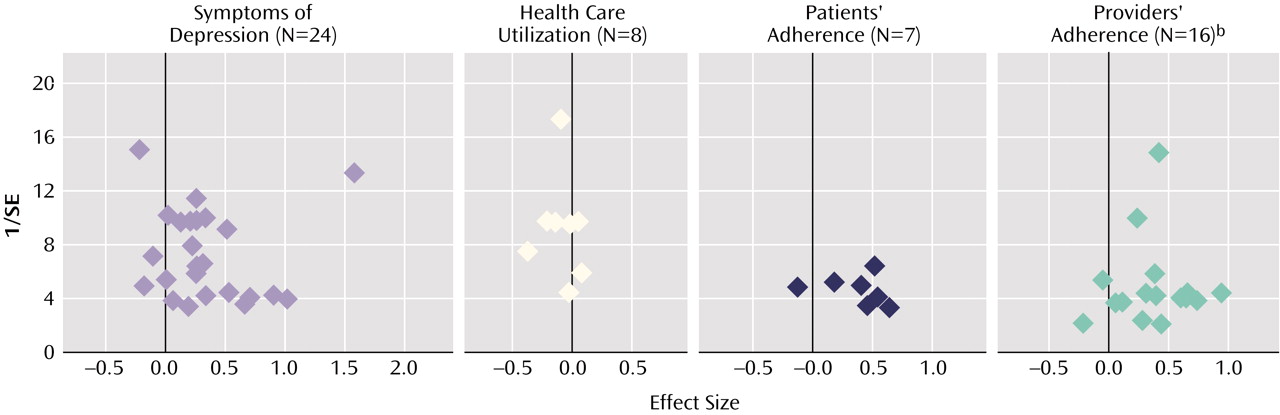
Publication Bias
We explored the evidence for publication bias with funnel plots
(37) for the four areas with at least seven effect estimates
(38). We plotted the effect size on the x-axis by the inverse of its standard error on the y-axis. A plot that is asymmetrical or that has a relative paucity of estimates favoring no treatment with large standard errors (the bottom left region of the graph) suggests publication bias.
Discussion
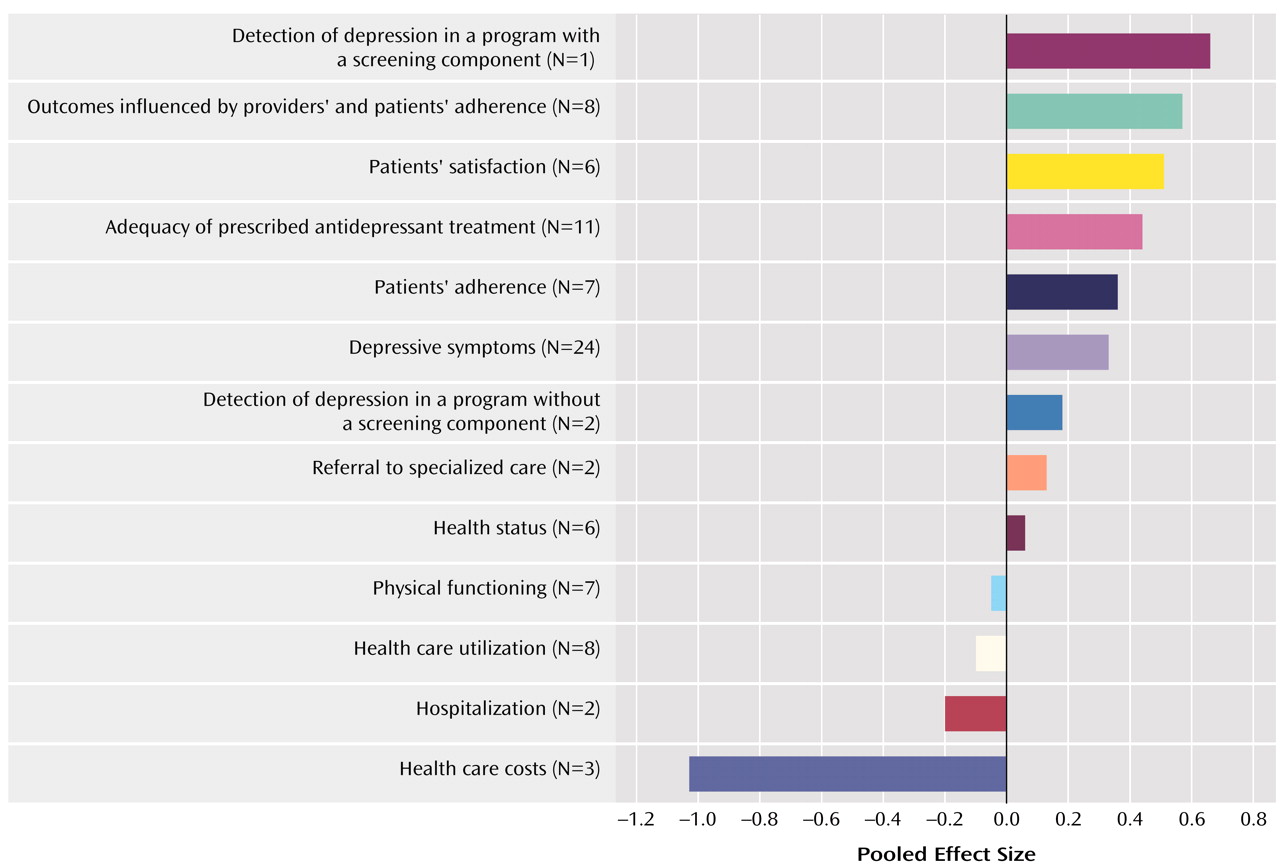
We systematically evaluated and appraised published evaluations of depression disease management programs and found that such programs appear to result in some improvements in both processes and outcomes of care. Pooled results indicated statistically significant improvements in patients’ symptoms of depression, physical functioning, health status, satisfaction of treatment, and adherence to treatment regimens, as well as in the rate of detection of depression, adequacy of treatment with antidepressants, and outcomes that are influenced by both providers’ and patients’ adherence. The largest effect was found in one program with an explicit screening component intended to increase the detection of depression in primary care patients (effect size=0.66).
This large effect is an important finding because 40%–50% of psychiatric disorders in primary care patients are undetected
(24). Several studies that have assessed the effect of structured screening on rates of detection of depression have reported increases in the diagnosis of depression between 10% and 47%, suggesting that screening is effective for identifying depression among primary care patients
(58). Systematic screening has been advocated as a means of improving detection, treatment, and outcomes of depression. Moreover, screening implemented with interventions aimed at increasing recognition and management of depression has been reported to result in favorable outcomes. For example, in one study that implemented screening in combination with quality improvement activities to increase the percentage of patients receiving appropriate care according to national guidelines, the proportion of patients receiving appropriate treatment was higher in the disease management group, compared to usual care
(49).
Even when depression is recognized, diagnosis does not necessarily result in appropriate treatment. In addition to their use in detecting depression among primary care patients, screening tools can also be used to establish thresholds for treatment initiation. Incorporating structured screening into disease management programs is likely to lead to increases in the detection and management of depression in the primary care setting.
Improved detection and treatment may increase costs to the extent that they result in more medications being prescribed and more visits to health care providers. Such increases are reflected in our pooled analysis. We found that disease management programs resulted in increases in measures of health care utilization, such as the number of primary care visits, the cost of treatment, and the number of hospitalizations for depression (
Figure 1). Potential cost savings resulting from improved treatment, such as reductions in nonpsychiatric health care costs and improvements in productivity, were not evaluated in the studies we identified.
To assist our analysis, we developed a conceptual model to describe key aspects of depression care such as detection, prescription of appropriate treatment, and patients’ compliance with treatment. These key domains represent potential targets for disease management interventions in addition to broader efforts in system reorganization. Treatment success, defined as improvement in symptoms and reduction of impairments in functional status, depends on the providers’ ability to recognize depression and prescribe appropriate treatment, as well as the patients’ adherence to prescribed treatment.
Some measures, such as the quantity of medication taken by patients, are potentially affected both by providers’ adherence to treatment guidelines and by patients’ adherence to treatment recommendations, since medications must be prescribed in order to be taken. We grouped together outcomes influenced by both providers’ and patients’ adherence, as well as examined them separately. The pooled result showed a statistically significant positive effect of disease management programs on this group of measures. This improvement could result from program effects on providers’ treatment patterns, on patients’ compliance with prescribed treatments, or both. The pooled estimate of program effect on measures of providers’ adherence (i.e., measures of adequacy of prescribed treatment) was slightly higher (effect size=0.44) than the pooled effect on measures of patients’ compliance (effect size=0.36). These results suggest that disease management programs can improve both providers’ adherence and patients’ compliance. Similar findings were reported in a study by Weingarten et al.
(59) that examined the effect of disease management interventions on the processes and outcomes of care among patients with chronic conditions.
Few studies evaluated the effects of multicomponent interventions on providers’ satisfaction. One study assessed the effect of a new clinical system of care for elderly patients and found that providers in the intervention group reported being “very satisfied” with the management of patients participating in the study
(60). However, studies measuring the relationship between providers’ satisfaction and the rate of adherence to practice guidelines were not identified. Future research should focus on the development of appropriate measures to assess providers’ satisfaction with disease management programs and explore whether an association exists between the rate of adherence to practice guidelines and providers’ satisfaction.
While our study has several strengths, it has some limitations. Our definition of disease management, based on a published definition
(27), was established a priori; however, disease management is a broad term, and its definition depends on the perspective employed. Our results may be subject to different interpretations, according to the operational definition of disease management.
The studies we identified may not be representative of all evaluations of depression disease management programs. Results from disease management programs implemented by health plans or disease management organizations may not be published for a variety of reasons, including negative findings, competitive or proprietary concerns, lack of expertise in publishing research studies, or a paucity of funding to support submission of programmatic results to peer-reviewed journals. Studies demonstrating statistically significant benefits, particularly small ones, may be more likely to be published than studies with nonsignificant or negative results. Examination of the funnel plots in this study suggested that such publication bias has, in fact, occurred to some extent.
In addition to using qualitative evaluation of disease management, we used effect sizes as a common metric to assess the magnitude of the effect of disease management across studies with different processes and outcomes of care. Some researchers have attempted to develop parameters to assist in interpreting effect sizes. We used the convention of Kazis et al.
(61), in which an effect size less than 0.6 is considered a “small effect” and an effect size between 0.6 and 1.2 is characterized as a “moderate” effect. In our study, most effect sizes were less than 0.6, including those for program effects on depressive symptoms, patients’ satisfaction, treatment adequacy, and patients’ adherence with recommended treatment.
Finally, disease management is in an early stage of evolution. Although population-based approaches to care have existed for quite some time, the mechanisms for implementation (e.g., technologies, strategies to change physicians’ and patients’ behavior, and assessment methods) are still evolving. Thus, the effectiveness of disease management in depression may change over time, particularly when it is implemented in broader patient populations and in less controlled settings. Effectiveness may increase as implementation strategies are refined and improved.
As with other chronic and relapsing illnesses, depression is a condition for which results may depend on the therapeutic alliance that results when the patient and a team of providers participate in treatment. It has been suggested that depressed patients benefit most when interactions with their providers are recurrent and varied; the ultimate purpose and length of these visits are less important than their frequency. Disease management programs may improve outcomes of treatment by fostering a structured treatment environment in which such therapeutic alliances can be forged more readily.
Disease management programs can improve quality of care and outcomes for patients with depression, as reflected in improvements in measures of both processes and outcomes of care. However, such programs also increase treatment costs. Although investment of resources may be required to achieve improved outcomes for patients, potential cost savings could result in other areas, such as other health care utilization and employee productivity.