Family, twin, and adoption studies
(1–
4) have demonstrated the role of genetic factors in the etiology of schizophrenia. Relatives of patients with the disorder not only have higher than normal rates of schizophrenia but also have higher rates of disorders related to schizophrenia, including schizoaffective disorder, schizotypal personality disorder, and paranoid personality disorder
(1,
5).
Studies across numerous medical disorders
(6) indicate that patients with an early onset may represent a more homogeneous subgroup of patients with more salient familial etiological factors. Two early studies of schizophrenia suggested that patients with early onset of the disorder may indeed have higher rates of family psychopathology. In a report on the first, Kallmann and Roth noted that “there must be some factor or combination of factors which in some cases leads to clinically recognizable symptoms at an unusually young age”
(7, p. 599). Theirs is the only major twin study of childhood-onset schizophrenia of which we are aware, and they found an uncorrected concordance rate for monozygotic twins of 88.2% and a concordance rate for dizygotic twins of 22.8%
(7). Later, in a series of landmark papers in 1971, Kolvin et al.
(8,
9) noted a high rate of social isolation (60% of mothers), introversion (50% of parents), and suspiciousness (42%) in parents of patients with childhood-onset schizophrenia, all higher than the rates seen in parents of children with autism. Parents of patients with childhood-onset schizophrenia had a rate of schizophrenia (10.4%) similar to that reported for parents of patients with adult-onset schizophrenia
(8).
Asarnow and colleagues
(10) reported what appears to be the first published family study of childhood-onset schizophrenia using modern diagnostic methods. They found that relatives of probands with childhood-onset disease had higher rates of schizophrenia spectrum disorders than seen for relatives of children and adolescents with attention deficit hyperactivity disorder and for relatives of community comparison subjects. Although that study did not directly compare relatives of patients with childhood-onset and adult-onset schizophrenia, the relative risk of a schizophrenia spectrum disorder among parents of patients with childhood-onset illness was greater than that found in other family studies of adult-onset schizophrenia, in keeping with the hypothesis of a greater familial vulnerability in illness with a very early onset
(11–
13). As Asarnow et al.
(10) noted, however, comparing rates of disorders in different studies is fraught with difficulties.
As part of an ongoing study of childhood-onset schizophrenia at the National Institute of Mental Health (NIMH), parents were evaluated for the presence of psychopathology, as were parents of adults with schizophrenia and parents of unselected comparison subjects from the community. The purpose of this study was to confirm and extend the findings of Asarnow and colleagues
(10). We hypothesized that parents of patients with childhood-onset schizophrenia would have higher rates of schizophrenia and related spectrum disorders than parents of community comparison subjects. Further, we hypothesized that the parents of these patients with very-early-onset illness would have higher rates of schizophrenia spectrum disorders than parents of patients with adult-onset schizophrenia.
Method
Subjects
As of September 2000, 54 children and adolescents had participated in a comprehensive study of childhood-onset schizophrenia
(14,
15). Patients were recruited through an extensive screening process, including a review of over 1,000 charts and in-person screening of over 230 subjects. The 54 patients who participated were diagnosed with schizophrenia according to DSM-III-R or DSM-IV criteria and had an onset of psychosis before age 12. The diagnosis was made through an extensive screening process, including the use of the Schedule for Affective Disorders and Schizophrenia for School-Age Children
(16).
To assess the presence of parental axis I and II disorders, parents of each of these patients were interviewed in person by using the Schedule for Affective Disorders and Schizophrenia (SADS)
(17) and the Structured Interview for DSM-IV Personality Disorders
(18). Of the 97 parents interviewed in person, two were nonnative speakers of English. Because an interpreter was unavailable, the validity of their results, particularly those from the Structured Interview for DSM-IV Personality Disorders, was unclear, and for that reason these two parents were excluded. For parents who were unavailable, attempts were made to obtain diagnostic information by interviewing the other parent with the same instruments. Using this family history interview method, we obtained adequate information on a further two parents, while insufficient information was available for nine parents (one patient had been adopted shortly after birth, information on an additional seven fathers lacked the detail necessary for a valid assessment of their mental health status). Sufficient data was, therefore, available for 97 parents of patients with childhood-onset illness.
Parents of 54 adults with schizophrenia who were involved in other medication or family studies at NIMH
(19) also participated in this study. The probands in these studies had been diagnosed with schizophrenia by means of the Structured Clinical Interview for DSM-IV
(20). The mean age at onset for 32 of these patients was 21.6 years (SD=3.8); age at onset was not available for the remainder. Parents of these patients who were available and willing to participate in the present study were interviewed by means of the SADS and the Structured Interview for DSM-IV Personality Disorders. Apart from being the parent of a patient with rigorously defined schizophrenia, there were no inclusion or exclusion criteria. These parents were not specifically matched with the parents of the patients with childhood-onset illness on demographic variables. Eighty-six parents were interviewed in person. As with the parents of the patients with childhood-onset schizophrenia, attempts were made to interview the available parent about the other parent, if unavailable, by means of the SADS and Structured Interview for DSM-IV Personality Disorders. For 11 of the 22 parents not seen in person, adequate data could be attained through family history interview. Therefore, usable data were obtained for 97 parents of adult patients with schizophrenia.
Finally, a comparison group of parents of 84 children and adults was recruited through flyers, newspaper advertisements, and word of mouth. These parents and their children were not screened for the presence of a personal or family history of psychiatric disorders, and among those calling to participate, none was excluded. None of the children of these parents had schizophrenia or any other psychotic disorder. These parents were also interviewed with the SADS and the Structured Interview for DSM-IV Personality Disorders. Of the volunteers, 123 parents were interviewed in person. Diagnostic information was obtained on a further six through family history interview, again with the SADS and Structured Interview for DSM-IV Personality Disorders. In total, data were obtained regarding 129 parents of comparison subjects.
As the vast majority of the siblings of the patients with childhood-onset schizophrenia had not reached 18 at the time of this study (many were still under age 10), data on the siblings are not included.
This study was approved by the NIMH institutional review board. All of the parents who were interviewed provided written consent.
Interviews
The interviews were all completed by a physician (R.N. or another physician) or a research social worker (M.L.) who was not blind to group membership. All interviewers had experience in using semistructured interviews. Because of time constraints, a number of parents of patients with adult-onset schizophrenia (N=21) and comparison subjects (N=31) and one parent of a patient with childhood-onset illness were not assessed for schizoid personality disorder. The transcribed interviews were scored by a psychologist (F.B.), who was unaware of subject identity. As an internal check on the reliability of the blinded scoring of this data, a second psychologist (L.J.I.) also blindly scored a portion of the interviews (N=46). The reliability of the two interviewers for the presence or absence of a schizophrenia spectrum disorder was high (kappa=0.96). The scoring of the interviews by the first blinded psychologist showed a high level of reliability in relation to the diagnoses obtained by the interviewers themselves (kappa ranged from a high of 1.00, for the presence of schizophrenia, to a low of 0.74, for the presence of schizoid personality disorder). For the presence of any schizophrenia spectrum disorder, the reliability of the blinded interviewer, in relation to the original interviewers, was 0.90.
For the purposes of this study, we used a narrow definition of the schizophrenia spectrum, which included schizophrenia, schizoaffective disorder, other nonaffective psychotic disorders, schizotypal personality disorder, and paranoid personality disorder. Diagnoses within the schizophrenia spectrum were defined hierarchically
(21), with the hierarchy being ordered as in the preceding list. When a subject received several diagnoses, only the highest in the hierarchy was used, and that subject then was censored from the calculation of rates of disorders lower in the hierarchy.
Statistical Analysis
The three parent groups were compared on demographic variables by means of chi-square analyses and one-way analyses of variance with least significant differences post hoc testing or pairwise chi-square tests. Lifetime morbid risks for the schizophrenia spectrum disorders (defined here as schizophrenia, schizoaffective disorder, other nonaffective psychosis, schizotypal personality disorder, paranoid personality disorder) and for schizoid personality disorder were determined by using the Kaplan-Meier method of analyzing life tables from SPSS (Chicago, SPSS). The age at onset for personality disorders was set at 18. Differences between groups in life table curves for individual schizophrenia spectrum disorders and for any spectrum disorder were analyzed by using the pairwise log-rank chi-square statistic. Using this method, we were able to compare each group to each of the other two parent groups.
The groups were also compared with respect to the number of schizotypal and paranoid symptoms. As the distribution of symptom numbers was highly skewed, this comparison was done by using a Kruskal-Wallis H test. When a significant difference was found, post hoc pairwise testing was performed by means of a Mann-Whitney U test.
Unfortunately, the age at onset of mood disorders and substance use disorders could not be determined for a number of parents of patients with adult-onset schizophrenia and parents of community comparison subjects. In order to assess the morbid risk for these disorders, we therefore instead used the abridged Weinberg method
(22). For this, the age of 40 was taken as the upper limit of the age of risk for major depressive disorder, bipolar disorder, and substance use disorders. Once the age-corrected group sizes were calculated, the three groups were compared on the morbid risk for these disorders by using chi-square tests.
All analyses were performed by using SPSS 10.0 with a significance level of 0.05. Although there was prior evidence for a greater risk for schizophrenia spectrum disorders in parents of both patients with childhood-onset and patients with adult-onset schizophrenia than in community comparison subjects and limited evidence for higher rates of such disorders in relatives of patients with childhood-onset illness than in relatives of those with adult-onset schizophrenia
(10), we chose to use the more conservative two-tailed p values in all comparisons.
Results
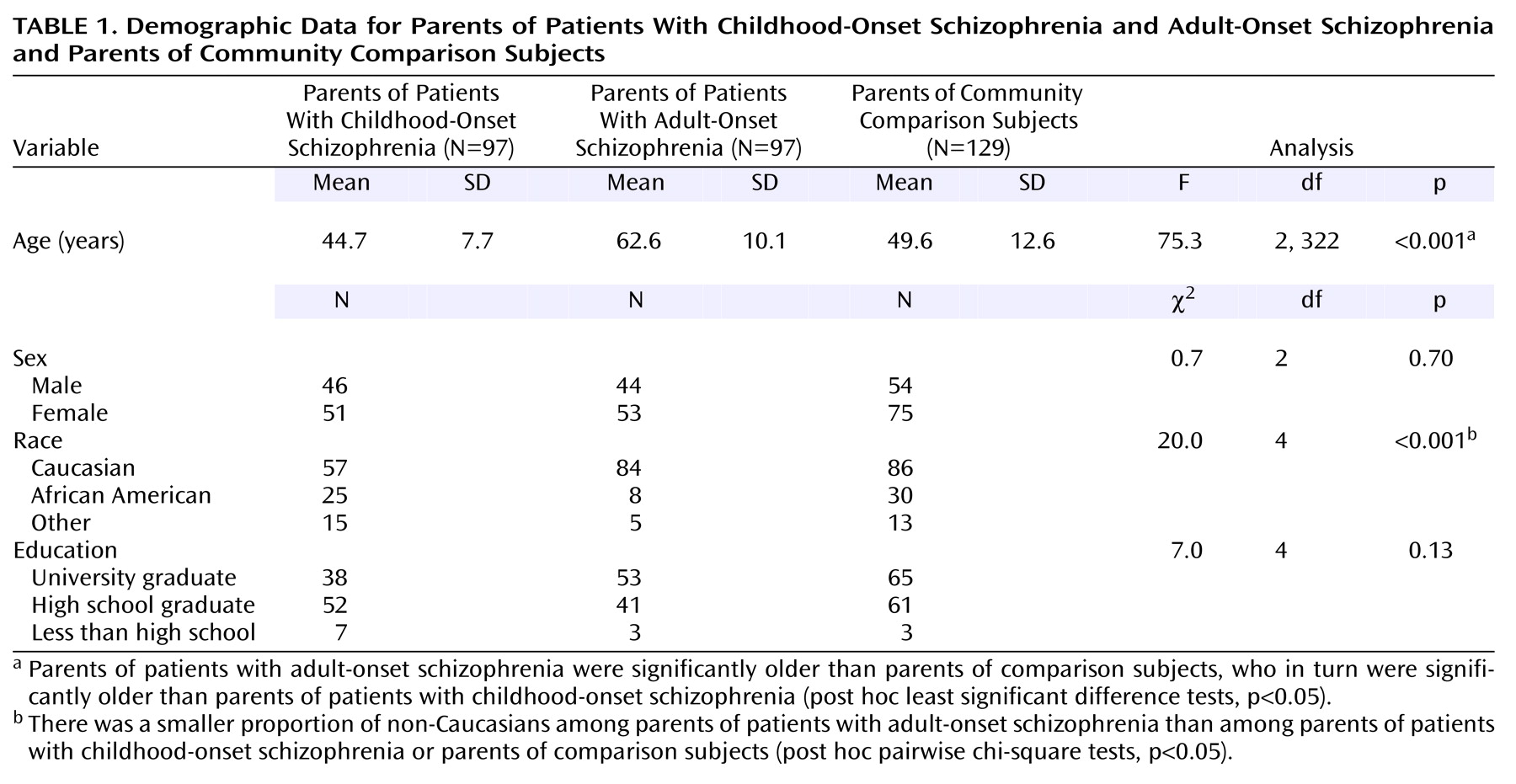
Demographic data for the three subject groups are presented in
Table 1. As expected, the parents of the patients with adult-onset schizophrenia were significantly older than the parents of the community subjects, who in turn were older than the parents of patients with childhood-onset illness. The parents of the patients with adult-onset illness had fewer non-Caucasian group members than the other groups. There were no other significant differences in terms of the demographic makeup of the three groups.
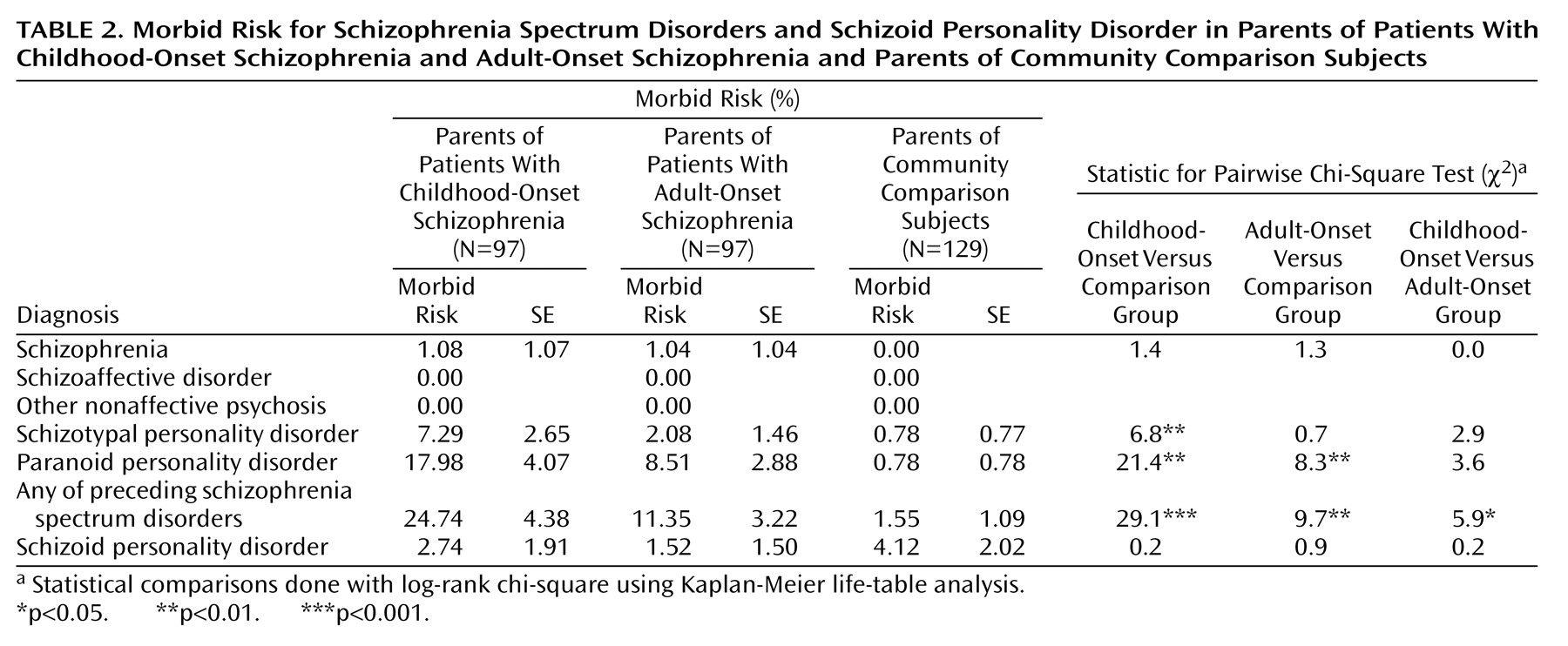
Schizophrenia was an uncommon diagnosis in these groups of parents; only one parent of a patient with childhood-onset schizophrenia and one parent of a patient with adult-onset illness received that diagnosis (
Table 2). No parents in any of the three groups received a diagnosis of either schizoaffective disorder or other nonaffective psychotic disorder.
There were significant group differences among the different personality disorders. Parents of patients with childhood-onset schizophrenia had a greater morbid risk for schizotypal personality disorder than parents of comparison subjects, who did not differ significantly from parents of patients with adult-onset illness. Parents of both patient groups had a significantly higher morbid risk for paranoid personality disorder than the comparison parents but did not differ from each other. The three groups did not differ significantly in the morbid risk for schizoid personality disorder. However, when the five disorders considered here as the schizophrenia spectrum (schizophrenia, schizoaffective disorder, other nonaffective psychotic disorder, schizotypal personality disorder, and paranoid personality disorder) were combined, the parents of the patients with childhood-onset schizophrenia had a greater morbid risk for schizophrenia spectrum disorders than did the parents of patients with adult onset; both of these parent groups had greater morbid risks for schizophrenia spectrum disorders than did the parents of the comparison subjects.
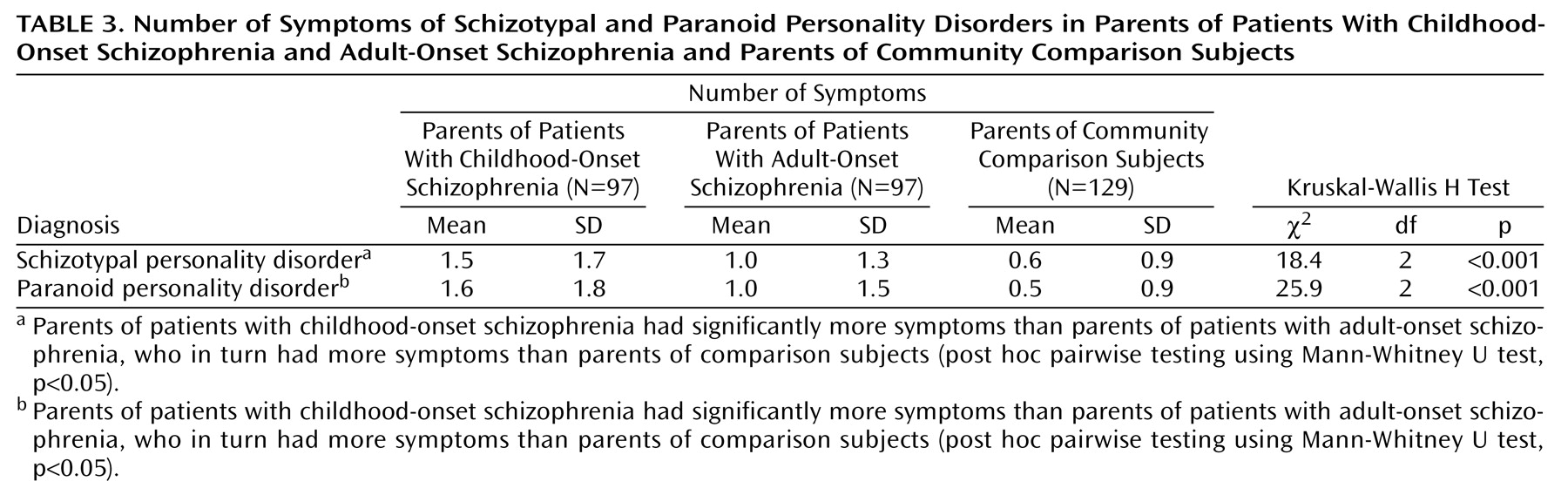
The three groups of parents also differed with respect to the number of symptoms of schizotypal personality disorder and paranoid personality disorder (
Table 3). The parents of the patients with childhood-onset schizophrenia had more symptoms of these personality disorders than did the parents of the patients with adult onset, who in turn had more symptoms of these disorders than did the parents of the comparison probands.
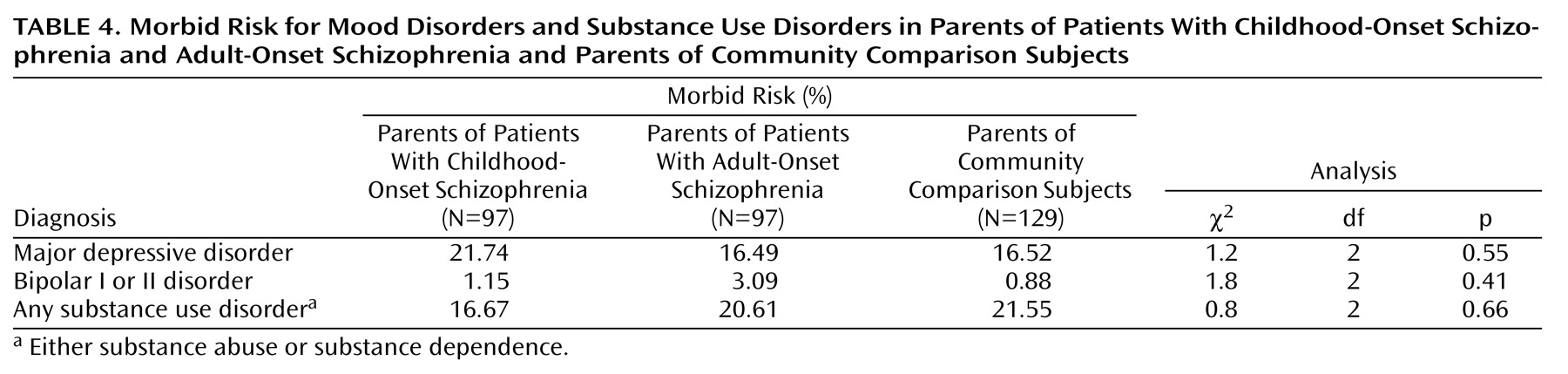
The three groups did not differ significantly in their morbid risks for major depressive disorder, bipolar disorder, or substance use disorders (
Table 4).
When only the parents who had been interviewed in person were included in the statistical analysis, the pattern of results was essentially the same.
Discussion
As expected, parents of patients with childhood-onset schizophrenia and parents of patients with adult-onset schizophrenia had higher morbid risks of schizophrenia spectrum disorders than parents of community comparison subjects. Further, the parents of the childhood-onset patients had a greater risk of schizophrenia spectrum disorders than did parents of patients with adult-onset illness. As well, the parents of the early-onset patients had more symptoms of the personality disorders associated with schizophrenia (schizotypal personality disorder and paranoid personality disorder) than did the parents of adult-onset patients. The groups did not differ in terms of mood disorders, substance use disorders, or the one non-schizophrenia-spectrum personality disorder assessed (schizoid personality disorder).
These findings support and extend the results of the recent study by Asarnow and colleagues
(10), which showed higher rates of schizophrenia spectrum disorders in relatives of patients with childhood-onset schizophrenia than in relatives of subjects with attention deficit hyperactivity disorder and relatives of community comparison subjects. This result is qualitatively similar to that seen for adult patients with schizophrenia and provides further evidence of continuity between the childhood-onset and adult-onset forms of the disorder.
To our knowledge, this is the first study to directly compare parents of adult-onset patients and childhood-onset patients with respect to family psychopathology. The greater morbid risk for schizophrenia spectrum disorders among the parents of the childhood-onset patients supports the hypothesis that schizophrenia with a very early onset is associated with a greater familial vulnerability for the disorder. The finding of higher numbers of schizotypal and paranoid symptoms among parents of patients with childhood-onset schizophrenia indicates that the results of this study represent a general shift in symptom dimensions and are not merely an artifact of the arbitrary setting of a minimum number of symptoms for both disorders in DSM-IV.
As in most family studies of schizophrenia, the rates of mood disorders, substance use disorders, and schizoid personality disorder did not differ among the three groups. This suggests that childhood-onset schizophrenia is associated with a specific elevation in familial rates of schizophrenia spectrum disorder rather than an elevation in psychopathology in general.
At first glance, the rates of the schizophrenia spectrum disorders in the parents of these patients may appear high relative to those seen in other studies. However, most family studies of schizophrenia have included both parents and siblings, which might mask differences between these groups of relatives. As schizophrenia is associated with a lower fertility rate
(23), the low rate of schizophrenia in the parents of patients here is likely due to the fitness effects associated with parenthood
(24). The rates of schizophrenia in the two parent groups may also reflect an ascertainment bias toward healthier parents: participation in studies at NIMH requires that parents be able to travel to the Washington, D.C., area, thereby excluding most parents with severe mental illnesses. Within the study of childhood-onset schizophrenia, there have been several patients who were not able to participate because of severe psychopathology in a parent that rendered them unable to travel. The rates of schizophrenia in the parent groups are not dissimilar from the rate of schizophrenia in parents of schizophrenic probands in the Roscommon study
(25), in which parents of patients had lower rates of schizophrenia than siblings of patients but higher rates of schizophrenia spectrum personality disorders
(26).
The results of this study must be viewed as preliminary because of several limitations. The most significant limitation is the manner in which the data were collected. Although the interviews were scored by raters blind to identity (and the ratings of the two blinded scorers showed high reliability), the interviews were completed with the knowledge of the subject’s identity, which may have introduced a bias. As well, the number of subjects was relatively small, necessitated in part by the rarity of childhood-onset schizophrenia
(27). National studies such as the present study of childhood-onset schizophrenia are biased toward involvement of relatively healthy parents because of logistical factors, such as travel to the National Institutes of Health. However, most of the parents of the adult-onset patients in this study were also from outside the Washington area, indicating similar biases in both groups of parents of patients. As well, neither the parents of the community comparison subjects nor the parents of the adult patients were ascertained randomly. In particular, only parents of adult-onset patients who traveled to the National Institutes of Health and were willing to participate were included. However, the rates of schizophrenia spectrum disorders in the parents of adult-onset patients were similar to those seen in parents of schizophrenic patients in other family studies of schizophrenia
(25,
26). In addition, the rates of psychiatric disorders, including schizophrenia spectrum disorders, among the comparison parents were similar to those seen in relatives of comparison subjects in other, much larger studies, suggesting that the parents of the comparison subjects are representative of the general population. The use of parents and not siblings may have resulted in results that do not reflect the whole family. Siblings of these patients were not included as none had passed through the age of risk for schizophrenia, and the vast majority had not even entered the age of risk. However, preliminary data
(28) suggest that the adult siblings of the childhood-onset patients in this cohort also have a high rate of schizophrenia spectrum disorders.
In conclusion, parents of patients with childhood-onset schizophrenia have a higher rate of schizophrenia spectrum disorders than do parents of patients with adult-onset illness, suggesting that a very early onset of the disorder is associated with greater familial vulnerability. Genetic studies of these patients and their families may be particularly informative in uncovering genes involved in the etiology of schizophrenia.